Abstract
Purpose
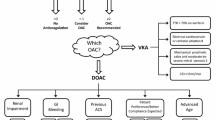
Direct oral anticoagulants (DOACs) have been approved, for over a decade, by both European and American medicine agencies, for treatment and prevention of several cardiovascular conditions. Since then, an increasing amount of data has been added to the medical literature day by day, resulting in a dichotomy in selection of the appropriate agent, dosage, and duration of treatment for special populations with multiple comorbidities. Considering these issues, we have prepared a comprehensive review for the clinical practitioner, to optimize the DOAC utilization in clinical practice.
Methods
A thorough literature search and review was conducted, concerning mainly the last decade. Our review focused on the current guidelines and the most recently published studies in PubMed, Science Direct Scopus, and Google Scholar to date.
Conclusion
The purpose of this study is to provide guidance for healthcare professionals for making proper decisions when confronted with clinical challenges. Nevertheless, further research is required to establish DOAC superiority in complicated cases, where there is clinical uncertainty.



Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Rose DK, Bar B. Direct oral anticoagulant agents: pharmacologic profile, indications, coagulation monitoring, and reversal agents. J Stroke Cerebrovasc Dis: Off J Natl Stroke Assoc. 2018;27(8):2049–58.
Carnicelli AP, et al. Direct oral anticoagulants versus warfarin in patients with atrial fibrillation: patient-level network meta-analyses of randomized clinical trials with interaction testing by age and sex. Circulation. 2022;145(4):242–55.
Chen A, et al. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc. 2020;9(13):e017559.
Direct oral anticoagulants: assessment report, European Medicines Agency. 2020. https://www.ema.europa.eu/en/documents/referral/assessment-report-article-53-procedure-direct-oral-anticoagulants-doacs_en.pdf. Accessed 19/04/2023.
Eliquis: EPAR – product information, European Medicines Agency. 2011. (Last updated: 09/09/2022). https://www.ema.europa.eu/en/documents/product-information/eliquis-epar-product-information_en.pdf. Accessed 19/04/2023.
Xarelto: EPAR – product information, European Medicines Agency. 2009. (Last updated: 23/02/2023). https://www.ema.europa.eu/en/documents/product-information/xarelto-epar-product-information_en.pdf. Accessed 19/04/2023.
Pradaxa: EPAR – product information, European Medicines Agency. 2009. (Last updated: 25/07/2022). https://www.ema.europa.eu/en/documents/product-information/pradaxa-epar-product-information_en.pdf. Accessed 19/04/2023.
Lixiana: EPAR – product information, European Medicines Agency. 2015. (Last updated: 25/05/2023). https://www.ema.europa.eu/en/documents/product-information/lixiana-epar-product-information_en.pdf. Accessed 19/04/2023.
Khan SU, et al. Dual antiplatelet therapy after percutaneous coronary intervention and drug-eluting stents: a systematic review and network meta-analysis. Circulation. 2020;142(15):1425–36.
Park DY, et al. Shortening the duration of dual antiplatelet therapy after percutaneous coronary intervention for acute coronary syndrome: a systematic review and meta-analysis. Am Heart J. 2022;251:101–14.
Gibson CM, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016;375(25):2423–34.
Cannon CP, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017;377(16):1513–24.
Dewilde WJM, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet (London, England). 2013;381(9872):1107–15.
Lopes RD, et al. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019;380(16):1509–24.
Berteotti M, et al. Clinical impact of high platelet reactivity in patients with atrial fibrillation and concomitant percutaneous coronary intervention on dual or triple antithrombotic therapy. J Thromb Thrombolysis. 2023;55(4):667–79.
Lianos I, et al. Platelet function testing in atrial fibrillation patients undergoing percutaneous coronary intervention. J Thromb Thrombolysis. 2023;55(1):42–50.
Lip GYH, et al. 2018 Joint European consensus document on the management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous cardiovascular interventions: a joint consensus document of the European Heart Rhythm Association (EHRA), European Society of Cardiology Working Group on Thrombosis, European Association of Percutaneous Cardiovascular Interventions (EAPCI), and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), Latin America Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern Africa (CASSA). Europace: Eur Pacing, Arrhythmias, Cardiac Electrophysiol: J Working Groups Cardiac Pacing, Arrhythmias, Cardiac Cell Electrophysiol Eur Soc Cardiol. 2019;21(2):192–3.
