Abstract
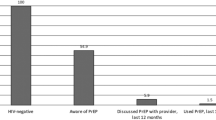
Long-acting injectable HIV pre-exposure prophylaxis (LAI-PrEP) could help overcome multilevel challenges to HIV prevention for people who inject drugs (PWID), including those in the binational San Diego-Tijuana metroplex. Yet, general PrEP awareness and interest in LAI-PrEP remain underexplored among PWID. From 2020 to 2021, 562 HIV-negative PWID in San Diego and Tijuana completed surveys assessing general PrEP awareness and interest in oral and LAI-PrEP. Modified Poisson regression examined factors associated with general PrEP awareness. Multinomial logistic regression assessed factors associated with interest in both oral and LAI-PrEP, oral PrEP only, LAI-PrEP only, or neither. General PrEP awareness was low (18%) and associated with experiencing unsheltered homelessness (adjusted prevalence ratio [APR] = 1.50, 95% confidence interval [CI]: 0.96–2.33), past 6-month fentanyl injection (APR = 1.53, 95% CI: 1.04–2.25), and transactional sex (APR = 1.71, 95% CI: 1.06–2.76). Interest in oral PrEP only was most common (44%), followed by LAI-PrEP only (25%) and neither (16%). Compared to the odds of being interested in LAI-PrEP only, the odds of being interested in oral PrEP only were lower among those who were stopped by police (AOR = 0.38, 95% CI: 0.22–0.65), reported past 6-month fentanyl injection (AOR = 0.33, 95% CI: 0.20–0.56), polydrug use (AOR = 0.48, 95% CI: 0.27–0.86), injecting multiple times daily (AOR = 0.26, 95% CI: 0.14–0.46), receptive syringe use (AOR = 0.30, 95% CI: 0.19–0.49), and higher perceived HIV risk (AOR = 0.24, 95% CI: 0.15–0.39). Interest in LAI-PrEP was more common among PWID reporting social and structural factors that could interfere with oral PrEP adherence, suggesting LAI-PrEP implementation could increase PrEP coverage among those most vulnerable to HIV.
Similar content being viewed by others
Data Availability
Data are available upon reasonable request to the Principal Investigator of La Frontera, Dr. Steffanie Strathdee (sstrathdee@health.ucsd.edu).
References
Hickman M, Larney S, Peacock A, Jones H, Grebely J, Degenhardt L. Competing global statistics on prevalence of injecting drug use: why does it matter and what can be done? Addiction. 2018;113(10):1768–74.
World Health Organization. People who inject drugs. https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/populations/people-who-inject-drugs. Accessed 4 Jan 2023.
Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–5.
County of San Diego Health and Human Services Agency Epidemiology and Immunization Services Branch. HIV/AIDS Epidemiology Report-2016. 2017. https://www.sandiegocounty.gov/content/dam/sdc/hhsa/programs/phs/documents/EpiReport2017final.pdf. Accessed 6 Jun 2023.
Joint United Nations Programme on HIV/AIDS (UNAIDS). The State of HIV Prevention in Mexico. 2021. https://hivpreventioncoalition.unaids.org/wp-content/uploads/2022/02/Mexico-2.pdf. Accessed 6 Jun 2023.
Brouwer KC, Case P, Ramos R, et al. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Subst Use Misuse. 2006;41(5):707–27.
Mehta SR, Wertheim JO, Brouwer KC, et al. HIV transmission networks in the San Diego-Tijuana Border Region. EBioMedicine. 2015;2(10):1456–63.
Vrancken B, Mehta SR, Ávila-Ríos S, et al. Dynamics and dispersal of local human immunodeficiency virus epidemics within San Diego and across the San Diego-Tijuana Border. Clin Infect Dis. 2021;73(7):e2018–25.
Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Chou R, Evans C, Hoverman A, et al. Preexposure prophylaxis for the prevention of HIV infection: evidence report and systematic review for the US preventive services task force. JAMA. 2019;321(22):2214–30.
Secretaría de Salud de Estados Unidos Mexicanos. Guía de atención para otorgar profilaxis preexposición. 2022. https://www.gob.mx/censida/documentos/guia-de-atencion-para-otorgar-profilaxis-preexposicion. Accessed 6 Jun 2023.
Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among persons who inject drugs – national HIV behavioral surveillance: injection drug use, 23, Cities US. 2018. 2020. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-24.pdf. Accessed 6 Jun 2023.
National Institute on Drug Abuse (NIDA). Awareness and Use of Pre-Exposure Prophylaxis for HIV Rise in At-Risk Groups, But Not Enough. 2021; https://nida.nih.gov/news-events/nida-notes/2021/03/awareness-use-pre-exposure-prophylaxis-for-hiv-rise-in-at-risk-groups-but-not-enough. Accessed 6 Jun 2023.
Bazzi AR, Biancarelli DL, Childs E, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDS. 2018;32(12):529–37.
Earlywine JJ, Bazzi AR, Biello KB, Klevens RM. High prevalence of indications for pre-exposure prophylaxis among people who inject drugs in Boston, Massachusetts. Am J Prev Med. 2021;60(3):369–78.
