Abstract
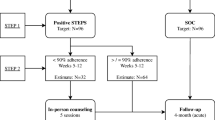
The Philippines HIV epidemic is among the fastest growing globally. Infections among men who have sex with men are rising at an alarming rate, necessitating targeted evidence-based interventions to retain people living with HIV in care, support adherence, and reach viral suppression. We conducted a 48-week prospective cohort study of 462 participants in which we provided a mobile health (mHealth) adherence support intervention using the Connect for Life platform. We observed an improvement in adherence, with the proportion of participants taking more than 95% of their antiretroviral therapy (ART) doses increasing from 78.6% at baseline to 90.3% at 48 weeks. Among treatment experienced participants, adherence improved significantly (McNemar’s test = 21.88, P < 0.001). Viral load suppression did not change, with 92.6% suppression at baseline and 92.0% at 48 weeks. Illicit drug use was associated with reduced adherence (aOR = 0.56, 95%CI 0.31–1.00, P = 0.05) and being on second-line therapy was associated with poor viral load suppression (aOR = 0.33, 95%CI 0.14–0.78, P = 0.01). Quality of life improved following ART initiation, from a mean of 84.6 points (of a possible 120) at baseline to 91.01 at 48 weeks. Due to technical issues, fidelity to the intended intervention was low, with 22.1% (102/462) of participants receiving any voice calls and most others receiving a scaled-back SMS intervention. The mHealth intervention did not have any observed effect on adherence or on viral load suppression. While evidence of effectiveness of mHealth adherence interventions is mixed, these platforms should continue to be explored as part of differentiated treatment support services.




Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available until after the study outcome evaluation is complete, but are available from the corresponding author upon reasonable request.
References
Joint United Nations Programme on HIV/AIDS (UNAIDS). Philippines country data 2020. 2020.
National HIV/AIDS & STI Surveillance and Strategic Information Unit. HIV/AIDS and ART Registry of the Philippines (HARP) report March 2022. Manila: National HIV/AIDS & STI Surveillance and Strategic Information Unit; 2022.
UNAIDS. The global AIDS strategy 2021–2026. Geneva: UNAIDS; 2021.
UNAIDS. Country factsheets: Philippines. AIDSinfo. Geneva: UNAIDS; 2021.
Eustaquio PC, Docken SS, Leyritana KT, Wulandari LPL. HIV care cascade among cisgender men who have sex with men in a key population-led community center in the Philippines. Int J STD AIDS. 2021;32(8):718–28.
Philippine Health Insurance Corporation. Outpatient HIV/AIDS treatment (OHAT) package (revision 2). 2021.
Ortego C, Huedo-Medina TB, Llorca J, Sevilla L, Santos P, Rodríguez E, Warren MR, Vejo J. Adherence to highly active antiretroviral therapy (HAART): a meta-analysis. AIDS Behav. 2011;15(7):1381–96.
Jiamsakul A, Kumarasamy N, Ditangco R, Li PCK, Phanuphak P, Sirisanthana T, Sungkanuparph S, Kantipong P, Lee CKC, Mustafa M, Merati TP, Kamarulzaman A, Singtoroj T, Law M. Factors associated with suboptimal adherence to antiretroviral therapy in Asia. J Int AIDS Soc. 2014;17:1–9.
Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, Bamberger JD, Chesney MA, Moss A. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14(4):357–66.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N, Hudson B. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30.
Ammassari A, Trotta MP, Shalev N, Marconi P, Antinori A. Beyond virological suppression: the role of adherence in the late HAART era. Antivir Ther. 2012;17(5):785–92.
Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM. Adherence to antiretroviral therapy and virologic failure: a meta-analysis. Medicine. 2016;95(15):e3361.
Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41.
Harrigan PR, Hogg RS, Dong WWY, Yip B, Wynhoven B, Woodward J, Brumme CJ, Brumme ZL, Mo T, Alexander CS, Montaner JSG. Predictors of HIV drug-resistance mutations in a large antiretroviral-naive cohort initiating triple antiretroviral therapy. J Infect Dis. 2005;191(3):339–47.
