Abstract
Background
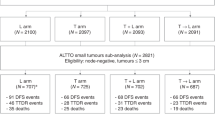
The primary aim of this randomized neoadjuvant trial in operable, HER2-positive breast cancer, was to determine the efficacy on pathologic complete response (pCR) of substituting lapatinib (L) for trastuzumab (T) or adding L to T, in combination with weekly paclitaxel (WP) following AC. Results on pCR were previously reported. Here, we report data on planned secondary endpoints, recurrence-free interval (RFI) post-surgery, and overall survival (OS).
Methods
All patients received standard AC q3 weeks × 4 cycles followed by WP (80 mg/m2) on days 1, 8, and 15, q28 days × 4 cycles. Concurrently with WP, patients received either T (4 mg/kg load, then 2 mg/kg) weekly until surgery, L (1250 mg) daily until surgery, or weekly T plus L (750 mg) daily until surgery. Following surgery, all patients received T to complete 52 weeks of HER2-targeted therapy. 522 of 529 randomized patients had follow-up. Median follow-up was 5.1 years.
Results
RFI at 4.5 years was 87.2%, 79.4% (p = 0.34; HR = 1.37; 95% CI 0.80, 2.34), and 89.4% (p = 0.37; HR = 0.70; 0.37, 1.32) for arms T, L, and TL, respectively. The corresponding five-year OS was 94.8%, 89.1% (p = 0.34; HR = 1.46; 0.68, 3.11), and 95.8% (p = 0.25; HR = 0.58; 0.22, 1.51), respectively. Patients with pCR had a much better prognosis, especially in the ER-negative cohort: RFI (HR = 0.23, p < 0.001) and OS (HR = 0.28, p < 0.001).
Conclusions
Although pCR, RFI, and OS were numerically better with the dual combination and less with L, the differences were not statistically significant. However, achievement of pCR again correlated with improved outcomes, especially remarkable in the ER-negative subset.
Clinical trials registration
NCT00486668



Similar content being viewed by others
Data availability
Data are available from the authors upon reasonable request and with permission of the NSABP Foundation.
Code availability
Data and programming codes are available from the authors upon reasonable request and with permission of the NSABP Foundation.
References
Gianni L, Eiermann W, Semiglazov V et al (2010) Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet 375:377–384. https://doi.org/10.1016/S0140-6736(09)61964-4
Cortazar P, Zhang L, Untch M et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384:164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Burris HA 3rd, Hurwitz HI, Dees EC et al (2005) Phase I safety, pharmacokinetics, and clinical activity study of lapatinib (GW572016), a reversible dual inhibitor of epidermal growth factor receptor tyrosine kinases, in heavily pretreated patients with metastatic carcinomas. J Clin Oncol 23:5305–5313. https://ascopubs.org/doi/full/10.1200/JCO.2005.16.584
Blackwell K, Kaplan E, Franco S et al (2004) A phase II, open-label, multicenter study of lapatinib (GW572016) in patients with metastatic breast cancer that has progressed on trastuzumab-containing regimens. Ann Oncol 15:27. https://doi.org/10.1093/oxfordjournals.annonc.a000353
Burstein H, Storniolo AM, Franco S et al (2004) A phase II, open-label, multicenter study of lapatinib in two cohorts of patients with advanced or metastatic breast cancer who have progressed while receiving trastuzumab-containing regimens. Ann Oncol 15:27. https://doi.org/10.1093/oxfordjournals.annonc.a000353
Geyer CE, Forster J, Lindquist D et al (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355:2733–2743. https://doi.org/10.1056/NEJMoa064320
Cameron D, Casey M, Oliva C, Newstat B, Imwalle B, Geyer CE (2010) Lapatinib plus capecitabine in women with HER-2-positive advanced breast cancer: final survival analysis of a phase III randomized trial. Oncologist 15:924–934. https://doi.org/10.1634/theoncologist.2009-0181
Robidoux A, Tang G, Rastogi P et al (2013) Lapatinib as a component of neoadjuvant therapy for HER2-positive operable breast cancer (NSABP protocol B-41): an open-label, randomised phase 3 trial. Lancet Oncol 14:1183–1192. https://doi.org/10.1016/S1470-2045(13)70411-X
Swain SM, Tang G, Lucas PC et al (2019) Pathologic complete response and outcomes by intrinsic subtypes in NSABP B-41, a randomized neoadjuvant trial of chemotherapy with trastuzumab, lapatinib, or the combination. Breast Cancer Res Treat 178:389–399. https://doi.org/10.1007/s10549-019-05398-3
