Abstract
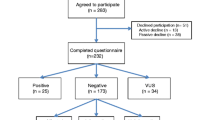
In a sample of individuals with ovarian cancer, we aimed to (a) identify factors associated with the psychosocial impact of genetic counseling and multigene panel testing, (b) identify factors associated with cancer genetics knowledge, and (c) summarize patient-reported recommendations to improve the genetic counseling and multigene panel testing process. Eligible participants in this secondary analysis of quantitative and qualitative survey data were English-speaking adults with ovarian cancer. Psychosocial impact was assessed using the Multidimensional Impact of Cancer Risk Assessment (MICRA) questionnaire. Knowledge of cancer genetics was assessed using the KnowGene scale. Significant predictors of MICRA and KnowGene scores were identified using multiple regression. Open-ended survey item responses were analyzed using conventional content analysis. Eighty-seven participants met eligibility criteria. A positive genetic test result was associated with greater adverse psychosocial impact (B = 1.13, p = 0.002). Older age (B = − 0.07, p = 0.044) and being a member of a minority racial or ethnic group (B = − 3.075, p = 0.033) were associated with lower knowledge, while a personal history of at least one other type of cancer (B = 1.975, p = 0.015) was associated with higher knowledge. In open-ended item responses, participants wanted clinicians to assist with family communication, improve result disclosure, and enhance patient and family understanding of results. A subset of individuals with ovarian cancer who receive a positive genetic test result may be at risk for adverse psychosocial outcomes. Tailored cancer genetics education is necessary to promote the equitable uptake of targeted ovarian cancer treatment and risk-reducing therapies. Interventions to enhance patient-clinician communication in this setting are a research priority.
Similar content being viewed by others
References
Pennington KP, Walsh T, Harrell MI, Lee MK, Pennil CC, Rendi MH, Thornton A, Norquist BM, Casadei S, Nord AS, Agnew KJ, Pritchard CC, Scroggins S, Garcia RL, King MC, Swisher EM (2014) Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas. Clin Cancer Res 20(3):764–775. https://doi.org/10.1158/1078-0432.CCR-13-2287
Walsh T, Casadei S, Lee MK, Pennil CC, Nord AS, Thornton AM, Roeb W, Agnew KJ, Stray SM, Wickramanayake A, Norquist B, Pennington KP, Garcia RL, King MC, Swisher EM (2011) Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing. Proc Natl Acad Sci USA 108(44):18032–18037. https://doi.org/10.1073/pnas.1115052108
Alsop K, Fereday S, Meldrum C, deFazio A, Emmanuel C, George J, Dobrovic A, Birrer MJ, Webb PM, Stewart C, Friedlander M, Fox S, Bowtell D, Mitchell G (2012) BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol 30(21):2654–2663. https://doi.org/10.1200/JCO.2011.39.8545
Lancaster JM, Powell CB, Chen LM, Richardson DL, Committee SGOCP (2015) Society of Gynecologic Oncology statement on risk assessment for inherited gynecologic cancer predispositions. Gynecol Oncol 136(1):3–7. https://doi.org/10.1016/j.ygyno.2014.09.009
National Comprehensive Cancer Network (2020) Genetic/familial high-risk assessment: breast and ovarian: National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf.