Tam LWY, Chui CKS, Brumme CJ, Bangsberg DR, Montaner JSG, Hogg RS, Harrigan PR. The relationship between resistance and adherence in drug-naive individuals initiating HAART is specific to individual drug classes. J Acquir Immune Defic Syndr. 2008;49(3):266–71.
Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–3.
Hogg RS, Heath K, Bangsberg D, Yip B, Press N, O’Shaughnessy MV, Montaner JSG. Intermittent use of triple-combination therapy is predictive of mortality at baseline and after 1 year of follow-up. AIDS. 2002;16(7):1051–8.
Dowshen N, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14(2):e51. https://doi.org/10.2196/jmir.2015.
Safren SA, Biello KB, Smeaton L, Mimiaga MJ, Walawander A, Lama JR, Rana A, Nyirenda M, Kayoyo VM, Samaneka W, Joglekar A, Celentano D, Martinez A, Remmert JE, Nair A, Lalloo UG, Kumarasamy N, Hakim J, Campbell TB. Psychosocial predictors of non-adherence and treatment failure in a large scale multi-national trial of antiretroviral therapy for HIV: data from the ACTG A5175/PEARLS trial. PLoS ONE. 2014. https://doi.org/10.1371/journal.pone.0104178.
Grierson J, Koelmeyer RL, Smith A, Pitts M. Adherence to antiretroviral therapy: factors independently associated with reported difficulty taking antiretroviral therapy in a national sample of HIV-positive Australians. HIV Med. 2011;12(9):562–9.
Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. AIDS Care. 2000;12(3):255–66.
Santos AP. Dying of shame and AIDS in the Philippines. Deutsche Welle Manila; 2016. Available from: http://www.dw.com/en/dying-of-shame-and-aids-in-the-philippines/a-19292896.
Santos AP. Sex and sensibilities podcast: HIV epidemic in the PH. Rappler Manila; 2015.
Gangcuangco LMA. HIV crisis in the Philippines: urgent actions needed. Lancet Public Health. 2019;4(2):e84. https://doi.org/10.1016/s2468-2667(18)30265-2.
O’Connor C, Leyritana K, Doyle AM, Lewis JJ, Gill R, Salvaña EM. Interactive mobile phone HIV adherence support for men who have sex with men in the Philippines connect for life study: mixed methods approach to intervention development and pilot testing. JMIR Form Res. 2022;6(2):e30811. https://doi.org/10.2196/30811.
Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, Patel V, Haines A. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e100136229.
Schnall R, Bakken S, Rojas M, Travers J, Carballo-dieguez A. mHealth technology as a persuasive tool for treatment, care and management of persons living with HIV. AIDS Behav. 2015;19:S81–9. https://doi.org/10.1007/s10461-014-0984-8.
Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. The Lancet. 2010;376(9755):1838–45.
Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(2):e88166.
Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lester RT, Mills EJ, Smieja M, Dolovich L, Kouanfack C. The Cameroon Mobile Phone SMS (CAMPS) trial: a randomized trial of text messaging versus usual care for adherence to antiretroviral therapy. PLoS ONE. 2012;7(12):6–12.
Kanters S, Park JJH, Chan K, Socias ME, Ford N, Forrest JI, Thorlund K, Nachega JB, Mills EJ. Interventions to improve adherence to antiretroviral therapy: a systematic review and network meta-analysis. Lancet HIV. 2017;4(1):e31–40.
Mbuagbaw L, Mursleen S, Lytvyn L, Smieja M, Dolovich L, Thabane L. Mobile phone text messaging interventions for HIV and other chronic diseases: an overview of systematic reviews and framework for evidence transfer. BMC Health Serv Res. 2015;15:33.