Swain SM, Tang G, Brauer HA et al (2020) NSABP B-41, a randomized neoadjuvant trial: genes and signatures associated with pathologic complete response. Clin Cancer Res 15(26):4233–4241. https://doi.org/10.1158/1078-0432.CCR-20-0152
White SJ, Freedman LS (1978) Allocation of patients to treatment groups in a controlled clinical study. Br J Cancer 37(5):849–857. https://doi.org/10.1038/bjc.1978.124
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481. https://www.tandfonline.com/doi/abs/10.1080/01621459.1958.10501452
Shaffer JP (1986) Modified sequentially rejective multiple test procedures. J Am Stat Assoc 395:826–831. https://www.jstor.org/stable/2289016
Konecny GE, Pegram MD, Venkatesan N et al (2006) Activity of the dual kinase inhibitor lapatinib (GW572016) against HER-2-overexpressing and trastuzumab-treated breast cancer cells. Cancer Res 66(3):1630–1639. https://doi.org/10.1158/0008-5472.CAN-05-1182
Carey LA, Berry DA, Cirrincione CT et al (2016) Molecular heterogeneity and response to neoadjuvant human epidermal growth factor receptor 2 targeting in CALGB 40601, a randomized phase III trial of paclitaxel plus trastuzumab with or without lapatinib. J Clin Oncol 34:542–549. https://ascopubs.org/doi/pdf/10.1200/JCO.2015.62.1268?role=tab
Fernandez-Martinez A, Krop IE, Hillman DW et al (2020) Survival, pathologic response, and genomics in CALGB 40601 (alliance), a neoadjuvant phase III Trial of paclitaxel-trastuzumab with or without lapatinib in HER2-positive breast cancer. J Clin Oncol. 38(35):4184–4193. https://ascopubs.org/doi/pdf/10.1200/JCO.20.01276?role=tab
Baselga J, Bradbury I, Eidtmann H et al (2012) Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet 379:633–640. https://doi.org/10.1016/S0140-6736(11)61847-3
de Azambuja E, Holmes AP, Piccart-Gebhart M et al (2014) Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol 15:1137–1146. https://doi.org/10.1016/S1470-2045(14)70320-1
Huober J, Holmes E, Baselga J et al (2019) Survival outcomes of the NeoALTTO study (BIG 1–06): updated results of a randomised multicenter phase III neoadjuvant clinical trial in patients with HER2-positive primary breast cancer. Eur J Cancer 118:169–177. https://doi.org/10.1016/j.ejca.2019.04.038
Gianni L, Pienkowski T, Im YH et al (2012) Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 13:25–32. https://doi.org/10.1016/S1470-2045(11)70336-9
Gianni L, Pienkowski T, Im YH et al (2016) 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol 17:791–800. https://doi.org/10.1016/S1470-2045(16)00163-7
Fernandez-Martinez A, Rediti M, Tang G et al (2022) Prognostic and predictive implications of the intrinsic subtypes and gene expression signatures in early-stage HER2+ breast cancer: a pooled analysis of CALGB 40601, NeoALTTO, and NSABP B-41 trials. J Clin Oncol 40:16. https://ascopubs.org/doi/abs/10.1200/JCO.2022.40.16_suppl.509
Schneeweiss A, Chia S, Hickish T et al (2013) Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol 24:2278–2284. https://doi.org/10.1093/annonc/mdt182
Piccart M, Procter M, Fumagalli D et al (2021) Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer in the APHINITY trial: 6 years’ follow-up. J Clin Oncol 39(13):1448–1457. https://ascopubs.org/doi/10.1200/JCO.20.01204
Acknowledgements
The authors would like to acknowledge Dr. André Robidoux for his invaluable contributions to this study. The authors would also like to thank Elaina Harper, Data Manager for this study; Christine I Rudock, Publications and Graphics Specialist; and Wendy L. Rea, Editorial Associate. They are all employees of NSABP, and were not compensated beyond their normal salaries for this work.
Funding
NSABP Foundation, Inc, and GlaxoSmithKline, during the course of the study. GlaxoSmithKline (GSK) provided lapatinib to all study sites as well as trastuzumab in Canada along with funding support. GSK provided input on the study design, but did not participate in data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors had full access to all the data and had final responsibility for the decision to submit for publication.
