Abstract
Background
Sarcopenia is defined by low muscle mass and low muscle strength and is a prognostic factor of unfavorable outcomes in various diseases. The purpose of this study is to examine the correlation between skeletal muscle wasting (SMW) during neoadjuvant chemotherapy (NAC) and postoperative complications in patients with esophageal cancer, particularly in relation to anastomotic leakage.
Methods
The present study involved 99 patients with thoracic esophageal cancer and esophago-gastric junctional cancer who received NAC followed by radical esophagectomy between August 2008 to June 2019, and who were pStage 0–III. Patient demographics and clinical variables were retrospectively reviewed. For assessing the extent of SMW, the rate of change in skeletal muscle mass index (SMI) was measured from CT images at the level of the third lumbar vertebra. Factors associated with postoperative complications were also examined.
Results
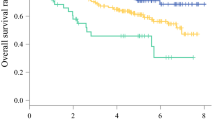
The median rate of change in total SMI in patients was − 1.87%. The decreased rates in SMI of the side abdominal muscles and rectus abdominis were significantly greater than that of the psoas major (side abdominal muscles: p = 0.0084, rectus abdominis: p = 0.036). Multivariate analysis showed a decreased rate in SMI, especially in the erector spinae muscle, and the Charlson comorbidity index (CCI) was significantly associated with Grade IIIa of higher anastomotic leakage (Grade ≥ IIIa) (SMI cutoff (favorable): ≤ − 7.84, p = 0.0040; CCI cutoff (favorable): ≥ 2, p = 0.0032).
Conclusion
In patients with esophageal cancer, SMI tend to decrease during NAC treatment. It is therefore important to prevent the additional impact that SMW during NAC has on postoperative anastomotic leakage.



Similar content being viewed by others
References
Takeda K, Umezawa R, Takahashi N, et al. Impact of change in serum albumin level during and after chemoradiotherapy in patients with locally advanced esophageal cancer. Esophagus. 2018;15:190–7.
Yin LX, Chen BM, Zhao GF, et al. Scoring system to predict the risk of surgical site infection in patients with esophageal cancer after esophagectomy with cervical anastomosis. Surg Infect (Larchmt). 2018;19:696–703.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in older people. Age Ageing. 2010;39:412–23.
Harada K, Ida S, Baba Y, et al. Prognostic and clinical impact of sarcopenia in esophageal squamous cell carcinoma. Dis Esophagus. 2016;29:627–33.
Elliott JA, Doyle SL, Murphy CF, et al. Sarcopenia: prevalence, and impact on operative and oncologic outcomes in the multimodal management of locally advanced esophageal cancer. Ann Surg. 2017;266:822–30.
Yohei O, Toru N, Yusuke T, et al. Evaluation of the impact of psoas muscle index, a parameter of sarcopenia, in patients with esophageal squamous cell carcinoma receiving neoadjuvant therapy. Esophagus. 2019;16:345–51.
Begini P, Gigante E, Antonelli G, et al. Sarcopenia predicts reduced survival in patients with hepatocellular carcinoma at first diagnosis. Ann Hepatol. 2017;16:107–14.
Ninomiya G, Fujii T, Yamada S, Yabusaki N, et al. Clinical impact of sarcopenia on prognosis in pancreatic ductal adenocarcinoma: a retrospective cohort study. Int J Surg. 2017;39:45–51.
Anker SD, Coats AJ, Morley JE, et al. Muscle wasting disease: a proposal for a new disease classification. J Cachexia Sarcopenia Muscle. 2014;5:1–3.
Ando N, Kato H, Igaki H, Shinoda M, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19:68–74.
van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074–84.
Ida S, Watanabe M, Karashima R, et al. Changes in body composition secondary to neoadjuvant chemotherapy for advanced esophageal cancer are related to the occurrence of postoperative complications after esophagectomy. Ann Surg Oncol. 2014;21:3675–9.
Schizas D, Frountzas M, Lidoriki I, et al. Sarcopenia does not affect postoperative complication rates in oesophageal cancer surgery: a systematic review and meta-analysis. Ann R Coll Surg Engl. 2019;11:1–13.
Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 2. Esophagus. 2019;16:25–43.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: part I. Esophagus. 2017;14:1–36.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–5.
Martin L, Lagergren J, Lindblad M, et al. Malnutrition after oesophageal cancer surgery in Sweden. Br J Surg. 2007;94:1496–500.
Backemar L, Lagergren P, Djärv T, et al. Comorbidities and risk of complications after surgery for esophageal cancer: a Nationwide Cohort Study in Sweden. World J Surg. 2015;39:2282–8.