Mbuagbaw L, Sivaramalingam B, Navarro T, Hobson N, Keepanasseril A, Wilczynski NJ, Haynes BR, Team the PAR. Interventions for enhancing adherence to antiretroviral therapy (ART): a systematic review of high quality studies. AIDS Patient Care STDS. 2015;29(5):248–66.
Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. 2014;14(1):188.
Park LG, Howie-Esquivel J, Dracup K. A quantitative systematic review of the efficacy of mobile phone interventions to improve medication adherence. J Adv Nurs. 2014;70(9):1932–53.
Shah R, Watson J, Free C. A systematic review and meta-analysis in the effectiveness of mobile phone interventions used to improve adherence to antiretroviral therapy in HIV infection. BMC Public Health. 2019. https://doi.org/10.1186/s12889-019-6899-6.
Demena BA, Artavia-Mora L, Ouedraogo D, Thiombiano BA, Wagner N. A systematic review of mobile phone interventions (SMS/IVR/calls) to improve adherence and retention to antiretroviral treatment in low- and middle-income countries. AIDS Patient Care STDS. 2020. https://doi.org/10.1089/apc.2019.0181.
Chib A, Van VMH, Car J, Chib A, Helena M. mHealth adoption in low-resource environments: a review of the use of mobile healthcare in developing countries mHealth adoption in low-resource environments: a review of the use of mobile healthcare in developing countries. J Health Commun. 2015;20(1):4–34. https://doi.org/10.1080/10810730.2013.864735.
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach: second edition. Geneva: World Health Organization; 2016. Available from: https://www.who.int/publications/i/item/9789241549684.
O’Connor C, Leyritana K, Doyle AM, Birdthistle I, Lewis JJ, Gill R, Salvaña EM. Delivering an mHealth adherence support intervention for patients with HIV: mixed methods process evaluation of the Philippines connect for life study. JMIR Form Res. 2022. https://doi.org/10.2196/37163.
Murthy N, Chandrasekharan S, Prakash MP, Ganju A, Peter J, Kaonga N, Mechael P. Effects of an mHealth voice message service (mMitra) on maternal health knowledge and practices of low-income women in India: findings from a pseudo-randomized controlled trial. BMC Public Health. 2020;20(1):1–10.
Johnson & Johnson India. mMitra: connecting more moms via mobile. 2017. Available from: https://www.jnj.com/our-giving/mmitra-connecting-more-moms-via-mobile. Accessed 30 Dec 2021.
Parkes-Ratanshi RM, Nabaggala MS, Bwanika AN, Lamorde M, King R, Owarwo N, Odongpiny EAL, Orama R, Castelnuovo B, Kiragga A. Call for life Uganda TM: an RCT using interactive voice response for PLHIV on art. Top Antivir Med. 2019;27(SUPPL 1):405s–6s.
Byonanebye DM, Nabaggala MS, Naggirinya AB, Lamorde M, Oseku E, King R, Owarwo N, Laker E, Orama R, Castelnuovo B, Kiragga A, Parkes-Ratanshi R. An interactive voice response software to improve the quality of life of people living with HIV in Uganda: randomized controlled trial. JMIR mHealth uHealth. 2021;9(2):1–16.
Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. 2014. ISBN:978-1-291-84605-8.
Fisher JD, Amico KR, Fisher WA, Harman JJ. The information-motivation-behavioral skills model of antiretroviral adherence and its applications. Curr HIV/AIDS Rep. 2008;5(4):193–203.
Krishnan A, Ferro EG, Weikum D, Vagenas P, Lama JR, Sanchez J, Altice FL. Communication technology use and mHealth acceptance among HIV-infected men who have sex with men in Peru: implications for HIV prevention and treatment. AIDS Care. 2014;0121(October):1–10.