Colas C, Golmard L, de Pauw A, Caputo SM, Stoppa-Lyonnet D (2019) Decoding hereditary breast cancer: benefits and questions from multigene panel testing. Breast 45:29–35. https://doi.org/10.1016/j.breast.2019.01.002
Song H, Dicks EM, Tyrer J, Intermaggio M, Chenevix-Trench G, Bowtell DD, Traficante N, Group A, Brenton J, Goranova T, Hosking K, Piskorz A, van Oudenhove E, Doherty J, Harris HR, Rossing MA, Duerst M, Dork T, Bogdanova NV, Modugno F, Moysich K, Odunsi K, Ness R, Karlan BY, Lester J, Jensen A, Krüger Kjaer S, Høgdall E, Campbell IG, Lázaro C, Pujara MA, Cunningham J, Vierkant R, Winham SJ, Hildebrandt M, Huff C, Li D, Wu X, Yu Y, Permuth JB, Levine DA, Schildkraut JM, Riggan MJ, Berchuck A, Webb PM, Group OS, Cybulski C, Gronwald J, Jakubowska A, Lubinski J, Alsop J, Harrington P, Chan I, Menon U, Pearce CL, Wu AH, de Fazio A, Kennedy CJ, Goode E, Ramus S, Gayther S, Pharoah P (2020) Population-based targeted sequencing of 54 candidate genes identifies PALB2 as a susceptibility gene for high-grade serous ovarian cancer. J Med Genet. https://doi.org/10.1136/jmedgenet-2019-106739
Yang X, Leslie G, Doroszuk A, Schneider S, Allen J, Decker B, Dunning AM, Redman J, Scarth J, Plaskocinska I, Luccarini C, Shah M, Pooley K, Dorling L, Lee A, Adank MA, Adlard J, Aittomäki K, Andrulis IL, Ang P, Barwell J, Bernstein JL, Bobolis K, Borg Å, Blomqvist C, Claes KBM, Concannon P, Cuggia A, Culver JO, Damiola F, de Pauw A, Diez O, Dolinsky JS, Domchek SM, Engel C, Evans DG, Fostira F, Garber J, Golmard L, Goode EL, Gruber SB, Hahnen E, Hake C, Heikkinen T, Hurley JE, Janavicius R, Kleibl Z, Kleiblova P, Konstantopoulou I, Kvist A, Laduca H, Lee ASG, Lesueur F, Maher ER, Mannermaa A, Manoukian S, McFarland R, McKinnon W, Meindl A, Metcalfe K, Mohd Taib NA, Moilanen J, Nathanson KL, Neuhausen S, Ng PS, Nguyen-Dumont T, Nielsen SM, Obermair F, Offit K, Olopade OI, Ottini L, Penkert J, Pylkäs K, Radice P, Ramus SJ, Rudaitis V, Side L, Silva-Smith R, Silvestri V, Skytte A-B, Slavin T, Soukupova J, Tondini C, Trainer AH, Unzeitig G, Usha L, van Overeem HT, Whitworth J, Wood M, Yip CH, Yoon S-Y, Yussuf A, Zogopoulos G, Goldgar D, Hopper JL, Chenevix-Trench G, Pharoah P, George SHL, Balmaña J, Houdayer C, James P, El-Haffaf Z, Ehrencrona H, Janatova M, Peterlongo P, Nevanlinna H, Schmutzler R, Teo S-H, Robson M, Pal T, Couch F, Weitzel JN, Elliott A, Southey M, Winqvist R, Easton DF, Foulkes WD, Antoniou AC, Tischkowitz M (2019) Cancer risks associated with germline PALB2 pathogenic variants: An international study of 524 families. J Clin Oncol 38(7):674–685. https://doi.org/10.1200/JCO.19.01907
Vysotskaia V, Kaseniit KE, Bucheit L, Ready K, Price K, Johansen Taber K (2020) Clinical utility of hereditary cancer panel testing: impact of PALB2, ATM, CHEK2, NBN, BRIP1, RAD51C, and RAD51D results on patient management and adherence to provider recommendations. Cancer 126(3):549–558. https://doi.org/10.1002/cncr.32572
Hall MJ, Patrick-Miller LJ, Egleston BL, Domchek SM, Daly MB, Ganschow P, Grana G, Olopade OI, Fetzer D, Brandt A, Chambers R, Clark DF, Forman A, Gaber R, Gulden C, Horte J, Long JM, Lucas T, Madaan S, Mattie K, McKenna D, Montgomery S, Nielsen S, Powers J, Rainey K, Rybak C, Savage M, Seelaus C, Stoll J, Stopfer JE, Yao XS, Bradbury AR (2018) Use and patient-reported outcomes of clinical multigene panel testing for cancer susceptibility in the multicenter communication of genetic test results by telephone study. JCO Precis Oncol. https://doi.org/10.1200/PO.18.00199
Graffeo R, Livraghi L, Pagani O, Goldhirsch A, Partridge AH, Garber JE (2016) Time to incorporate germline multigene panel testing into breast and ovarian cancer patient care. Breast Cancer Res Treat 160(3):393–410. https://doi.org/10.1007/s10549-016-4003-9
