Abstract
Aim
Healthcare resource allocation varies worldwide. It is integral that countries identify optimal allocation methods to distribute healthcare resources to ensure and sustain good population heath. This study examines the association between healthcare resource allocation and perception of health status across countries.
Subject and methods
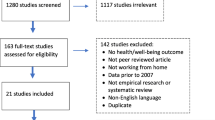
Data from OECD Health Statistics and OECD Health Care Resources is analyzed with visual analytics methodology.
Results
Findings show that the relationship between factors that influence resource allocation and health status differ based on the development status and geographic location of countries. In developing countries, there is a significant relationship between the number of hospitals and absence from work due to perceived poor health. Medical resource allocation is positively associated with health status perception in countries where the allocation is proportional to incidence of diseases. Among the various medical resources, medical personnel are the most important factor in both developing and developed countries in influencing the positive perceived health status of the population.
Conclusions
With more healthcare resources people’s life expectancy should increase, and overall mortality should decline. This study offers several implications for the future. Governments can take differential actions based on their citizens’ needs to improve their perceived health status. In general, there should be an emphasis on allocation of human medical resources, rather than medical equipment. Businesses should invest more in healthcare education to be able to implement and administer government health policies. Strategic investments in key healthcare resources can boost revenue and offer sufficient incentives for development of innovative medical technology.


















Similar content being viewed by others
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- OECD:
-
Organization for Economic Co-operation and Development
References
Ahlert M, Felder S, Vogt B (2012) Which patients do I treat? An experimental study with economics and physicians. Heal Econ Rev 2:1–11
Angelis A, Kanavos P, Montibeller G (2017) Resource allocation and priority setting in health care: a multi-criteria decision analysis problem of value? Global Policy 8:6–83
Angelis A, Kanavos P (2017) Multiple Criteria Decision Analysis (MCDA) for evaluating new medicines in Health Technology Assessment and beyond: The Advance Value Framework, Soc Sci Medicine 188:137–156, ISSN 0277-9536. https://doi.org/10.1016/j.socscimed.2017.06.024
Bangdiwala SI, Fonn S, Okoye O, Tollman S (2010) Workforce resources for health in developing countries. Public Health Rev 32(1):296–318
Beauchamp TL (2003) Methods and principles in biomedical ethics. J Med Ethics 29(5):269–274
Benishek LE, Kachalia A, Daugherty Biddison L, Wu AW, Biddison LD (2020) Mitigating healthcare worker distress from scarce medical resource allocation during a public health crisis. Chest 158(6):2285–2287
Bennett S, Chanfreau C (2005) Approaches to rationing antiretroviral treatment: ethical and equity implications. Bull World Health Organ 83:541–547
Chaudhury N, Hammer J, Kremer M, Muralidharan K, Rogers FH (2006) Missing in action: teacher and health worker absence in developing countries. J Econ Perspect 20(1):91–116
Chen C, Wang J, Yang C, Fan J (2016) Nurse practitioner job content and stress effects on anxiety and depressive symptoms, and self-perceived health status. J Nurs Manag 24:695–704