Uhrig JD, Lewis MA, Bann CM, Harris JL, Furberg D, Coomes CM, Kuhns LM, Uhrig JD, Lewis MA, Bann CM, Harris JL, Furberg RD, Coomes CM, Kuhns LM, Hiv A, Uhrig JD, Lewis MA, Bann CM, Harris JL, Furberg RD, Coomes CM, Kuhns LM. Addressing HIV knowledge, risk reduction, social support, and patient involvement using SMS: results of a proof-of-concept study addressing HIV knowledge, risk reduction, social support, and patient involvement using SMS: results of a proof-of-con. J Health Commun. 2012;17(Sup1):128–45. https://doi.org/10.1080/10810730.2011.649156.
UNAIDS. UNAIDS meeting report: information and communications technologies: engaging the private sector and communities in HIV programmes with gay men and other men who have sex with men. 2016. https://doi.org/10.1057/9781137542809_11.
Schnall R, Travers J, Rojas M, Carballo-Diéguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. J Med Internet Res. 2014;16(5):1–10.
Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–82. https://doi.org/10.1521/aeap.14.2.172.23902.
World Health Organization. WHOQOL-HIV BREF, 2012 revision. Geneva: World Health Organization; 2002.
World Health Organization. WHOQOL-HIV instrument: scoring and coding for the WHOQOL-HIV instruments: users manual, 2012 revision. WHOQOL-HIV instrument users manual. Geneva: World Health Organization; 2002.
NIH. Drinking levels defined. National Institute on Alcohol Abuse and Alcoholism (NIAAA). 2011. p. 5–6. Available from: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
Carliner H, Mauro PM, Brown QL, Shmulewitz D, Rahim-Juwel R, Sarvet AL, Wall MM, Martins SS, Carliner G, Hasin DS. Key substance use and mental health indicators in the United States. Drug Alcohol Depend. 2017;170:51–8.
Torres TS, Harrison LJ, La Rosa AM, Cardoso SW, Zheng L, Ngongondo M, Some F, Lalloo UG, Mwelase T, Collier AC, Hughes MD. Quality of life improvement in resource-limited settings after one year of second-line antiretroviral therapy use among adult men and women. AIDS. 2018;32(5):583–93. https://doi.org/10.1097/QAD.0000000000001738.
Dutra BS, Lédo AP, Lins-Kusterer L, Luz E, Prieto IR, Brites C. Changes health-related quality of life in HIV-infected patients following initiation of antiretroviral therapy: a longitudinal study. Braz J Infect Dis. 2019;23(4):211–7.
Lifson AR, Grund B, Gardner EM, Kaplan R, Denning E, Engen N, Carey CL, Chen F, Dao S, Florence E, Sanz J, Emery S. Improved quality of life with immediate versus deferred initiation of antiretroviral therapy in early asymptomatic HIV infection. AIDS. 2017;31(7):953–63. https://doi.org/10.1097/QAD.0000000000001417.
Philippines Department of Health. Department of Health Administrative order 2014-0031: policies and guidelines on the use of antiretroviral therapy (ART) among people living with human immunodeficiency virus and HIV-exposed infants. 2014.
Philippines Department of Health. Department of Health Administrative order 2018-0024: revised policies and guidelines on the use of antiretroviral therapy (ART) among people living with human immunodeficiency virus and HIV-exposed infants. 2018. Available from: https://doh.gov.ph/sites/default/files/health_programs/ao2018-0024.pdf.
Salvana EMT, Samonte GMJ, Telan E, Leyritana K, Tactacan-Abrenica RJ, Ching PR, Arevalo GM, Dungca NT, Peñalosa-Ramos C, Mendoza KAR, Trinidad LF, dela Tonga A, Lim J, Destura R, Alejandria M, Solante R, Arcangel L, Palaypayon NS, Schwem BE. High rates of tenofovir failure in a CRF01_AE-predominant HIV epidemic in the Philippines. Int J Infect Dis Int Soc Infect Dis. 2020;95:125–32.
Dungca NT, Schwem B, Arevalo G, Li KL, Salvana EM. 1257. Antiretroviral treatment failure in a prospective cohort of persons living with HIV in the Philippines. Open Forum Infect Dis. 2022. https://doi.org/10.1093/ofid/ofac492.1088.
