Abstract
Background
Family history of gout and sex are independently associated with gout. However, there is a paucity of research regarding the joint role of both factors in gout pathogenesis. Therefore, we assessed the independent and combined association of family history of gout and sex with gout.
Methods
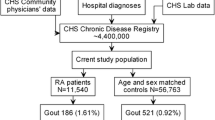
Our analysis included 132,311 Taiwan Biobank (TWB)-enrolled individuals comprising 21,159 gout cases and 111,152 controls. We subcategorized the family history of gout as (1) both siblings and parents had gout), (2) only parents had gout, and (3) only siblings had gout.
Results
Generally, sex (men compared to women) and family history of gout were independently associated with a higher risk of gout. The odds ratio (OR); 95% confidence interval (CI) was 9.175; 8.801–9.566 for sex, and 2.306; 2.206–2.410 for family history. For the subcategories ‘both siblings and had gout,’ ‘only parents had gout,’ and ‘only siblings had gout,’ the odds ratios (ORs); 95% confidence intervals (CIs) were 4.944; 4.414–5.538, 2.041; 1.927–2.161, and 2.162; 2.012–2.323, respectively. The interaction between sex and family history was significant (p value = 0.0001). After stratification by sex, family history of gout remained significantly associated with a higher risk of gout in both sexes, even though the odds ratios were higher in men. For the subcategories ‘both siblings and parents had gout,’ ‘only parent had gout,’ and ‘only siblings had gout,’ the corresponding ORs; 95% CIs were 6.279; 5.243–7.520, 2.211; 2.062–2.371, and 2.148; 1.955–2.361 in men and 4.199; 3.566–4.945, 1.827; 1.640–2.035, and 2.093; 1.876–2.336 in women. After integrating sex and family history (reference: women with no family history), the highest risk of gout was observed in men who had at least one parent and sibling with a history of gout (OR; 95% CI 55.774; 46.360–67.101).
Conclusion
Sex and family history of gout were independently and interactively associated with gout. Sex-wise, men had a higher risk of gout than women. Family history was associated with a higher risk of gout in both sexes, but men had a higher risk. Notably, men having both siblings and parents with gout had the highest risk of gout.
Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from Taiwan Biobank but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author, Prof. Yung-Po Liaw upon reasonable request and with permission of Taiwan Biobank.
References
MacFarlane LA, Kim SC. Gout: a review of nonmodifiable and modifiable risk factors. Rheum Dis Clin. 2014;40(4):581–604.
Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: Fifty-two-year followup of a prospective cohort. Arthritis Rheum. 2010;62(4):1069–76.
Trifirò G, Morabito P, Cavagna L, et al. Epidemiology of gout and hyperuricaemia in Italy during the years 2005–2009: a nationwide population-based study. Ann Rheum Dis. 2013;72(5):694–700.
Kopke A, Greeff OB. Hyperuricaemia and gout. S Afr Fam Pract. 2015;57(1):6–12.
Singh JA, Reddy SG, Kundukulam J. Risk factors for gout and prevention: a systematic review of the literature. Curr Opin Rheumatol. 2011;23(2):192.
Lin K-C, Lin H, Chou P. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J Rheumatol. 2000;27(6):1501–5.
Li-Yu J, Clayburne G, Sieck M, et al. Treatment of chronic gout. Can we determine when urate stores are depleted enough to prevent attacks of gout? J Rheumatol. 2001;28(3):577–80.
Gao Q, Cheng X, Merriman TR, et al. Trends in the manifestations of 9754 gout patients in a Chinese clinical center: a 10-year observational study. Joint Bone Spine. 2021;88(6): 105078.
Roddy E, Doherty M. Gout. Epidemiology of gout. Arthritis Res Ther. 2010;12(6):1–11.
Annemans L, Spaepen E, Gaskin M, et al. Gout in the UK and Germany: prevalence, comorbidities and management in general practice 2000–2005. Ann Rheum Dis. 2008;67(7):960–6.
Padang C, Muirden KD, Schumacher HR, Darmawan J, Nasution AR. Characteristics of chronic gout in Northern Sulawesi, Indonesia. J Rheumatol. 2006;33(9):1813–7.
Wu EQ, Patel PA, Mody RR, et al. Frequency, risk, and cost of gout-related episodes among the elderly: does serum uric acid level matter? J Rheumatol. 2009;36(5):1032–40.
Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol. 2004;31(8):1582–7.
Wang W, Krishnan E. Cigarette smoking is associated with a reduction in the risk of incident gout: results from the Framingham Heart Study original cohort. Rheumatology. 2015;54(1):91–5.