Cloos P, Ndao EM, Aho J, Benoît M, Fillol A, Munoz-Bertrand M, et al (2020) The negative self-perceived health of migrants with precarious status in Montreal, Canada: A cross-sectional study. PLoS ONE 15(4):e0231327. https://doi.org/10.1371/journal.pone.0231327
Diderichsen F (2004) Resource Allocation for Health Equity : Issues and Methods. Health, Nutrition and Population (HNP) Discussion paper. World Bank, Washington, DC. © World Bank. https://openknowledge.worldbank.org/handle/10986/13619. License: CC BY 3.0 IGO
Dieleman JL, Haakenstad A (2015) The complexity of resource allocation for health. Lancet Glob Health 3:e8–e9
Dieleman JL, Graves CM, Templin T, Johnson E, Baral R, Leach-Kemon K, Murray CJ (2014) Global health development assistance remained steady in 2013 but did not align with recipients’ disease burden. Health Aff 33(5):878–886
Dubois C-A, Mckee M (2006) Gross - national comparisons of human resources for health - what can we learn? Health Econ Policy Law 1:59–78
Eddy DM (1991a) Clinical decision making: from theory to practice. The individual vs society. Is there a conflict. JAMA 265(11):1446–1450
Eddy DM (1991b) Clinical decision making: from theory to practice. The individual vs society. Resolving the conflict. JAMA 265(18):2399–2406
Emanuel EJ (2000) Justice and managed care. Four principles for the just allocation of healthcare resources. Hast Cent Rep 30(3):8–16
Fleck L (2001) Healthcare justice and rational democratic deliberation. Am J Bioeth 1(2):20–21
Fox DM (2006) The determinants of policy for population health. Health Econ Policy Law 1:395–407
Gandjour A, Lauterbach KW (2000) Allocating resources in health care. HEPAC 2:116–121
Ghosh B, Scott JE (2011) Antecedents and catalysts for developing a healthcare analytic capability. Commun Assoc Inf Syst 29(22):395–410
Gil-Salmerón A, Valia-Cotanda E, Garces-Ferrer J (2018) The effect of perceived discrimination on the health status of immigrant population in Spain (Valencia). Int J Integr Care 18(S2):A345, pp. 1-8. https://doi.org/10.5334/ijic.s2345
Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Musgrove P (eds) (2006) Disease control priorities in developing countries (2nd edn). The World Bank, Washington, DC
Kaleta D, Polańska K, Dziankowska-Zaborszczyk E, Hanke W, Drygas W (2009) Factors influencing self-perception of health status. Cent Eur J Public Health 17(3):122–127
Keim D, Andrienko G, Fekete J-D, Görg C, Kohlhammer J, Melançon G (2008) Visual analytics: definition, process, and challenges. Lect Notes Comput Sci 4950:154–176
Kephart G, Asada Y (2009)Need-based resource allocation: different need indicators, different results? BMC Health Serv Res 9(1):122
Klein R, Maybin J (2012) Thinking about rationing. The King's Fund, London. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Thinking-about-rationing-the-kings-fund-may-2012.pdf. Accessed on 1 May 2020
Kohlhammer J, Keim D, Pohl M, Santucci G, Andrienko G (2011) Solving problems with visual analytics. Procedia Comp Sci 7:117–120
Kong NY, Kim DH (2020) Factors influencing health care use by health insurance subscribers and medical aid beneficiaries: a study based on data from the Korea welfare panel study database. BMC Public Health 20:1133. https://doi.org/10.1186/s12889-020-09073-x
Kunst AE, Bos V, Lahelma E, Bartley M, Lissau I, Regidor E et al (2005) Trends in socioeconomic inequalities in self-assessed health in 10 European countries. Int J Epidemiol 34(2):295–305
Li Q, Wei J, Jiang F, Zhou G, Jiang R, Chen M, Zhang X, Hu W (2020) Equity and efficiency in healthcare resource allocation in Jiangsu Province, China. Int J Equity Health 19:211. https://doi.org/10.1186/s12939-020-01320-2
