Abstract
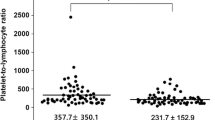
This study aimed to elucidate the immune status of systemic lupus erythematosus (SLE) patients with infections. We enrolled 253 SLE patients including 77 patients with infections. Clinical features and immunological parameters were analyzed, with particular reference to neutrophil CD64 (nCD64) expression, myeloid-derived suppressor cells (MDSCs), activated T cells and multiple cytokines. Among the 77 SLE patients with infections, 32 patients (41.56%) developed fever and 20 patients (25.97%) developed serositis, which were higher compared to the non-infection group. A considerably higher level of nCD64 was found in the infection group (4.65 vs 1.01, P < 0.001). In addition, the infection group exhibited higher percentages of total MDSCs (6.99 vs 4.30%, P = 0.003), polymorphonuclear MDSCs (PMN-MDSCs) (P = 0.032) and monocytic MDSCs (M-MDSCs) (P = 0.015). T cells were more activated during infections, with an elevated level of IL-2R (P < 0.001). Specifically, higher percentages of CD4+CD38+ T cells (55.73 vs 50.17%, P = 0.036), CD8+HLA-DR+ T cells (59.82 vs 47.99%, P < 0.001) and CD8+CD38+ T cells (68.59 vs 63.90%, P = 0.044) were identified in the infection group. Furthermore, the serum levels of IL-6, IL-8 and IL-10 were elevated in the infection group (all P < 0.001). Higher proportions of neutrophils, CD4+ and CD8+ T cells, and MDSCs were activated during infections in SLE patients. Additionally, the serum cytokines altered during infections, with noticeably elevated levels of IL-6, IL-8 and IL-10. Infections may lead to the amplification of immune alterations in SLE.








Similar content being viewed by others
Data availability
The data used during the study are available on reasonable request.
References
Tsokos GC. Autoimmunity and organ damage in systemic lupus erythematosus. Nat Immunol. 2020;21(6):605–14.
Crow MK. Pathogenesis of systemic lupus erythematosus: risks, mechanisms and therapeutic targets. Ann Rheum Dis. 2023.
Kaul A, Gordon C, Crow MK, et al. Systemic lupus erythematosus. Nat Rev Dis Primers. 2016;2:16039.
He J, Li Z. Dilemma of immunosuppression and infection risk in systemic lupus erythematosus. Rheumatology (Oxford). 2023;62(Suppl 1):i22–9.
Dörner T, Furie R. Novel paradigms in systemic lupus erythematosus. Lancet. 2019;393(10188):2344–58.
Goldblatt F, Chambers S, Rahman A, Isenberg DA. Serious infections in British patients with systemic lupus erythematosus: hospitalisations and mortality. Lupus. 2009;18(8):682–9.
Dias AMB, do Couto MCM, Duarte CCM, Inês LPB, Malcata AB. White blood cell count abnormalities and infections in one-year follow-up of 124 patients with SLE. Ann N Y Acad Sci. 2009;1173:103–7.
Goldblatt F, Yuste J, Isenberg DA, Rahman A, Brown J. Impaired C3b/iC3b deposition on Streptococcus pneumoniae in serum from patients with systemic lupus erythematosus. Rheumatology (Oxford). 2009;48(12):1498–501.
Paton NI, Cheong IK, Kong NC, Segasothy M. Risk factors for infection in Malaysian patients with systemic lupus erythematosus. QJM. 1996;89(7):531–8.
Noël V, Lortholary O, Casassus P, et al. Risk factors and prognostic influence of infection in a single cohort of 87 adults with systemic lupus erythematosus. Ann Rheum Dis. 2001;60(12):1141–4.
Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, Martinez-Berriotxoa A, Egurbide M-V, Aguirre C. Predictors of major infections in systemic lupus erythematosus. Arthritis Res Ther. 2009;11(4):R109.
Hochberg MC. Updating the American College of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725.
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European organization for research and treatment of cancer/invasive fungal infections cooperative group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–21.
Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2020;71(6):1367–76.
Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29(2):288–91.
Olivares-Zavaleta N, Carmody A, Messer R, Whitmire WM, Caldwell HD. Chlamydia pneumoniae inhibits activated human T lymphocyte proliferation by the induction of apoptotic and pyroptotic pathways. J Immunol. 2011;186(12):7120–6.
Poujol F, Monneret G, Pachot A, Textoris J, Venet F. Altered T lymphocyte proliferation upon lipopolysaccharide challenge ex vivo. PLoS ONE. 2015;10(12): e0144375.
Merayo-Chalico J, Gómez-Martín D, Piñeirúa-Menéndez A, Santana-De Anda K, Alcocer-Varela J. Lymphopenia as risk factor for development of severe infections in patients with systemic lupus erythematosus: a case-control study. QJM. 2013;106(5):451–7.