Angiolillo DJ, et al. Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a North American perspective: 2021 update. Circulation. 2021;143(6):583–96.
Zhu H, et al. Secondary prevention of antithrombotic therapy in patients with stable cardiovascular disease at high ischemic risk: a network meta-analysis of randomized controlled trials. Front Cardiovasc Med. 2023;9:1040473.
Antithrombotic Trialists’ (ATT) Collaboration, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet (London, England). 2009;373(9678):1849–60.
Coppens M, et al. Synergy of dual pathway inhibition in chronic cardiovascular disease. Circ Res. 2019;124(3):416–25.
Mega JL, et al. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med. 2012;366(1):9–19.
Eikelboom JW, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319–30.
Knuuti J, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77.
Yasuda S, et al. Antithrombotic therapy for atrial fibrillation with stable coronary disease. N Engl J Med. 2019;381(12):1103–13.
Tanigawa T, et al. Model-based dose selection for phase III rivaroxaban study in Japanese patients with non-valvular atrial fibrillation. Drug Metab Pharmacokinet. 2013;28(1):59–70.
Renda G, et al. Non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation and valvular heart disease. J Am College Cardiol. 2017;69(11):1363–71.
Eikelboom JW, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013;369(13):1206–14.
Durães AR, et al. Usefulness and safety of rivaroxaban in patients following isolated mitral valve replacement with a mechanical prosthesis. Am J Cardiol. 2018;122(6):1047–50.
Roost E, et al. Rivaroxaban in patients with mechanical heart valves: a pilot study. Thromb Res. 2020;186:1–6.
Duraes AR, et al. Rivaroxaban versus warfarin in patients with mechanical heart valves: open-label, proof-of-concept trial-the RIWA study. Am J Cardiovasc Drugs: Drugs, Devices, Other Interv. 2021;21(3):363–71.
Ryu R, Tran R. DOACs in mechanical and bioprosthetic heart valves: a narrative review of emerging data and future directions. Clin Appl Thromb/Hemost: Off J Int Acad Clin Appl Thromb/Hemost. 2022;28:10760296221103578.
Jawitz OK, et al. Rationale and design of PROACT Xa: a randomized, multicenter, open-label, clinical trial to evaluate the efficacy and safety of apixaban versus warfarin in patients with a mechanical On-X Aortic Heart Valve. Am Heart J. 2020;227:91–9.
Connolly SJ, et al. Rivaroxaban in rheumatic heart disease-associated atrial fibrillation. N Engl J Med. 2022;387(11):978–88.
Vahanian A, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632.
Guimarães PO, et al. Efficacy and safety of apixaban vs warfarin in patients with atrial fibrillation and prior bioprosthetic valve replacement or valve repair: insights from the ARISTOTLE trial. Clin Cardiol. 2019;42(5):568–71.
De Caterina R, et al. Valvular heart disease patients on edoxaban or warfarin in the ENGAGE AF-TIMI 48 trial. J Am College Cardiol. 2017;69(11):1372–82.
Montalescot, G. “Anti-thrombotic strategy to lower all cardiovascular and neurologic ischemic and hemorrhagic events after trans-aortic valve implantation for aortic stenosis—ATLANTIS.” American College of Cardiology Virtual Annual Scientific Session (ACC 2021). 2021.
Van Mieghem NM, et al. Edoxaban versus vitamin K antagonist for atrial fibrillation after TAVR. N Engl J Med. 2021;385(23):2150–60.
Guimarães HP, et al. Rivaroxaban in patients with atrial fibrillation and a bioprosthetic mitral valve. N Engl J Med. 2020;383(22):2117–26.
Durães AR, et al. Dabigatran versus warfarin after bioprosthesis valve replacement for the management of atrial fibrillation postoperatively: DAWA pilot study. Drugs R&D. 2016;16(2):149–54.
Collet JP, et al. Apixaban vs. standard of care after transcatheter aortic valve implantation: the ATLANTIS trial. Eur Heart J. 2022;43(29):2783–97.
Dangas GD, et al. A controlled trial of rivaroxaban after transcatheter aortic-valve replacement. N Engl J Med. 2020;382(2):120–9.