John ME, Chipwaza B. HIV status disclosure among adults attending care and treatment clinic in Kilombero district, South-Eastern Tanzania. Int J Afr Nurs Sci. 2022;17(May):100434. https://doi.org/10.1016/j.ijans.2022.100434.
Peng W, Song X, Zhang C, Chen Y, Zhou Q, Välimäki MA, Li X. The proportion of HIV disclosure to sexual partners among people diagnosed with HIV in China: a systematic review and meta-analysis. Front Public Health. 2022;10:1004869.
Elsayed H, O’Connor C, Leyritana K, Salvana E, Cox SE. Depression, nutrition, and adherence to antiretroviral therapy in men who have sex with Men in Manila, Philippines. Front Public Health. 2021;9(September):1–10. https://doi.org/10.3389/fpubh.2021.644438.
O’Connor C, Leyritana K, Calica K, Gill R, Doyle AM, Lewis JJ, Salvaña EM. Risk factors affecting adherence to antiretroviral therapy among HIV patients in Manila, Philippines: a baseline cross-sectional analysis of the Philippines Connect for Life Study. Sex Health. 2021;18(1):95–103.
Hoenigl M, Chaillon A, Moore DJ, Morris SR, Smith DM, Little SJ. Clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with men clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with me. J Acquir Immune Defic Syndr. 2016;71(5):551–7. https://doi.org/10.1097/QAI.0000000000000888.
Human Rights Watch. Fueling the Philippines’ HIV epidemic: government barriers to condom use by men who have sex with men. 2016. Available from: https://www.hrw.org/sites/default/files/report_pdf/philippines1216_web.pdf.
Dombrowski JC, Dorabjee J, Strathdee SA, Diego S. Atrocity in the Philippines: how Rodrigo Duterte’s war on drug users may exacerbate the burgeoning HIV epidemic. J Acquir Immune Defic Syndr. 2017;76(1):23–5. https://doi.org/10.1097/QAI.0000000000001464.Atrocity.
Alibudbud R. Expanding pre-exposure prophylaxis (PrEP) utilization in the Philippine HIV crisis. J Prim Care Community Health. 2023;14:215013192311636. https://doi.org/10.1177/21501319231163643.
Philippines Department of Health. Philippines Interim National PrEP guidelines 2021. 2021. Available from: https://www.prepwatch.org/resources/philippines-interim-national-prep-guidelines-2021/. Accessed 10 Sept 2023.
Da Costa TM, Barbosa BJP, Gomes e Costa DA, Sigulem D, De Fátima Marin H, Filho AC, Pisa IT. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform. 2012;81(4):257–69.
Orrell C, Cohen K, Mauff K, Bangsberg DR, Maartens G, Wood R. A randomized controlled trial of real-time electronic adherence monitoring with text message dosing reminders in people starting first-line antiretroviral therapy. J Acquir Immune Defic Syndr. 2015;70(5):495–502.
Haberer JE, Musiimenta A, Atukunda EC, Musinguzi N, Wyatt MA, Ware NC, Bangsberg DR. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30(8):1295–9.
Dillingham R, Ingersoll K, Flickinger TE, Waldman AL, Grabowski M, Laurence C, Wispelwey E, Reynolds G, Conaway M, Cohn WF. PositiveLinks: a mobile health intervention for retention in HIV care and clinical outcomes with 12-month follow-up. AIDS Patient Care STDS. 2018;32(6):241–50.
UNAIDS. Ensuring that people living with HIV in the Philippines have access to treatment during COVID-19. unaids.org. 2020. p. 2020–22. Available from: https://www.unaids.org/en/resources/presscentre/featurestories/2020/april/20200408_philippines. Accessed 30 Jan 2022.
UNAIDS. Community-led HIV services stepped up in the Philippines during the COVID-19 pandemic. unaids.org. 2021. Available from: https://www.unaids.org/en/resources/presscentre/featurestories/2021/may/20210511_philippines. Accessed 30 Oct 2022.