Dehlin M, Jacobsson L, Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. 2020;16(7):380–90.
Singh JA, Gaffo A. Gout epidemiology and comorbidities. Sem Arthritis Rheum. 2020;50:S11–6.
Lyu L-C, Hsu C-Y, Yeh C-Y, Lee M-S, Huang S-H, Chen C-L. A case-control study of the association of diet and obesity with gout in Taiwan. Am J Clin Nutr. 2003;78(4):690–701.
Chuang S-Y, Lee S-C, Hsieh Y-T, Pan W-H. Trends in hyperuricemia and gout prevalence: Nutrition and Health Survey in Taiwan from 1993–1996 to 2005–2008. Asia Pac J Clin Nutr. 2011;20(2):301–8.
Lin K-C, Lin H-Y, Chou P. Community based epidemiological study on hyperuricemia and gout in Kin-Hu, Kinmen. J Rheumatol. 2000;27(4):1045–50.
Harrold LR, Etzel CJ, Gibofsky A, et al. Sex differences in gout characteristics: tailoring care for women and men. BMC Musculoskelet Disord. 2017;18(1):1–6.
Harrold LR, Yood RA, Mikuls TR, et al. Sex differences in gout epidemiology: evaluation and treatment. Ann Rheum Dis. 2006;65(10):1368–72.
De Souza AW, Fernandes V, Ferrari AJ. Female gout: clinical and laboratory features. J Rheumatol. 2005;32(11):2186–8.
Zitt E, Fischer A, Lhotta K, Concin H, Nagel G. Sex-and age-specific variations, temporal trends and metabolic determinants of serum uric acid concentrations in a large population-based Austrian cohort. Sci Rep. 2020;10(1):1–8.
Evans PL, Prior JA, Belcher J, Hay CA, Mallen CD, Roddy E. Gender-specific risk factors for gout: a systematic review of cohort studies. Adv Rheumatol. 2019. https://doi.org/10.1186/s42358-019-0067-7.
Vitart V, Rudan I, Hayward C, et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet. 2008;40(4):437–42.
Dehghan A, Köttgen A, Yang Q, et al. Association of three genetic loci with uric acid concentration and risk of gout: a genome-wide association study. The Lancet. 2008;372(9654):1953–61.
Köttgen A, Albrecht E, Teumer A, et al. Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat Genet. 2013;45(2):145–54.
Wang WH, Chang SJ, Wang TN, et al. Complex segregation and linkage analysis of familial gout in Taiwanese aborigines. Arthritis Rheum. 2004;50(1):242–6.
Krishnan E, Lessov-Schlaggar CN, Krasnow RE, Swan GE. Nature versus nurture in gout: a twin study. Am J Med. 2012;125(5):499–504.
Wilk JB, Djousse L, Borecki I, et al. Segregation analysis of serum uric acid in the NHLBI Family Heart Study. Hum Genet. 2000;106(3):355–9.
Emmerson B, Nagel S, Duffy D, Martin N. Genetic control of the renal clearance of urate: a study of twins. Ann Rheum Dis. 1992;51(3):375–7.
Chang S, Ko YC, Wang T, Chang F, Cinkotai F, Chen C. High prevalence of gout and related risk factors in Taiwan’s Aborigines. J Rheumatol. 1997;24(7):1364–9.
Chou C, Lai J. The epidemiology of hyperuricaemia and gout in Taiwan aborigines. Br J Rheumatol. 1998;37(3):258–62.
Chandratre P, Roddy E, Clarson L, Richardson J, Hider SL, Mallen CD. Health-related quality of life in gout: a systematic review. Rheumatology. 2013;52(11):2031–40.
Kuo C-F, Grainge MJ, See L-C, et al. Epidemiology and management of gout in Taiwan: a nationwide population study. Arthritis Res Ther. 2015;17(1):1–10.
Yu KH, Luo SF. Younger age of onset of gout in Taiwan. Rheumatology. 2003;42(1):166–70.
Kuo C-F, Grainge MJ, See L-C, et al. Familial aggregation of gout and relative genetic and environmental contributions: a nationwide population study in Taiwan. Ann Rheum Dis. 2015;74(2):369–74.
Chen S-Y, Chen C-L, Shen M-L, Kamatani N. Clinical features of familial gout and effects of probable genetic association between gout and its related disorders. Metabol Clin Exp. 2001;50(10):1203–7.