Lin SH, Liao WC, Chen MY, Fan JY (2014) The impact of shift work on nurses’ job stress, sleep quality and self-perceived health status. J Nurs Manag 22(5):604–612
Maia MJ, Moniz AB (2014) Equity in access to MRI equipment. In: Michalek T, Hebáková L, Hennen L, Scherz C, Nierling L, Hahn J (eds) Technology assessment and policy areas of great transitions, 1st PACITA project conference, Technologické centrum. AV ČR, Praha, pp 307–313
Malinauskiene V, Leisyte P, Romualdas M, Kirtiklyte K (2011) Associations between self-rated health and psychosocial conditions, lifestyle factors and health resources among hospital nurses in Lithuania. J Adv Nurs 67(11):2383–2393
Martin S, Rice N, Smith PC (2008) Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ 27:826–842
Martin S, Rice N, Smith PC (2012) Comparing costs and outcomes across programmes of health care. Health Econ 21(3):316–337
McArthur JW (2013) Own the goals: what the millennium development goals have accomplished. Foreign Aff 92:152
Mitton C, Donaldson C (2004) Health care priority setting: principles, practice and challenges. Cost Eff Res Alloc 2(1):3
Mohsenpour SR, Arab M, Razavi SHE, Sari AA (2017) Exploring the challenges of the Iranian parliament about passing laws for resource allocation in healthcare: a qualitative study. Electron Physician 9(10):5418–5426
Mukamel DB, Zwanziger J, Bamezai A (2002) Hospital completion resource allocation and quality of care. BMC Health Serv Res 2:1–9
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C et al (2012)Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 380(9859):2197–2223
Obermann K, Chanturidze T, Glazinski B, Schuetz DK, Steinhauer H (2018) The shaded side of the UHC cube: a systematic review of human resources for health management and administration in social health protection schemes. Heal Econ Rev 8:1–7
Olson LM, Tang SFS, Newacheck PW (2005) Children in the United States with discontinuous health insurance coverage. N Engl J Med 353:382–391
Osterdal LP (2005) Axioms for health care resource allocation. J Health Econ 24:679–702
Otterson T, Evans DB, Mossialos E, Rottingen J-A(2017) Global Health financing towards 2030 and beyond. Health Econ Policy Law 12:105–111
Pontone GM, Williams JR, Anderson KE et al (2011) Anxiety and self-perceived health status in Parkinson’s disease. Parkinsonism Relat Disord 17(4):249–254
Raghupathi V, Raghupathi W (2013) An overview of health analytics. J Health Med Inform 14(3):132. https://doi.org/10.4172/2157-7420.1000132
Raghupathi V, Raghupathi W (2020) The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 78(20). https://doi.org/10.1186/s13690-020-00402-5
Raghupathi V, Ren J, Raghupathi W (2021) Understanding the nature and dimensions of litigation crowdfunding: a visual analytics approach. PLoS One 16(4):e0250522. https://doi.org/10.1371/journal.pone.0250522
Rawls J (1999) A theory of justice. Belknap Press of Harvard University. http://www.hup.harvard.edu/catalog.php?isbn=9780674000780. Accessed on 1 May 2020
Resch S, Ryckman T, Hecht R (2015) Funding AIDS programmes in the era of shared responsibility: an analysis of domestic funding in 12 low-income and middle-income countries. Lancet Glob Health 3(1):e52–61
Ritchwood TD, Bishu KG, Egede LE (2017) Trends in healthcare expenditure among people living with HIV/AIDS in the United States: evidence from 10 years of nationally representative data. Int J Equity Health 16(1):188. https://doi.org/10.1186/s12939-017-0683-y
Rural Information Hub (RIH) (2019) Demographic changes and aging population. https://www.ruralhealthinfo.org/toolkits/aging/1/demographics. Accessed on 1 May 2020