Repp R, Valerius T, Sendler A, et al. Neutrophils express the high affinity receptor for IgG (Fc gamma RI, CD64) after in vivo application of recombinant human granulocyte colony-stimulating factor. Blood. 1991;78(4):885–9.
Davis BH, Olsen SH, Ahmad E, Bigelow NC. Neutrophil CD64 is an improved indicator of infection or sepsis in emergency department patients. Arch Pathol Lab Med. 2006;130(5):654–61.
Yeh C-F, Wu C-C, Liu S-H, Chen K-F. Comparison of the accuracy of neutrophil CD64, procalcitonin, and C-reactive protein for sepsis identification: a systematic review and meta-analysis. Ann Intensive Care. 2019;9(1):5.
Cid J, Aguinaco R, Sánchez R, García-Pardo G, Llorente A. Neutrophil CD64 expression as marker of bacterial infection: a systematic review and meta-analysis. J Infect. 2010;60(5):313–9.
Burn GL, Foti A, Marsman G, Patel DF, Zychlinsky A. The neutrophil. Immunity. 2021;54(7):1377–91.
Rahman S, Sagar D, Hanna RN, et al. Low-density granulocytes activate T cells and demonstrate a non-suppressive role in systemic lupus erythematosus. Ann Rheum Dis. 2019;78(7):957–66.
Florez-Pollack S, Tseng L-C, Kobayashi M, Hosler GA, Ariizumi K, Chong BF. Expansion of myeloid-derived suppressor cells in the peripheral blood and Lesional skin of cutaneous lupus patients. J Invest Dermatol. 2019;139(2):478–81.
Veglia F, Sanseviero E, Gabrilovich DI. Myeloid-derived suppressor cells in the era of increasing myeloid cell diversity. Nat Rev Immunol. 2021;21(8):485–98.
Hollen MK, Stortz JA, Darden D, et al. Myeloid-derived suppressor cell function and epigenetic expression evolves over time after surgical sepsis. Crit Care. 2019;23(1):355.
Mathias B, Delmas AL, Ozrazgat-Baslanti T, et al. Human myeloid-derived suppressor cells are associated with chronic immune suppression after severe sepsis/septic shock. Ann Surg. 2017;265(4):827–34.
Katsuyama E, Suarez-Fueyo A, Bradley SJ, et al. The CD38/NAD/SIRTUIN1/EZH2 axis mitigates cytotoxic CD8 T cell function and identifies patients with SLE prone to infections. Cell Rep. 2020;30(1):112-123.e4.
Li Z, Yang Z, Hu P, et al. Cytokine expression of lung bacterial infection in newly diagnosed adult hematological malignancies. Front Immunol. 2021;12: 748585.
Rose-John S, Winthrop K, Calabrese L. The role of IL-6 in host defence against infections: immunobiology and clinical implications. Nat Rev Rheumatol. 2017;13(7):399–409.
Hunter CA, Jones SA. IL-6 as a keystone cytokine in health and disease. Nat Immunol. 2015;16(5):448–57.
Kang S, Kishimoto T. Interplay between interleukin-6 signaling and the vascular endothelium in cytokine storms. Exp Mol Med. 2021;53(7):1116–23.
Yang J, Hooper WC, Phillips DJ, Talkington DF. Cytokines in Mycoplasma pneumoniae infections. Cytokine Growth Factor Rev. 2004;15(2–3):157–68.
Ouyang W, O’Garra A. IL-10 family cytokines IL-10 and IL-22: from basic science to clinical translation. Immunity. 2019;50(4):871–91.
Preble OT, Black RJ, Friedman RM, Klippel JH, Vilcek J. Systemic lupus erythematosus: presence in human serum of an unusual acid-labile leukocyte interferon. Science. 1982;216(4544):429–31.
Mathian A, Mouries-Martin S, Dorgham K, et al. Ultrasensitive serum interferon-α quantification during SLE remission identifies patients at risk for relapse. Ann Rheum Dis. 2019;78(12):1669–76.
Acknowledgements
We are very grateful to Dr Shi Bisheng and Dr Ma Xiaowei from Department of Laboratory Medicine, Renji Hospital, School of Medicine, Shanghai Jiaotong University for flow cytometry analysis. We thank the patients and their families for their cooperation.
Funding
This work was supported by the National Natural Science Foundation of China (82001707 and 81373209), Shanghai Sailing Program (22YF1424000 and 20YF1425700), and the Fundamental Research Funds for the Central Universities (YG2023ZD09).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. RG and LL designed the study and revised the manuscript. LZ and LG drafted the manuscript. LT and XL collected and analysed clinical data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Written informed consent for publication of the study was obtained from all individual participants included in the study. All authors approved the final manuscript.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Renji Hospital (Number: [2017]201), Shanghai, China.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhi, L., Gu, L., Tong, L. et al. Immune profile alterations of systemic lupus erythematosus patients with infections. Clin Exp Med 23, 4765–4777 (2023). https://doi.org/10.1007/s10238-023-01220-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01220-z