Maniwa N, et al. Anticoagulation combined with antiplatelet therapy in patients with left ventricular thrombus after first acute myocardial infarction. Eur Heart J. 2018;39(3):201–8.
Camaj A, et al. Left ventricular thrombus following acute myocardial infarction: JACC state-of-the-art review. J Am College Cardiol. 2022;79(10):1010–22.
Kajy M, Shokr M, Ramappa P. Use of direct oral anticoagulants in the treatment of left ventricular thrombus: systematic review of current literature. Am J Ther. 2020;27(6):e584–90.
Sedhom R, et al. Use of direct oral anticoagulants in the treatment of left ventricular thrombi: a systematic review. Am J Med. 2020;133(11):1266-1273.e6.
Ibanez B, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Robinson AA, et al. Off-label use of direct oral anticoagulants compared with warfarin for left ventricular thrombi. JAMA Cardiol. 2020;5(6):685–92.
Lip GYH, et al. Left atrial thrombus resolution in atrial fibrillation or flutter: results of a prospective study with rivaroxaban (X-TRA) and a retrospective observational registry providing baseline data (CLOT-AF). Am Heart J. 2016;178:126–34.
Cheng Y-Y, et al. Left atrial appendage thrombosis and oral anticoagulants: a meta-analysis of risk and treatment response. J Cardiovasc Dev Dis. 2022;9(10):351.
Delewi R, et al. Left ventricular thrombus formation after acute myocardial infarction. Heart (Br Cardiac Soc). 2012;98(23):1743–9.
Nso N, et al. Direct oral anticoagulants (DOAC) versus warfarin for the treatment of left ventricular thrombus (LVT) in patients with or without cardiorenal comorbidities, including CKD (chronic kidney disease) and atrial fibrillation: a systematic review and meta-analysis. Circulation. 2021;144(Suppl_1):A12654–A12654.
Huang L, et al. Systematic review of efficacy of direct oral anticoagulants and vitamin K antagonists in left ventricular thrombus. ESC Heart Failure. 2022;9(5):3519–32.
Condello F, et al. Direct oral anticoagulants versus vitamin K antagonists in the treatment of left ventricular thrombosis: a systematic review and meta-analysis. Minerva Cardiol Angiol. 2022;70(6):666–76.
Isa WYHW, et al. Apixaban versus warfarin in patients with left ventricular thrombus: a pilot prospective randomized outcome blinded study investigating size reduction or resolution of left ventricular thrombus. J Clin Prev Cardiol. 2020;9(4):150.
Alcalai R, et al. Apixaban vs. warfarin in patients with left ventricular thrombus: a prospective multicentre randomized clinical trial. Eur Heart J Cardiovasc Pharmacother. 2022;8(7):660–7.
Abdelnabi M, et al. Comparative study of oral anticoagulation in left ventricular thrombi (No-LVT Trial). J Am College Cardiol. 2021;77(12):1590–2.
He J, et al. Rationale and design of a prospective multi-center randomized trial of EARLY treatment by rivaroxaban versus warfarin in ST-segment elevation MYOcardial infarction with Left Ventricular Thrombus (EARLY-MYO-LVT trial). Ann Transl Med. 2020;8(6):392.
Shokr M, et al. Use of direct oral anticoagulants in the treatment of left ventricular thrombi: a tertiary center experience and review of the literature. Clin Case Rep. 2018;7(1):135–42.
Makrides Constantinos Andreas. Resolution of left ventricular postinfarction thrombi in patients undergoing percutaneous coronary intervention using rivaroxaban in addition to dual antiplatelet therapy. BMJ case reports. 2016;2016(bcr2016217843):26.
Wilks ML. Direct oral anticoagulants and cancer thrombosis: what APs need to know. J Adv Pract Oncol. 2022;13(3):253–6.
Falanga A, et al. Venous thromboembolism in cancer patients: ESMO Clinical Practice Guideline. Ann Oncology Off J Eur Soc Med Oncol. 2023;34(5):452–67.
Young AM, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol: Off J Am Soc Clin Oncol. 2018;36(20):2017–23.
McBane RD 2nd, et al. Apixaban and dalteparin in active malignancy-associated venous thromboembolism: the ADAM VTE trial. J Thromb Haemost: JTH. 2020;18(2):411–21.