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, Lu S, Kemberling H, Wilt C, Luber BS, Wong F, Azad NS, Rucki AA, Laheru D, Donehower R, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Greten TF, Duffy AG, Ciombor KK, Eyring AD, Lam BH, Joe A, Kang SP, Holdhoff M, Danilova L, Cope L, Meyer C, Zhou S, Goldberg RM, Armstrong DK, Bever KM, Fader AN, Taube J, Housseau F, Spetzler D, Xiao N, Pardoll DM, Papadopoulos N, Kinzler KW, Eshleman JR, Vogelstein B, Anders RA, Diaz LA Jr (2017) Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 357(6349):409–413. https://doi.org/10.1126/science.aan6733
Hamilton JG, Lobel M, Moyer A (2009) Emotional distress following genetic testing for hereditary breast and ovarian cancer: a meta-analytic review. Health Psychol 28(4):510–518. https://doi.org/10.1037/a0014778
Murakami Y, Okamura H, Sugano K, Yoshida T, Kazuma K, Akechi T, Uchitomi Y (2004) Psychologic distress after disclosure of genetic test results regarding hereditary nonpolyposis colorectal carcinoma: a preliminary report. Cancer 101(2):395–403. https://doi.org/10.1002/cncr.20363
van Oostrom I, Meijers-Heijboer H, Duivenvoorden HJ, Bröcker-Vriends AHJT, van Asperen CJ, Sijmons RH, Seynaeve C, Van Gool AR, Klijn JGM, Tibben A (2007) Prognostic factors for hereditary cancer distress six months after BRCA1/2 or HNPCC genetic susceptibility testing. Eur J Cancer 43(1):71–77. https://doi.org/10.1016/j.ejca.2006.08.023
Liang MI, Wong DH, Walsh CS, Farias-Eisner R, Cohen JG (2018) Cancer genetic counseling and testing: perspectives of epithelial ovarian cancer patients and gynecologic oncology healthcare providers. J Genet Couns 27(1):177–186. https://doi.org/10.1007/s10897-017-0135-2
Lumish HS, Steinfeld H, Koval C, Russo D, Levinson E, Wynn J, Duong J, Chung WK (2017) Impact of panel gene testing for hereditary breast and ovarian cancer on patients. J Genet Couns 26(5):1116–1129. https://doi.org/10.1007/s10897-017-0090-y
Faller H, Brahler E, Harter M, Keller M, Schulz H, Wegscheider K, Weis J, Boehncke A, Reuter K, Richard M, Sehner S, Koch U, Mehnert A (2017) Unmet needs for information and psychosocial support in relation to quality of life and emotional distress: a comparison between gynecological and breast cancer patients. Patient Educ Couns 100(10):1934–1942. https://doi.org/10.1016/j.pec.2017.05.031
Kapoor NS, Curcio LD, Blakemore CA, Bremner AK, McFarland RE, West JG, Banks KC (2015) Multigene panel testing detects equal rates of pathogenic BRCA1/2 mutations and has a higher diagnostic yield compared to limited BRCA1/2 analysis alone in patients at risk for hereditary breast cancer. Ann Surg Oncol 22(10):3282–3288. https://doi.org/10.1245/s10434-015-4754-2
Montgomery SV, Barsevick AM, Egleston BL, Bingler R, Ruth K, Miller SM, Malick J, Cescon TP, Daly MB (2013) Preparing individuals to communicate genetic test results to their relatives: report of a randomized control trial. Fam Cancer 12(3):537–546. https://doi.org/10.1007/s10689-013-9609-z
Underhill-Blazey M, Blonquist T, Chittenden A, Pozzar R, Nayak M, Lansang K, Hong F, Garber J, Stopfer J (2020) Informing models of cancer genetic care in the era of multigene panel testing with patient-led recommendations. J Genet Couns. https://doi.org/10.1002/jgc4.1317
Cella D, Hughes C, Peterman A, Chang C-H, Peshkin BN, Schwartz MD, Wenzel L, Lemke A, Marcus AC, Lerman C (2002) A brief assessment of concerns associated with genetic testing for cancer: the multidimensional impact of cancer risk assessment (MICRA) questionnaire. Health Psychol 21(6):564–572. https://doi.org/10.1037/0278-6133.21.6.564