Gronnier C, Tréchot B, Duhamel A, et al. Impact of neoadjuvant chemoradiotherapy on postoperative outcomes after esophageal cancer resection: results of a European multicenter study. Ann Surg. 2014;260:761–4.
Michelet P, D'Journo X-B, Roch A, et al. Perioperative risk factors for anastomotic leakage after esophagectomy: influence of thoracic epidural analgesia. Chest. 2005;128:3461–6.
Wang Y, Yuqi M, Mingjian L, et al. Impact of type 2 diabetes mellitus on short-term and long-term outcomes of patients with esophageal squamous cell cancer undergoing resection: a propensity score analysis. Cancer Commun (Lond). 2018;38:14.
Kassis ES, Kosinski AS, Ross PJ, et al. Predictors of anastomotic leak after esophagectomy: an analysis of the Society of Thoracic Surgeons General Thoracic Database. Ann Thorac Surg. 2013;96:1919–26.
Ercan S, Rice TW, Murthy SC, et al. Does esophagogastric anastomotic technique influence the outcome of patients with esophageal cancer? J Thorac Cardiovasc Surg. 2005;129:623–31.
Sugimura K, Miyata H, Matsunaga T, et al. Comparison of the modified Collard and hand-sewn anastomosis for cervical esophagogastric anastomosis after esophagectomy in esophageal cancer patients: a propensity score-matched analysis. Ann Gastroenterol Surg. 2018;3:104–13.
Haverkamp L, van der Sluis PC, Verhage RJJ, et al. End-to-end cervical esophagogastric anastomoses are associated with a higher number of strictures compared with end-to-side anastomoses. J Gastrointest Surg. 2013;17:872–6.
Kataoka K, Takeuchi H, Mizusawa J, et al. Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg. 2017;265:1152–7.
Saeterbakken AH, Fimland MS. Muscle activity of the core during bilateral, unilateral, seated and standing resistance exercise. Eur J Appl Physiol. 2012;112:1671–8.
Callaghan JP, McGill SM. Low back joint loading and kinematics during standing and unsupported sitting. Ergonomics. 2001;44:280–94.
Kippers V, Parker AW. Electromyographic studies of erectors spinae: symmetrical postures and sagittal trunk motion. Aust J Physiother. 1985;31:95–105.
Standring S, editor. Gray’s anatomy: the anatomical basis of clinical practice. London: Churchill Livingstone; 2008.
Yoshio M, Murakami G, Sato T, et al. The function of the psoas major muscle: passive kinetics and morphological studies using donated cadavers. J Orthop Sci. 2002;7:199–207.
Belavý DL, Armbrecht G, Richardson CA, et al. Muscle atrophy and changes in spinal morphology: is the lumbar spine vulnerable after prolonged bed-rest? Spine (Phila Pa 1976). 2011;36:137–45.
Tanimura K, Sato S, Sato A, et al. Accelerated loss of antigravity muscles is associated with mortality in patients with COPD. Respiration. 2020;99:298–306.
Akiko N, Hirotsugu O, Hiroyuki T, et al. Early decrease in erector spinae muscle area and future risk of mortality in idiopathic pulmonary fibrosis. Sci Rep. 2020;11:2312.
Read JA, Beale PJ, Volker DH, et al. Nutrition intervention using an eicosapentaenoic acid (EPA) containing supplement in patients with advanced colorectal cancer. Effects on nutritional and inflammatory status: a phase II trial. Support Care Cancer. 2007;15:301–7.
Gonçalves Dias MC, de Fátima NMM, et al. Nutritional intervention improves the caloric and proteic ingestion of head and neck cancer patients under radiotherapy. Nutr Hosp. 2005;20:320–5.
Vikberg S, Sörlén N, Brandén L, et al. Effects of resistance training on functional strength and muscle mass in 70-year-old individuals with pre-sarcopenia: a randomized controlled trial. J Am Med Dir Assoc. 2019;20:28–34.
Pedersen BK, Akerstrom TC, Nielsen AR, et al. Role of myokines in exercise and metabolism. J Appl Physiol. 2007;103:1093–8.
Pedersen BK, Fischer CP. Beneficial health effects of exercise–the role of IL-6 as a myokine. Trends Pharmacol Sci. 2007;28:152–6.
Adams GR. Autocrine/paracrine IGF-I and skeletal muscle adaptation. J Appl Physiol. 2001;93:1159–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
All procedures of this study were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fujihata, S., Ogawa, R., Nakaya, S. et al. The impact of skeletal muscle wasting during neoadjuvant chemotherapy on postoperative anastomotic leakage in patients with esophageal cancer. Esophagus 18, 258–266 (2021). https://doi.org/10.1007/s10388-020-00774-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00774-1