Agnelli G, et al. Apixaban for the treatment of venous thromboembolism associated with cancer. N Engl J Med. 2020;382(17):1599–607.
Raskob GE, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018;378(7):615–24.
Planquette B, et al. Rivaroxaban vs dalteparin in cancer-associated thromboembolism: a randomized trial. Chest. 2022;161(3):781–90.
Lee AYY, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–53.
Sabatino J, et al. Direct oral anticoagulants in patients with active cancer: a systematic review and meta-analysis. JACC: CardioOncology. 2020;2(3):428–40.
Toyoda K. Antithrombotic therapy for pregnant women. Neurol Med Chir. 2013;53(8):526–30.
Youssef G. “Management of atrial fibrillation during pregnancy.” E-Journal of Cardiology Practice. 2019. Vol. 17, N° 15 - 17 Jul 2019
Beyer-Westendorf J, et al. Safety of direct oral anticoagulant exposure during pregnancy: a retrospective cohort study. Lancet Haematol. 2020;7(12):e884–91.
Beyer-Westendorf J, Marten S, Michalski F. Outcome of NOAC exposure during pregnancy (... and the problem of event reporting...). Blood. 2015;126(23):1125.
Said S, Hernandez GT. The link between chronic kidney disease and cardiovascular disease. J Nephropathol. 2014;3(3):99–104.
Lau YC, et al. Atrial fibrillation and thromboembolism in patients with chronic kidney disease. J Am College Cardiol. 2016;68(13):1452–64.
Christiansen CF, et al. Kidney disease and risk of venous thromboembolism: a nationwide population-based case-control study. J Thromb Haemost: JTH. 2014;12(9):1449–54.
Rogula S, et al. Safety and efficacy of DOACs in patients with advanced and end-stage renal disease. Int J Environ Res Public Health. 2022;19(3):1436.
Jain N, Reilly RF. Clinical pharmacology of oral anticoagulants in patients with kidney disease. Clin J Am Soc Nephrol: CJASN. 2019;14(2):278–87.
Kumar S, et al. Anticoagulation in concomitant chronic kidney disease and atrial fibrillation: JACC Review Topic of the Week. J Am College Cardiol. 2019;74(17):2204–15.
Aursulesei V, Costache II. Anticoagulation in chronic kidney disease: from guidelines to clinical practice. Clin Cardiol. 2019;42(8):774–82.
ROCKET AF Study Investigators. Rivaroxaban-once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation: rationale and design of the ROCKET AF study. Am Heart J. 2010;159(3):340-347.e1.
Landman GW, Gans ROB. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2011;364(12):1178.
Connolly SJ, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Schulman S, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–52.
Giugliano RP, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Investigators H-VTE, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369(15):1406–15.
Lopes RD, et al. Apixaban for reduction in stroke and other ThromboemboLic events in atrial fibrillation (ARISTOTLE) trial: design and rationale. Am Heart J. 2010;159(3):331–9.
Agnelli G, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799–808.
Steffel J, et al. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace: Eur Pacing, Arrhythmias, Cardiac Electrophysiol: J Working Groups Cardiac Pacing, Arrhythmias, Cardiac Cell Electrophysiol Eur Soc Cardiol. 2021;23(10):1612–76.
Eliquis: highlights of prescribing information, Food and Drug Administration. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202155s000lbl.pdf. Accessed 25/04/2023.
Harrington, Josephine et al. “Direct Oral Anticoagulants Versus Warfarin Across the Spectrum of Kidney Function: Patient-Level Network Meta-Analyses From COMBINE AF.” Circulation. 2023;147,23:1748-1757.
Bohula EA, et al. Impact of Renal function on outcomes with edoxaban in the ENGAGE AF-TIMI 48 trial. Circulation. 2016;134(1):24–36.
Yu HT, et al. Impact of renal function on outcomes with edoxaban in real-world patients with atrial fibrillation. Stroke. 2018;49(10):2421–9.
Wang Y, et al. Efficacy and safety of renal function on edoxaban versus warfarin for atrial fibrillation: a systematic review and meta-analysis. Medicines (Basel, Switzerland). 2023;10(1):13.
Chan KE, et al. Dabigatran and rivaroxaban use in atrial fibrillation patients on hemodialysis. Circulation. 2015;131(11):972–9.