Ethical approval
NSABP B-41 was approved by local human investigations committees or institutional review boards in accordance with assurances filed with and approved by the US Department of Health and Human Services. Written informed consent was required.
Competing Interests
SH: Research funding for unrelated projects from Pfizer and Exact Sciences; Honorary Fees from Exact Sciences and Merck for Advisory Board meetings. CEG, Jr: Abbvie: Contracted Research (Terminated, Jul 1, 2022), Writing assistance (Terminated, Jul 1, 2022); AstraZeneca: Contracted Research (Ongoing), Writing assistance (Ongoing); Daiichi/Sankyo: Contracted Research (Ongoing); Exact Sciences: Consulting Fees (e.g., advisory boards) (Ongoing); F. Hoffman-La Roche Ltd: Contracted Research (Ongoing); Genentech: Contracted Research (Ongoing), Writing assistance (Ongoing) HDB: Non-relevant disclosures: Talks/honoraria, Genentech. J-FB: Honoraria/speaker’s fee: Roche, Exact Sciences, Merck, AstraZeneca; Advisory boards or speakers’ bureaus: Pfizer, Novartis, Merck. AstraZeneca, Lilly, Roche; Funded grants or clinical trials: Institutional PI, clinical trial: Roche, Merck, Lilly, Novartis, Pfizer, Bristol Myers Squibb, AstraZeneca (also Steering Committee). AMB: Consultant for AstraZeneca, Roche, Puma, Seattle Genetics, Macrogenics, Daiichi Sankyo. SMS: Grants/contracts: Genentech/Roche, Kailos Genetics, BCRF; Consulting fees: Roche/Genentech, Molecular Therapeutics; Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events: Genentech/Roche, Daiichi Sankyo; Support for attending meetings and/or travel: Genentech/Roche travel to Boston 11/2019; Participation on a Data Safety Monitoring Board or Advisory Board: DSMB AstraZeneca; Ad Board: AstraZeneca, Daiichi Sankyo, Exact Sciences, Biotheranostics, Natera, Merck, Silverback Therapeutics, Athenex, Lilly; Scientific Advisory Board: Inivata. Leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid: NSABP Vice chairman; CCF, ASCO Director; Receipt of equipment, materials, drugs, medical writing, gifts or other services: Third-party writing: Genentech/Roche and AstraZeneca. EPM: Genentech/Roche, Exact Sciences, Merck: Consultant, Speaker’s Bureau; Biotheranostics, Puma Biotechnology, Agendia, AstraZeneca: Consultant. All other authors have no other potential COIs to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10549_2023_6881_MOESM2_ESM.eps
Forest Plots Comparing Arms L and TL to Arm T in Recurrence-free Interval: B-41. The hazard ratios (HR) and their 95% CIs are obtained from the corresponding Cox proportional hazards models. HR>1 implies the superiority of arm T. Supplementary file2 (EPS 525 KB)
10549_2023_6881_MOESM3_ESM.eps
Forest Plots Comparing Arms L and TL to Arm T in Overall Survival: B-41. The hazard ratios (HR) and their 95% CIs are obtained from the corresponding Cox proportional hazards models. HR>1 implies the superiority of arm T. Supplementary file3 (EPS 292 KB)
10549_2023_6881_MOESM4_ESM.eps
Kaplan-Meier Estimates of Recurrence-free Interval by pCR Status among HR-positive Patients: B-41. Supplementary file4 (EPS 303 KB)
10549_2023_6881_MOESM5_ESM.eps
Kaplan-Meier Estimates of Recurrence-free Interval by pCR Status among HR-negative Patients: B-41. Supplementary file5 (EPS 305 KB)
10549_2023_6881_MOESM6_ESM.eps
Kaplan-Meier Estimates of Overall Survival by pCR Status among HR-positive Patients: B-41. Supplementary file6 (EPS 294 KB)
10549_2023_6881_MOESM7_ESM.eps
Kaplan-Meier Estimates of Overall Survival by pCR Status among HR-negative Patients: B-41. Supplementary file7 (EPS 294 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rastogi, P., Tang, G., Hassan, S. et al. Long-term outcomes of dual vs single HER2-directed neoadjuvant therapy in NSABP B-41. Breast Cancer Res Treat 199, 243–252 (2023). https://doi.org/10.1007/s10549-023-06881-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06881-8