Sallasky E, Gursky EA (2006) The case for transforming governmental public health. Health Aff 25(4):1017–1028
Savel TG, Foldy S (2012) The role of public health informatics in enhancing public health surveillance. Morb Mortal Wkly Rep 61(3):20–24
Šplíchalová A, Tomášková H, Šlachtová H (2003) Risks of different self-approach to health in an industrial city population. Cent Eur J Public Health 11(3):142–148
Tao YK, Henry K, Zou Q, Zhong X (2014) Methods for measuring horizontal in health resource allocation: a comparative study. Heal Econ Rev 4:1–10
Thomas JJ, Cook KA (2006) A visual analytics agenda. IEEE Comp Graph Appl 26:10–13
Vingilis ER, Wade TJ, Seeley JS, Predictors of Adolescent Self-Rated Health (2002) Analysis of the National Population Health Survey. Can J Public Health 93(3):193–197
Wada K, Higuchi Y, Smith DR (2015) Socioeconomic status and self-reported health among middle-aged Japanese men: results from a nationwide longitudinal study. BMJ Open 5:e008178
Wagstaff A, Van Doorslaer E (1993) Equity in the finance and delivery of health care: an Int perspective. J Epidemiol Community Health 47(4):338–339
Wall AE, Pruett T, Stock P, Testa G (2020) Coronavirus disease 2019: utilizing an ethical framework for rationing absolutely scarce health-care resources in transplant allocation decisions. Am J Transplant 20(9):2332–2336
Wang F, Wang J-D, Huang Y-X(2016) Health expenditures spend for prevention economic performance and social welfare. Heal Econ Rev 6:1–10
Wróblewska W (2005) The male-female differences in health: the role of the health-related behaviours. In: Szamotulska K (ed) Polish population review. GUS, Warsaw, p 27
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1 Descriptive statistics
Appendix 1 Descriptive statistics
Descriptive statistics | |||||
|---|---|---|---|---|---|
# | Min | Max | Mean | Std. Dev. | |
Year | 543 | 2000 | 2016 | 2007.97 | 4.44 |
Females at age 40 | 543 | 40.50 | 53.80 | 48.11 | 2.16 |
Females at age 60 | 543 | 21.80 | 34.10 | 28.55 | 1.95 |
Females at age 65 | 543 | 17.50 | 29.20 | 23.80 | 1.85 |
Females at age 80 | 543 | 7.00 | 14.70 | 10.87 | 1.30 |
Females at birth | 543 | 80.00 | 93.40 | 87.83 | 2.21 |
Males at age 40 | 543 | 18.10 | 44.13 | 32.55 | 4.59 |
Males at age 60 | 543 | 8.70 | 22.70 | 16.49 | 2.83 |
Males at age 65 | 543 | 7.60 | 18.70 | 13.29 | 2.23 |
Males at age 80 | 543 | 4.10 | 8.50 | 6.01 | 0.85 |
Males at birth | 543 | 51.80 | 78.90 | 69.95 | 5.36 |
Hospital beds | 543 | 29,161.76 | 1,839,205.16 | 177,310.09 | 337,038.83 |
Bad/very bad health, total aged 15+ | 543 | 1.41 | 27.21 | 10.59 | 5.36 |
Fair (not good, not bad) health, total aged 15+ | 543 | 6.90 | 51.80 | 23.00 | 8.70 |
Good/very good health, total aged 15+ | 543 | 28.49 | 189.82 | 129.99 | 30.82 |
Good/very good health, total aged 15+, High education (ISCED 5–8) | 543 | 38.40 | 102.06 | 79.68 | 11.27 |
Good/very good health, total aged 15+, Income quintile 1 (lowest) | 543 | 18.60 | 94.39 | 58.66 | 14.70 |
Good/very good health, total aged 15+, Income quintile 5 (highest) | 543 | 34.50 | 102.60 | 78.28 | 12.21 |
Good/very good health, total aged 15+, Low education (ISCED 0–2) | 543 | 14.95 | 87.30 | 55.10 | 13.23 |
Good/very good health, total aged 15+, Medium education (ISCED 3, 4) | 543 | 32.20 | 103.00 | 72.18 | 13.21 |
Good/very good health, total aged 15–24 | 543 | 45.50 | 112.70 | 89.34 | 8.82 |
Good/very good health, total aged 25–44 | 543 | 32.20 | 111.60 | 81.01 | 11.12 |
Good/very good health, total aged 45–64 | 543 | 15.21 | 96.79 | 60.48 | 17.08 |
Good/very good health, total aged 65+ | 543 | 22.43 | 88.30 | 39.37 | 20.80 |