Siontis KC, et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018;138(15):1519–29.
Miao B, et al. Rivaroxaban versus apixaban in non-valvular atrial fibrillation patients with end-stage renal disease or receiving dialysis. Eur J Haematol. 2020;104(4):328–35.
Pokorney SD, et al. Apixaban for patients with atrial fibrillation on hemodialysis: a multicenter randomized controlled trial. Circulation. 2022;146(23):1735–45.
Reinecke H, et al. A randomized controlled trial comparing apixaban with the vitamin K antagonist phenprocoumon in patients on chronic hemodialysis: the AXADIA-AFNET 8 study. Circulation. 2023;147(4):296–309.
Strategies for the management of atrial fibrillation in patients receiving dialysis (SAFE-D). 2019. ClinicalTrials.gov. Access 25 April 2023.
Semmler G, et al. Safety of direct oral anticoagulants in patients with advanced liver disease. Liver Int: Off J Int Assoc Study Liver. 2021;41(9):2159–70.
O’Leary JG, et al. AGA clinical practice update: coagulation in cirrhosis. Gastroenterology. 2019;157(1):34-43.e1.
Qamar A, et al. Oral anticoagulation in patients with liver disease. J Am College Cardiol. 2018;71(19):2162–75.
Lawal OD, et al. Comparative effectiveness and safety of direct oral anticoagulants and warfarin in patients with atrial fibrillation and chronic liver disease: a nationwide cohort study. Circulation. 2023;147(10):782–94.
Chagnac A, et al. Glomerular hemodynamics in severe obesity. Am J Physiol Renal Physiol. 2000;278(5):F817–22.
Wallace JL, et al. Comparison of initial warfarin response in obese patients versus non-obese patients. J Thromb Thrombolysis. 2013;36(1):96–101.
Malik AH, et al. Impact of weight on the efficacy and safety of direct-acting oral anticoagulants in patients with non-valvular atrial fibrillation: a meta-analysis. Europace: Eur Pacing, Arrhythmias, Cardiac Electrophysiol: J Working Groups Cardiac Pacing, Arrhythmias, Cardiac Cell Electrophysiol Eur Soc Cardiol. 2020;22(3):361–7.
Martin K, et al. Use of the direct oral anticoagulants in obese patients: guidance from the SSC of the ISTH. J Thromb Haemost: JTH. 2016;14(6):1308–13.
Piran S, et al. Peak plasma concentration of direct oral anticoagulants in obese patients weighing over 120 kilograms: a retrospective study. Res Pract Thromb Haemost. 2018;2(4):684–8.
Coons, James C., et al. Effectiveness and safety of direct oral anticoagulants versus warfarin in obese patients with acute venous thromboembolism. Pharmacother J Human Pharmacol Drug Ther 2020;40.3:204-210.
Mhanna M, et al. Direct oral anticoagulants versus warfarin in morbidly obese patients with nonvalvular atrial fibrillation: a systematic review and meta-analysis. Am J Ther. 2021;28(5):e531–9.
Park CS, et al. Increased risk of major bleeding in underweight §patients with atrial fibrillation who were prescribed non-vitamin K antagonist oral anticoagulants. Heart Rhythm. 2017;14(4):501–7.
Boriani G, et al. Relationship between body mass index and outcomes in patients with atrial fibrillation treated with edoxaban or warfarin in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1541–50.
Hohnloser SH, et al. Efficacy and safety of apixaban versus warfarin in patients with atrial fibrillation and extremes in body weight. Circulation. 2019;139(20):2292–300.
Lee C-H, et al. Body mass index is an independent predictor of major bleeding in non-valvular atrial fibrillation patients taking dabigatran. Int J Cardiol. 2017;228:771–8.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design and implementation. Angeliki Mouzarou supervised the study. All authors were involved in literature search and review. The first draft of the manuscript was written by Maria Ioannou. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Fully compliant with ethical issues.
Consent to Participate/Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ioannou, M., Leonidou, E., Chaziri, I. et al. Direct Oral Anticoagulants: Navigating Through Clinical Challenges. Cardiovasc Drugs Ther 38, 637–650 (2024). https://doi.org/10.1007/s10557-023-07499-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-023-07499-0