Alibudbud R. The Philippine HIV crisis and the COVID-19 pandemic: a worsening crisis. Public Health. 2021;200(January):e1. https://doi.org/10.1016/j.puhe.2021.09.008.
Hung CC, Banerjee S, Gilada I, Green K, Inoue Y, Kamarulzaman A, Leyritana K, Phanuphak N, Wong T, Wong TH, Singh S, Choi JY. Impact of COVID-19 on the HIV care continuum in Asia: insights from people living with HIV, key populations, and HIV healthcare providers. PLoS ONE. 2022;17(7):1–18.
Finitsis DJ, Pellowski JA, Huedo-Medina TB, Fox MC, Kalichman SC. Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): a meta-analysis. J Behav Med. 2016;39(6):1043–55.
Kabore L, Muntner P, Chamot E, Zinski A, Burkholder G, Mugavero MJ. Self-report measures in the assessment of antiretroviral medication adherence: comparison with medication possession ratio and HIV viral load. J Int Assoc Provid AIDS Care. 2015;14(2):156–62.
Buscher A, Hartman C, Kallen M, Giordano T. Validity of self-report measures in assessing antiretroviral adherence of newly diagnosed, HAART-Naïve, HIV patients. HIV Clin Trials. 2011;12(5):244–54.
Acknowledgements
This study received sponsorship from Johnson & Johnson Global Public Health. We are thankful to our collaborators in the Johnson & Johnson team for developing the Connect for LifeTM platform and for their extensive work to tailor the technology to the Philippine setting: Randeep Gill, Paula McKenna, Piet Knaepen, Avinash Agrawal, and Jurgen de Beckker. Furthermore, this study would not have been possible without the efforts of our implementing partner the STI/AIDS Guidance Intervention & Prevention Unit at the Philippine General Hospital. Thank you to Cari Free, Ford Hickson, and James Hargreaves at London School of Hygiene and Tropical Medicine for their guidance during protocol development, especially regarding intervention development, behavior change theory, and process evaluation methodology.
Funding
This study received sponsorship from Johnson & Johnson Global Public Health.
Author information
Authors and Affiliations
Contributions
CO: Co-principal Investigator responsible for protocol development, data collection and analysis, development of manuscript. Trustee, Sustained Health Initiatives of the Philippines (SHIP). KL: Co-investigator responsible for medical services provision to patients in SHIP clinic. Medical Director, SHIP. Provided editorial input on manuscript. AMD: PhD co-supervisor, responsible for technical input on data analysis plan and editorial input on manuscript. Associate Professor of Epidemiology, LSHTM. JJL: Co-investigator and PhD co-supervisor responsible for technical input on protocol development and data analysis plan and editorial input on manuscript. Professor, Cardiff University. EMS: Co-principal Investigator responsible for oversight of research protocol. Provided editorial input on manuscript. Clinician at STI/AIDS Guidance Intervention & Prevention Unit at the Philippine General Hospital.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests. The study was funded through a sponsorship agreement with Johnson & Johnson Global Public Health (J&J), the developer of the Connect for Life™ platform. Per the licensing agreement all platform content and data are owned solely by the licensee (SHIP). While J&J had a collaborative role in the intervention development phase, all data collection and analysis herein were conducted by the study team at Sustained Health Initiatives of the Philippines.
Ethical Approval
Ethical clearance for the study was obtained from the University of the Philippines Manila Research Ethics Board (protocol number 2016-265-01) and from the London School of Hygiene and Tropical Medicine (reference number 11631).
Consent to Participate
All participants provided written consent prior to inclusion in the study. All data collection and reporting is compliant with national privacy laws, and no report will allow an individual participant to be identified.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
O’Connor, C., Leyritana, K., Doyle, A.M. et al. Changes in Adherence and Viral Load Suppression Among People with HIV in Manila: Outcomes of the Philippines Connect for Life Study. AIDS Behav 28, 837–853 (2024). https://doi.org/10.1007/s10461-023-04190-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04190-1