Dubov A, Krakower DS, Rockwood N, Montgomery S, Shoptaw S. Provider implicit bias in prescribing HIV pre-exposure prophylaxis (PrEP) to people who inject drugs. J Gen Intern Med. 2023.
Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Biello KB, Bazzi AR, Mimiaga MJ, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J. 2018;15(1):55.
Bazzi AR, Drainoni ML, Biancarelli DL, et al. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions. BMC Public Health. 2019;19(1):31.
Motavalli D, Taylor JL, Childs E, et al. Health is on the back burner: multilevel barriers and facilitators to primary care among people who inject drugs. J Gen Intern Med. 2021;36(1):129–37.
Allen ST, O’Rourke A, White RH, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural appalachia: a qualitative study. AIDS Behav. 2020;24(6):1942–50.
Bazzi AR, Valasek CJ, Streuli SA, et al. Long-acting injectable human immunodeficiency virus pre-exposure prophylaxis preferred over other modalities among people who inject drugs: findings from a qualitative study in California. AIDS Patient Care STDS. 2022;36(7):254–62.
King AR, Shah S, Randall LA, et al. Acceptability of injectable pre-exposure prophylaxis among people who inject drugs in three urban U.S. settings. BMC Infect Dis. 2022;22(1):737.
Biello KB, Mimiaga MJ, Valente PK, Saxena N, Bazzi AR. The past, present, and future of PrEP implementation among people who use drugs. Curr HIV/AIDS Rep. 2021;18(4):328–38.
Delany-Moretlwe S, Hughes JP, Bock P, et al. Cabotegravir for the prevention of HIV-1 in women: results from HPTN 084, a phase 3, randomised clinical trial. Lancet. 2022;399(10337):1779–89.
Landovitz RJ, Donnell D, Clement ME, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385(7):595–608.
Brody JK, Taylor J, Biello K, Bazzi AR. Towards equity for people who inject drugs in HIV prevention drug trials. Int J Drug Policy. 2021;96:103284.
Maloney KM, Le Guillou A, Driggers RA, et al. Projected impact of concurrently available long-acting injectable and daily-oral human immunodeficiency virus preexposure prophylaxis: a mathematical model. J Infect Dis. 2021;223(1):72–82.
Andrews CD, Bernard LS, Poon AY, et al. Cabotegravir long acting injection protects macaques against intravenous challenge with SIVmac251. AIDS. 2017;31(4):461–7.
Strathdee SA, Abramovitz D, Harvey-Vera A, et al. Prevalence and correlates of SARS-CoV-2 seropositivity among people who inject drugs in the San Diego-Tijuana border region. PLoS ONE. 2021;16(11):e0260286.
Yeager S, Abramovitz D, Harvey-Vera AY, et al. A cross-sectional study of factors associated with COVID-19 testing among people who inject drugs: missed opportunities for reaching those most at risk. BMC Public Health. 2022;22(1):842.
MedMira Laboratories Inc. Miriad: Rapid HCV/HIV anti-body test. 2018. https://medmira.com/wp-content/uploads/2020/01/815311005954.pdf. Accessed 6 Jun 2023.
Reynolds SJ, Muwonga J. OraQuick ADVANCE rapid HIV-1/2 antibody test. Expert Rev Mol Diagn. 2004;4(5):587–91.
Gorbach PM, Siminski S, Ragsdale A, Investigators CP. Cohort Profile: the collaborating Consortium of cohorts producing NIDA opportunities (C3PNO). Int J Epidemiol. 2021;50(1):31–40.
Robertson AM, Garfein RS, Wagner KD et al. Evaluating the impact of Mexico’s drug policy reforms on people who inject drugs in Tijuana, B.C., Mexico, and San Diego, CA, United States: a binational mixed methods research agenda. Harm Reduct J. 2014;11(1):4.
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88(6):791–804.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol. 1995;24(5):1064–7.
Royall RM. Model robust confidence-intervals using maximum-likelihood estimators. Int Stat Rev. 1986;54(2):221–6.
Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48.
Sterne JA, Davey Smith G. Sifting the evidence-what’s wrong with significance tests? BMJ. 2001;322(7280):226–31.
Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567(7748):305–7.
McFarland W, Lin J, Santos GM, Arayasirikul S, Raymond HF, Wilson E. Low PrEP awareness and use among people who inject drugs, San Francisco, 2018. AIDS Behav. 2020;24(5):1290–1293.
Corcorran MA, Scott JD, Tinsley J, Wald A, Glick SN. Awareness and correlates of HIV pre-exposure prophylaxis (PrEP) among HIV-negative people who access syringe services in Seattle, Washington. Subst Use Misuse. 2022;57(3):337–43.
Calabrese SK, Kalwicz DA, Modrakovic D, et al. An experimental study of the effects of patient race, sexual orientation, and injection drug use on providers’ PrEP-related clinical judgments. AIDS Behav. 2022;26(5):1393–421.
Pleuhs B, Mistler CB, Quinn KG, et al. Evidence of potential discriminatory HIV pre-exposure prophylaxis (PrEP) prescribing practices for people who inject drugs among a small percentage of providers in the U.S. J Prim Care Community Health. 2022;13:21501319211063999.
Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025–33.
Lambdin BH, Bluthenthal RN, Zibbell JE, Wenger L, Simpson K, Kral AH. Associations between perceived illicit fentanyl use and infectious disease risks among people who inject drugs. Int J Drug Policy. 2019;74:299–304.
Kenny KS, Kolla G, Greig S, et al. Association of illicit fentanyl use with injection risk practices among people who inject drugs. AIDS Behav. 2023;27(6):1757–65.
Centers for Disease Control and Prevention. About homelessness. 2022; https://www.cdc.gov/ddid/homelessness/about.html. Accessed 4 Dec 2022.
Joint United Nations Programme on HIV/AIDS and Strive. Transactional sex and HIV risk: from analysis to action. 2018. https://www.unaids.org/sites/default/files/media_asset/transactional-sex-and-hiv-risk_en.pdf. Accessed 6 Jun 2023.
Barry MP, Austin EJ, Bhatraju EP, et al. Qualitative inquiry into perceptions of HIV pre-exposure prophylaxis among people who inject drugs living with hepatitis C in Seattle, WA, USA. Harm Reduct J. 2022;19(1):121.
Walters SM, Coston B, Neaigus A, et al. The role of syringe exchange programs and sexual identity in awareness of pre-exposure prophylaxis (PrEP) for male persons who inject drugs. Int J Drug Policy. 2020;77:102671.
McNeil R, Small W. Safer environment interventions’: a qualitative synthesis of the experiences and perceptions of people who inject drugs. Soc Sci Med. 2014;106:151–8.
Walters SM, Platt J, Anakaraonye A, et al. Considerations for the design of pre-exposure Prophylaxis (PrEP) interventions for women: lessons learned from the implementation of a novel PrEP intervention. AIDS Behav. 2021;25(12):3987–99.
Shaw LC, Biello KB, Vahey S, Brody JK, Bazzi AR. PrEP disclosure and discussions within social networks of people who inject drugs experiencing homelessness: a brief report. BMC Public Health. 2023;23(1):263.
Sherman SG, Schneider KE, Park JN, et al. PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug Alcohol Depend. 2019;195:148–55.
Belludi A, McFall AM, Solomon SS, et al. Awareness of and willingness to use pre-exposure prophylaxis (PrEP) among people who inject drugs and men who have sex with men in India: results from a multi-city cross-sectional survey. PLoS ONE. 2021;16(2):e0247352.
Schneider KE, White RH, O’Rourke A, et al. Awareness of and interest in oral pre-exposure prophylaxis (PrEP) for HIV prevention and interest in hypothetical forms of PrEP among people who inject drugs in rural West Virginia. AIDS Care. 2021;33(6):721–8.
Biello KB, Edeza A, Salhaney P, et al. A missing perspective: injectable pre-exposure prophylaxis for people who inject drugs. AIDS Care. 2019;31(10):1214–20.
Mikulak A. Long-acting antiretroviral therapy suppresses HIV among people with unstable housing, mental illnesses, substance use disorder. 2023; https://www.nimh.nih.gov/news/science-news/2023/long-acting-antiretroviral-therapy-suppresses-hiv-among-people-with-unstable-housing-mental-illnesses-substance-use-disorder. Accessed 6 Jun 2023.
Miller AS, Krakower DS, Mayer KH. The potential of long-acting, injectable PrEP, and impediments to its uptake. J Urban Health. 2023;100(1):212–4.
Acknowledgements
The authors gratefully acknowledge the La Frontera study team and participants in the San Diego-Tijuana metroplex where data were collected. We also thank staff at Genayltye and Fluxergy, and the Center for AIDS Research at UC San Diego for assistance interpreting laboratory results.
Funding
This work was supported by the San Diego Center for AIDS Research (National Institute of Allergy and Infectious Diseases, grant P30AI036214) with additional support from the National Institute on Drug Abuse (grants R01DA049644-S1, R01DA049644-02S2, K01DA043412, 3K01DA043412-04S1, and T32DA023356), and the California HIV/AIDS Research Program (CHRP; grant OS17-SD001). The funders had no role in the decision to write and publish this manuscript or in the interpretation and presentation of findings.
Author information
Authors and Affiliations
Contributions
Conceptualization, Methodology, Funding acquisition: A.R.B., S.A.S., and H.A.P.; Data validation and curation: W.H.E., I.A., and H.A.P.; Data analysis: W.H.E. and H.A.P.; Original manuscript draft: W.H.E., A.R.B., H.A.P.; Resources and project administration: C.F.V., A.H.V., M.G.R., and S.A.S. All authors contributed to the interpretation of results, manuscript revisions, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
We declare no conflicts of interest.
Ethics Statement
Institutional review boards at UCSD and Xochicalco University approved all study activities.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eger, W.H., Bazzi, A.R., Valasek, C.J. et al. Long-acting Injectable PrEP Interest and General PrEP Awareness among People who Inject Drugs in the San Diego-Tijuana Border Metroplex. AIDS Behav 28, 1650–1661 (2024). https://doi.org/10.1007/s10461-024-04285-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-024-04285-3