Certain conditions originating in the perinatal period | 543 | 15,542.67 | 38,837.40 | 2718.35 | 6982.86 |
Certain infectious and parasitic diseases | 543 | 33,325.87 | 141,337.20 | 10,904.21 | 23,414.27 |
Complications of pregnancy, childbirth, and the puerperium | 543 | 567.31 | 1336.70 | 72.07 | 238.66 |
Congenital malformations and chromosomal abnormalities | 543 | 2811.15 | 21,395.90 | 2251.48 | 4541.72 |
Diseases of the blood and blood-forming organs | 543 | 168.79 | 21,396.10 | 2034.65 | 3745.68 |
Diseases of the circulatory system | 543 | 456,107.01 | 1,885,254.70 | 192,577.06 | 311,860.65 |
Diseases of the digestive system | 543 | 199.50 | 214,946.73 | 24,925.09 | 37,400.85 |
Diseases of the genitourinary system | 543 | 859.44 | 132,455.90 | 12,278.76 | 23,030.59 |
Diseases of the musculoskeletal system and connective tissue | 543 | 641.74 | 29,009.20 | 3057.99 | 5163.39 |
Diseases of the nervous system | 543 | 4793.00 | 331,357.80 | 20,119.95 | 46,550.37 |
Diseases of the respiratory system | 543 | 46,673.32 | 522,647.70 | 52,087.60 | 97,908.31 |
Diseases of the skin and subcutaneous tissue | 543 | 736.38 | 8922.50 | 967.83 | 1568.05 |
Endocrine, nutritional, and metabolic diseases | 543 | 282.03 | 246,692.06 | 22,167.65 | 44,707.85 |
External causes of mortality | 543 | 211.90 | 404,976.00 | 35,694.34 | 64,803.33 |
Malignant neoplasms | 543 | 1464.57 | 1,184,586.70 | 139,441.14 | 222,773.90 |
Neoplasms | 543 | 54,067.44 | 1,216,751.60 | 145,132.53 | 229,107.25 |
Symptoms, signs, ill-defined causes | 543 | 23,712.90 | 186,250.00 | 17,036.52 | 26,083.03 |
All causes of death | 543 | 627,557.82 | 5,257,809.20 | 544,431.65 | 901,221.76 |
Compensated absence from work due to illness | 543 | 25.61 | 30.37 | 11.86 | 5.39 |
Self-reported absence from work due to illness | 543 | 11.73 | 21.10 | 7.05 | 2.63 |
# of psychiatrists | 543 | 5552.25 | 45,961.74 | 4575.23 | 8170.39 |
# of physicians | 543 | 1476.86 | 820,251.00 | 91,586.48 | 141,759.22 |
# of pharmacists | 543 | 2742.50 | 295,620.92 | 30,329.61 | 56,478.56 |
# of nurses | 543 | 8301.09 | 22,108,726.56 | 1,343,730.45 | 3,288,910.41 |
# of midwives | 543 | 16,840.63 | 53,508.48 | 7207.68 | 11,722.67 |
For-profit, privately owned hospitals | 543 | 612.66 | 9385.71 | 398.43 | 753.62 |
General hospitals | 543 | 1414.00 | 8179.69 | 831.43 | 1544.66 |
# of hospitals | 543 | 1182.77 | 9259.09 | 1197.96 | 1903.85 |
Non-profit, privately owned hospitals | 543 | 422.80 | 4265.90 | 303.54 | 676.20 |
Publicly owned hospitals | 543 | 264.34 | 2422.29 | 419.16 | 442.80 |
# of dentists | 543 | 45,130.83 | 195,700.61 | 26,142.84 | 38,109.69 |
# of pediatricians | 543 | 996.75 | 81,209.15 | 5659.56 | 12,579.70 |
Computed tomography scanners, total | 543 | 260.24 | 13,818.87 | 886.67 | 2220.26 |
Digital subtraction angiography units, total | 543 | 474.86 | 3315.37 | 183.65 | 337.31 |
Gamma cameras, total | 543 | 213.61 | 15,951.02 | 343.07 | 1464.17 |
Lithotripters, total | 543 | 65.09 | 1115.03 | 81.87 | 173.12 |
MRI units, total | 543 | 238.72 | 12,554.00 | 581.77 | 1659.77 |
Mammographs, total | 543 | 272.59 | 15,200.22 | 1065.83 | 2626.92 |
PET scanners, total | 543 | 394.32 | 1650.13 | 64.18 | 201.92 |
Radiation therapy equipment, total | 543 | 544.96 | 3927.47 | 161.28 | 386.18 |
Rights and permissions
About this article
Cite this article
Raghupathi, V., Raghupathi, W. The association between healthcare resource allocation and health status: an empirical insight with visual analytics. J Public Health (Berl.) 31, 1035–1057 (2023). https://doi.org/10.1007/s10389-021-01651-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-021-01651-6