Abstract
Background
Cirrhosis is associated with an increased risk for both bleeding and venous thromboembolic (VTE) complications. The data regarding the impact of etiology of cirrhosis on VTE risk is poorly understood.
Methods
In this retrospective observational analysis of the US Nationwide readmissions database 2019, we identified hospitalized patients who had cirrhosis from alcohol, viral, or nonalcoholic steatohepatitis (NASH) etiologies. We identified patients who had acute VTE, chronic/history of VTE, and portal venous thrombosis (PVT). Overall VTE risk was defined as the composite of acute and chronic VTE or PVT. The impact of etiology of cirrhosis on the crude and risk adjusted rates of VTE and PVT was studied.
Results
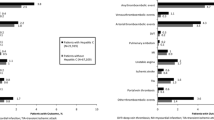
Of 432,383 patients with cirrhosis, 41.4% patients had NASH-cirrhosis, 39.7% had alcohol-related cirrhosis, and 18.9% had viral cirrhosis. The overall VTE rate was highest in patients with NASH cirrhosis (10.8%) followed by viral cirrhosis (9.7%) and alcohol-related cirrhosis (7.5%; P < 0.001). Similar results were observed for acute and chronic VTE. After risk adjustment, patients with NASH (OR 1.48 95% CI 1.42–1.54) and viral cirrhosis (OR 1.22 95% CI 1.17–1.29) had significantly higher overall VTE risk compared with alcohol-related cirrhosis. When separately evaluated, the adjusted risk for acute and chronic VTE was similar between patients with alcohol-related and viral cirrhosis but higher with NASH cirrhosis. PVT rate was highest with viral cirrhosis (4.3%) followed by NASH (2.8%) and alcohol-related cirrhosis (2.4%; P < 0.001). The adjusted risk of PVT was higher with viral (OR 1.61 95% CI 1.50–1.72) and NASH cirrhosis (OR 1.41 95% CI 1.31–1.52).
Conclusion
NASH cirrhosis was associated with a higher VTE risk compared with alcohol-related and viral etiologies. As NASH cirrhosis increases in prevalence as the major etiology of cirrhosis, it is important to understand the increased VTE risk associated with this condition to improve management strategies and patient outcomes.

Similar content being viewed by others
References
Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Hepatol Baltim Md 2020;72:1605–1616. https://doi.org/10.1002/hep.31173.
Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2020;18:2650–2666. https://doi.org/10.1016/j.cgh.2019.07.060.
Singh AD, Mucha SR, Lindenmeyer CC. Cirrhotic coagulopathy: a rebalanced hemostasis. Cleve Clin J Med 2022;89:523–533. https://doi.org/10.3949/ccjm.89a.21018.
Ambrosino P, Tarantino L, Di Minno G et al. The risk of venous thromboembolism in patients with cirrhosis. A systematic review and meta-analysis. Thromb Haemost 2017;117:139–148. https://doi.org/10.1160/TH16-06-0450.
Subhani M, Sheth A, Ahmed J et al. Incidence and prevalence of venous thromboembolism in chronic liver disease: a systematic review and meta-analysis. Thromb Res 2022;215:19–29. https://doi.org/10.1016/j.thromres.2022.05.004.
Wu H, Nguyen GC. Liver cirrhosis is associated with venous thromboembolism among hospitalized patients in a nationwide US study. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2010;8:800–805. https://doi.org/10.1016/j.cgh.2010.05.014.
Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Ungprasert P. Hepatitis C virus infection and risk of venous thromboembolism: a systematic review and meta-analysis. Ann Hepatol 2017;16:514–520. https://doi.org/10.5604/01.3001.0010.0279.
Stine JG, Niccum BA, Zimmet AN et al. Increased risk of venous thromboembolism in hospitalized patients with cirrhosis due to nonalcoholic steatohepatitis. Clin Transl Gastroenterol 2018;9:140. https://doi.org/10.1038/s41424-018-0002-y.
Ng KJ, Lee YK, Huang MY, Hsu CY, Su YC. Risks of venous thromboembolism in patients with liver cirrhosis: a nationwide cohort study in Taiwan. J Thromb Haemost 2015;13:206–213. https://doi.org/10.1111/jth.12805.
Jepsen P, Tapper EB, Deleuran T et al. Risk and outcome of venous and arterial thrombosis in patients with cirrhosis: a danish nation-wide cohort study. Hepatol Baltim Md 2021;74:2725–2734. https://doi.org/10.1002/hep.32019.
Bikdeli B, Jiménez D, Garcia-Tsao G et al. Venous Thromboembolism in patients with liver cirrhosis: findings from the RIETE (Registro Informatizado de la Enfermedad TromboEmbolica) Registry. Semin Thromb Hemost 2019;45:793–801. https://doi.org/10.1055/s-0039-1697682.
Søgaard KK, Horváth-Puhó E, Grønbaek H, Jepsen P, Vilstrup H, Sørensen HT. Risk of venous thromboembolism in patients with liver disease: a nationwide population-based case-control study. Am J Gastroenterol 2009;104:96–101. https://doi.org/10.1038/ajg.2008.34.
Molinari M, Fernandez-Carrillo C, Dai D et al. Portal vein thrombosis and renal dysfunction: a national comparative study of liver transplant recipients for NAFLD versus alcoholic cirrhosis. Transpl Int Off J Eur Soc Organ Transplant 2021;34:1105–1122. https://doi.org/10.1111/tri.13873.
