Abstract
Purpose
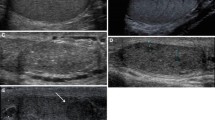
To determine the feasibility of high-frequency ultrasound (HFUS) for assessing seminiferous tubules and to understand high-resolution B-mode images of the testes in cases of azoospermia.
Methods
We verified how the histopathological images of testicular biopsy specimens can be observed using HFUS images and measurement analysis of seminiferous tubules was performed to 28 testes of 14 cases with azoospermia who underwent preoperative ultrasound and microdissection testicular sperm extraction (micro-TESE). The population consisted of obstructive azoospermia (OA) and non-obstructive azoospermia (NOA), including Sertoli cell-only syndrome (SCOS), and the other pathologies. Statistical verification of differences in seminiferous tubule diameters among preoperative ultrasound examination, ultrasound examination of pathological specimens, and histopathological specimens. We also examined the imagingpathology correlation via a case series presentation, aiming to identify imaging markers of testicular pathology and determine the possibility of predicting each condition.
Results
A comparison between HFUS images and histopathology from the same biopsy specimens suggested that ultrasonography could be seen as stereoscopic images due to its significantly greater slice thickness. The diameters of tubules were generally larger in pathological tissues as compared to ultrasonographic findings in OA and SCOS, but not in the other conditions. Comparisons provided insights into the predictability of SCOS and revealed imaging findings such as gaps between tubules and decreased diameter reflective of testicular damage.
Conclusion
Seminiferous tubules can be observed however the diameter of seminiferous tubules varies in imaging and histopathology depending on the pathology. Imaging findings that reflect testicular damage and the predictability of SCOS were revealed in this study, but further verification is required.








Similar content being viewed by others
Data availability
The information in this article can be inquired about to the extent that it does not concern the privacy of the patient, but it will not be accepted for disclosure of clinical or pathological images that are not published. For inquiries, please contact the corresponding author.
References
Nariyoshi S, Nakano K, Sukegawa G, et al. Ultrasonographically determined size of seminiferous tubules predicts sperm retrieval by microdissection testicular sperm extraction in men with nonobstructive azoospermia. Fertil Steril. 2020;113:97-104.e2.
Schlegel PN. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod. 1999;14:131–5.
Westlander G. Utility of micro-TESE in the most severe cases of non-obstructive azoospermia. Ups J Med Sci. 2020;125:99–103.
Yang Yu, Xi Qi, Wang R, et al. Intraoperative assessment of tubules in predicting microdissection testicular sperm extraction outcome in men with Sertoli cell-only syndrome. J Int Med Res. 2019;47:722–9.
Hayashi A, Giacalone G, Yamamoto T, et al. Ultra high-frequency ultrasonographic imaging with 70 MHz scanner for visualization of the lymphatic vessels. Plast Reconstr Surg Glob Open. 2019;7: e2086.
Levy J, Barrett DL, Harris N, et al. High-frequency ultrasound in clinical dermatology: a review. Ultrasound J. 2021;13:24.
Amer M, Zohdy W, Abd El Naser T, et al. Single tubule biopsy: a new objective microsurgical advancement for testicular sperm retrieval in patients with nonobstructive azoospermia. Fertil Steril. 2008;89:592–6.
Johnsen SG. Testicular biopsy score count–a method for registration of spermatogenesis in human testes: normal values and results in 335 hypogonadal males. Hormones. 1970;1:2–25.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Liu J, Wang Z, Li M, et al. Differential diagnostic value of obstructive and nonobstructive azoospermia by scrotal ultrasound. Ultrasound Q. 2017;33:272–5.
Hawksworth DJ, Szafran AA, Jordan PW, et al. Infertility in patients with klinefelter syndrome: optimal timing for sperm and testicular tissue cryopreservation. Rev Urol. 2018;20:56–62.
Shiraishi K, Matsuyama H. Klinefelter syndrome: from pediatrics to geriatrics. Reprod Med Biol. 2019;18:140–50.
Vakalopoulos I, Dimou P, Anagnostou I, et al. Impact of cancer and cancer treatment on male fertility. Hormones. 2015;14:579–89.
Yumura Y, Takeshima T, Komeya M, et al. Long-term fertility function sequelae in young male cancer survivors. World J Mens Health. 2023;41:255–71.
Ghanami Gashti N, Sadighi Gilani MA, Abbasi M. Sertoli cell-only syndrome: etiology and clinical management. J Assist Reprod Genet. 2021;38:559–72.
Li H, Chen LP, Yang J, et al. Predictive value of FSH, testicular volume, and histopathological findings for the sperm retrieval rate of microdissection TESE in nonobstructive azoospermia: a meta-analysis. Asian J Androl. 2018;20:30–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors received no financial support for the research authorship and/or publication of this article, and report that there are no other conflicts of interest.
Ethics statement
Informed consent was obtained from all patients undergoing micro-TESE during the study period, including cases excluded from measurement analysis. The ethics committee and institutional review board of the university hospital approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ohta, T., Kojo, K., Kurobe, M. et al. Feasibility of high-frequency ultrasound for seminiferous tubule assessment and correlation of B-mode imaging with pathological findings in the testis in azoospermia. J Med Ultrasonics (2024). https://doi.org/10.1007/s10396-024-01462-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10396-024-01462-8