Underhill-Blazey M, Stopfer J, Chittenden A, Nayak MM, Lansang K, Lederman R, Garber J, Gundersen DA (2019) Development and testing of the KnowGene scale to assess general cancer genetic knowledge related to multigene panel testing. Patient Educ Couns 102(8):1558–1564. https://doi.org/10.1016/j.pec.2019.04.014
Hsieh H-F, Shannon S (2005) Three approaches to qualitative content analysis. Qual Health Res 15(9):1277–1288. https://doi.org/10.1177/1049732305276687
Bjornslett M, Dahl AA, Sorebo O, Dorum A (2015) Psychological distress related to BRCA testing in ovarian cancer patients. Fam Cancer 14(4):495–504. https://doi.org/10.1007/s10689-015-9811-2
Watts S, Prescott P, Mason J, McLeod N, Lewith G (2015) Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 5(11):e007618. https://doi.org/10.1136/bmjopen-2015-007618
Ozga M, Aghajanian C, Myers-Virtue S, McDonnell G, Jhanwar S, Hichenberg S, Sulimanoff I (2015) A systematic review of ovarian cancer and fear of recurrence. Palliat Support Care 13(6):1771–1780. https://doi.org/10.1017/S1478951515000127
Fox E, McCuaig J, Demsky R, Shuman C, Chitayat D, Maganti M, Murphy J, Rosen B, Ferguson S, Randall Armel S (2015) The sooner the better: genetic testing following ovarian cancer diagnosis. Gynecol Oncol 137(3):423–429. https://doi.org/10.1016/j.ygyno.2015.03.057
Gleeson M, Meiser B, Barlow-Stewart K, Trainer A, Tucker K, Watts K, Friedlander M, Kasparian N (2013) Communication and information needs of women diagnosed with ovarian cancer regarding treatment-focused genetic testing. Oncol Nurs Forum 40(3):275–283. https://doi.org/10.1188/13.ONF.40-03AP
Bradbury AR, Patrick-Miller LJ, Egleston BL, Hall MJ, Domchek SM, Daly MB, Ganschow P, Grana G, Olopade OI, Fetzer D, Brandt A, Chambers R, Clark DF, Forman A, Gaber R, Gulden C, Horte J, Long JM, Lucas T, Madaan S, Mattie K, McKenna D, Montgomery S, Nielsen S, Powers J, Rainey K, Rybak C, Savage M, Seelaus C, Stoll J, Stopfer JE, Yao XS (2018) Randomized noninferiority trial of telephone vs in-person disclosure of germline cancer genetic test results. J Natl Cancer Inst 110(9):985–993. https://doi.org/10.1093/jnci/djy015
O’Shea R, Meany M, Carroll C, Cody N, Healy D, Green A, Lynch SA (2016) Predictive genetic testing and alternatives to face to face results disclosure: a retrospective review of patients preference for alternative modes of BRCA 1 and 2 results disclosure in the Republic of Ireland. J Genet Couns 25(3):422–431. https://doi.org/10.1007/s10897-015-9887-8
Beri N, Patrick-Miller LJ, Egleston BL, Hall MJ, Domchek SM, Daly MB, Ganschow P, Grana G, Olopade OI, Fetzer D, Brandt A, Chambers R, Clark DF, Forman A, Gaber R, Gulden C, Horte J, Long J, Lucas T, Madaan S, Mattie K, McKenna D, Montgomery S, Nielsen S, Powers J, Rainey K, Rybak C, Savage M, Seelaus C, Stoll J, Stopfer JE, Yao XS, Bradbury AR (2019) Preferences for in-person disclosure: patients declining telephone disclosure characteristics and outcomes in the multicenter Communication Of GENetic Test Results by Telephone study. Clin Genet 95(2):293–301. https://doi.org/10.1111/cge.13474
Ashida S, Schafer EJ (2015) Family health information sharing among older adults: reaching more family members. J Commun Genet 6(1):17–27. https://doi.org/10.1007/s12687-014-0197-x
Hinchcliff EM, Bednar EM, Lu KH, Rauh-Hain JA (2019) Disparities in gynecologic cancer genetics evaluation. Gynecol Oncol 153(1):184–191. https://doi.org/10.1016/j.ygyno.2019.01.024
Pozzar RA, Berry DL (2017) Patient-centered research priorities in ovarian cancer: a systematic review of potential determinants of guideline care. Gynecol Oncol 147(3):714–722. https://doi.org/10.1016/j.ygyno.2017.10.004