Stine JG, Shah NL, Argo CK, Pelletier SJ, Caldwell SH, Northup PG. Increased risk of portal vein thrombosis in patients with cirrhosis due to nonalcoholic steatohepatitis. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc 2015;21:1016–1021. https://doi.org/10.1002/lt.24134.
Ambrosino P, Tarantino L, Criscuolo L, Nasto A, Celentano A, Di Minno MND. The risk of venous thromboembolism in patients with hepatitis C. A systematic review and meta-analysis. Thromb Haemost 2016;116:958–966. https://doi.org/10.1160/TH16-03-0185.
NRD Overview. Accessed March 21, 2019. https://www.hcup-us.ahrq.gov/nrdoverview.jsp
Hirode G, Saab S, Wong RJ. Trends in the burden of chronic liver disease among hospitalized US adults. JAMA Netw Open 2020;3:e201997. https://doi.org/10.1001/jamanetworkopen.2020.1997.
Bengtsson B, Askling J, Ludvigsson JF, Hagström H. Validity of administrative codes associated with cirrhosis in Sweden. Scand J Gastroenterol 2020;55:1205–1210. https://doi.org/10.1080/00365521.2020.1820566.
Hayward KL, Johnson AL, Mckillen BJ et al. ICD-10-AM codes for cirrhosis and related complications: key performance considerations for population and healthcare studies. BMJ Open Gastroenterol 2020;7:e000485. https://doi.org/10.1136/bmjgast-2020-000485.
Mapakshi S, Kramer JR, Richardson P, El-Serag HB, Kanwal F. Positive predictive value of international classification of diseases, 10th revision, codes for cirrhosis and its related complications. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2018;16:1677–1678. https://doi.org/10.1016/j.cgh.2018.01.042.
Shearer JE, Gonzalez JJ, Min T et al. Systematic review: development of a consensus code set to identify cirrhosis in electronic health records. Aliment Pharmacol Ther 2022;55:645–657. https://doi.org/10.1111/apt.16806.
Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol 2015;12:464–474. https://doi.org/10.1038/nrcardio.2015.83.
Raskob GE, Angchaisuksiri P, Blanco AN et al. Thrombosis: a major contributor to the global disease burden. J Thromb Haemost 2014;12:1580–1590. https://doi.org/10.1111/jth.12698.
Roberts LN, Hernandez-Gea V, Magnusson M et al. Thromboprophylaxis for venous thromboembolism prevention in hospitalized patients with cirrhosis: guidance from the SSC of the ISTH. J Thromb Haemost 2022;20:2237–2245. https://doi.org/10.1111/jth.15829.
Pant A, Kopec AK, Luyendyk JP. Role of the blood coagulation cascade in hepatic fibrosis. Am J Physiol Gastrointest Liver Physiol 2018;315:G171–G176. https://doi.org/10.1152/ajpgi.00402.2017.
Noureddin M, Vipani A, Bresee C et al. NASH leading cause of liver transplant in women: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol 2018;113:1649–1659. https://doi.org/10.1038/s41395-018-0088-6.
Ciavarella A, Gnocchi D, Custodero C et al. Translational insight into prothrombotic state and hypercoagulation in nonalcoholic fatty liver disease. Thromb Res 2021;198:139–150. https://doi.org/10.1016/j.thromres.2020.12.002.
Tripodi A, Lombardi R, Primignani M, La Mura V, Peyvandi F, Fracanzani AL. Hypercoagulability in patients with Nonalcoholic Fatty Liver Disease (NAFLD): causes and consequences. Biomedicines 2022;10:249. https://doi.org/10.3390/biomedicines10020249.
van der Windt DJ, Sud V, Zhang H et al. Neutrophil extracellular traps promote inflammation and development of hepatocellular carcinoma in nonalcoholic steatohepatitis. Hepatology 2018;68:1347–1360. https://doi.org/10.1002/hep.29914.
Luci C, Bourinet M, Leclère PS, Anty R, Gual P. Chronic inflammation in nonalcoholic steatohepatitis: molecular mechanisms and therapeutic strategies. Front Endocrinol 2020;11:597648. https://doi.org/10.3389/fendo.2020.597648.
Rivas G, Hummer-Bair B, Bezinover D, Kadry Z, Stine J. Plasminogen activator inhibitor is significantly elevated in liver transplant recipients with decompensated NASH cirrhosis. BMJ Open Gastroenterol 2021;8:e000683. https://doi.org/10.1136/bmjgast-2021-000683.
Ogresta D, Mrzljak A, Cigrovski Berkovic M, Bilic-Curcic I, Stojsavljevic-Shapeski S, Virovic-Jukic L. Coagulation and endothelial dysfunction associated with NAFLD: current status and therapeutic implications. J Clin Transl Hepatol 2022;10:339–355. https://doi.org/10.14218/JCTH.2021.00268.
Funding
None.
Author information
Authors and Affiliations
Contributions
GP: design, data acquisition and analysis, interpretation, prepared initial draft and final manuscript. WT: data and results interpretation, critical review of draft manuscript and final approval; RK: data and results interpretation, critical review of draft manuscript and final approval; SJ: study design, data and results interpretation, critical review of draft manuscript and final approval.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any related conflicts of interest.
Ethical approval
As this study used only data that was previously de-identified and available from a publicly available database, Institutional Review Board approval was not required.
Guarantor of the article
Savio John MD.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pemmasani, G., Tremaine, W., Karagozian, R. et al. Impact of Cirrhosis Etiology on the Risk for Venous Thromboembolism. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08440-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08440-7