Vogel RI, Niendorf K, Petzel S, Lee H, Teoh D, Blaes AH, Argenta P, Rivard C, Winterhoff B, Lee HY, Geller MA (2019) A patient-centered mobile health application to motivate use of genetic counseling among women with ovarian cancer: a pilot randomized controlled trial. Gynecol Oncol 153(1):100–107. https://doi.org/10.1016/j.ygyno.2019.01.019
Tea MM, Tan YY, Staudigl C, Eibl B, Renz R, Asseryanis E, Berger A, Pfeiler G, Singer CF (2018) Improving comprehension of genetic counseling for hereditary breast and ovarian cancer clients with a visual tool. PLoS ONE 13(7):e0200559. https://doi.org/10.1371/journal.pone.0200559
Epstein RM, Franks P, Fiscella K, Shields CG, Meldrum SC, Kravitz RL, Duberstein PR (2005) Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med 61(7):1516–1528. https://doi.org/10.1016/j.socscimed.2005.02.001
Littell RD, Kumar A, Einstein MH, Karam A, Bevis K (2019) Advanced communication: a critical component of high quality gynecologic cancer care. A Society of Gynecologic Oncology evidence based review and guide. Gynecol Oncol 155(1):161–169. https://doi.org/10.1016/j.ygyno.2019.07.026
Chivers Seymour K, Addington-Hall J, Lucassen AM, Foster CL (2010) What facilitates or impedes family communication following genetic testing for cancer risk? A systematic review and meta-synthesis of primary qualitative research. J Genet Couns 19(4):330–342. https://doi.org/10.1007/s10897-010-9296-y
Mesters I, Ausems M, Eichhorn S, Vasen H (2005) Informing one’s family about genetic testing for hereditary non-polyposis colorectal cancer (HNPCC): a retrospective exploratory study. Fam Cancer 4:163–167
Douma KF, Smets EM, Allain DC (2016) Non-genetic health professionals’ attitude towards, knowledge of and skills in discussing and ordering genetic testing for hereditary cancer. Fam Cancer 15(2):341–350. https://doi.org/10.1007/s10689-015-9852-6
Acknowledgements
The authors wish to acknowledge the Center for Cancer Genetics and Prevention and the Phyllis F. Cantor Center for Research in Nursing and Patient Care Services at Dana-Farber Cancer Institute for providing clinical and research support.
Funding
Rachel A. Pozzar is supported by an American Cancer Society Postdoctoral Fellowship (133063-PF-19–102-01-CPPB) and a Society for Medical Decision Making/Gordon and Betty Moore Foundation Fellowship in Medical Decision Making (GBMF7853). Funding for the parent study was provided by the Friends of Dana-Farber. The funding sources were not involved in the study design; data collection, analysis, and interpretation; manuscript preparation; or decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
RAP: Conceptualization, analysis, writing—original draft. FH: Analysis, writing—review and editing. NX: Analysis, writing—review and editing. JES: Conceptualization, writing—review and editing. MMN: Investigation, analysis, writing—review and editing. MU-B: Conceptualization, investigation, analysis, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
Jill E. Stopfer reports personal fees from Astra Zeneca. Rachel A. Pozzar, Fangxin Hong, Niya Xiong, Manan M. Nayak, and Meghan Underhill-Blazey have no conflict of interest to disclose.
Ethical approval
The Dana-Farber/Harvard Cancer Center Institutional Review Board approved the study protocol.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pozzar, R.A., Hong, F., Xiong, N. et al. Knowledge and psychosocial impact of genetic counseling and multigene panel testing among individuals with ovarian cancer. Familial Cancer 21, 35–47 (2022). https://doi.org/10.1007/s10689-021-00240-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-021-00240-6