Feng Y-CA, Chen C-Y, Chen T-T, et al. Taiwan Biobank: a rich biomedical research database of the Taiwanese population. Cell Genom. 2022;2(11):100197–9.
Fan C-T, Lin J-C, Lee C-H. Taiwan Biobank: a project aiming to aid Taiwan’s transition into a biomedical island. Pharmacogenomics. 2008;9:235–46.
Tsai H-H, Shen C-Y, Ho C-C, et al. Interaction between a diabetes-related methylation site (TXNIP cg19693031) and variant (GLUT1 rs841853) on fasting blood glucose levels among non-diabetics. J Transl Med. 2022;20(1):1–9.
Hsu T-L, Tantoh DM, Chou Y-H, et al. Association between osteoporosis and menopause in relation to SOX6 rs297325 variant in Taiwanese women. Menopause (New York, NY). 2020;27(8):887.
Liu C-S, Li T-C, Lin C-C. The epidemiology of hyperuricemia in children of Taiwan aborigines. J Rheumatol. 2003;30(4):841–5.
Lu X, Li X, Zhao Y, Zheng Z, Guan S, Chan P. Contemporary epidemiology of gout and hyperuricemia in community elderly in Beijing. Int J Rheum Dis. 2014;17(4):400–7.
Chen S-Y, Shen M-L. Juvenile gout in Taiwan associated with family history and overweight. J Rheumatol. 2007;34(11):2308–11.
Wang Y, Yan S, Li C, et al. Risk factors for gout developed from hyperuricemia in China: a five-year prospective cohort study. Rheumatol Int. 2013;33(3):705–10.
Mohd A, Das Gupta E, Loh Y, Gandhi C, D’souza B, Gun S. Clinical characteristics of gout: a hospital case series. Malays Fam Physician. 2011;6(2–3):72.
Choi HK, Atkinson K, Karlson EW, Curhan G. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Arch Intern Med. 2005;165(7):742–8.
Nicholls A, Snaith M, Scott J. Effect of oestrogen therapy on plasma and urinary levels of uric acid. Br Med J. 1973;1(5851):449–51.
Sumino H, Ichikawa S, Kanda T, Nakamura T, Sakamaki T. Reduction of serum uric acid by hormone replacement therapy in postmenopausal women with hyperuricaemia. The Lancet. 1999;354(9179):650.
Hak AE, Choi HK. Menopause, postmenopausal hormone use and serum uric acid levels in US women—the Third National Health and Nutrition Examination Survey. Arthritis Res Ther. 2008;10(5):1–7.
Hak AE, Curhan GC, Grodstein F, Choi HK. Menopause, postmenopausal hormone use and risk of incident gout. Ann Rheum Dis. 2010;69(7):1305–9.
Yahyaoui R, Esteva I, Haro-Mora J, et al. Effect of long-term administration of cross-sex hormone therapy on serum and urinary uric acid in transsexual persons. J Clin Endocrinol Metab. 2008;93(6):2230–3.
McCormick N, Rai SK, Lu N, Yokose C, Curhan GC, Choi HK. Estimation of primary prevention of gout in men through modification of obesity and other key lifestyle factors. JAMA Netw Open. 2020;3(11):e2027421–e2027421.
Soriano LC, Rothenbacher D, Choi HK, Rodríguez LAG. Contemporary epidemiology of gout in the UK general population. Arthritis Res Ther. 2011;13(2):1–9.
Williams PT. Effects of diet, physical activity and performance, and body weight on incident gout in ostensibly healthy, vigorously active men. Am J Clin Nutr. 2008;87(5):1480–7.
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Alcohol intake and risk of incident gout in men: a prospective study. The Lancet. 2004;363(9417):1277–81.
Wang M, Jiang X, Wu W, Zhang D. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol. 2013;32(11):1641–8.
Zhang Y, Woods R, Chaisson CE, et al. Alcohol consumption as a trigger of recurrent gout attacks. Am J Med. 2006;119(9):800.e811-800.e816.
Maclachlan MJ, Rodnan GP. Effects of food, fast and alcohol on serum uric acid and acute attacks of gout. Am J Med. 1967;42(1):38–57.
Kim Y, Kang J. Association of urinary cotinine-verified smoking status with hyperuricemia: Analysis of population-based nationally representative data. Tobacco Induced Dis. 2020;18:1–10.
Hanna BE, Hamed JM, Touhala LM. Serum uric Acid in smokers. Oman Med J. 2008;23(4):269.
Tsuchiya M, Asada A, Kasahara E, Sato EF, Shindo M, Inoue M. Smoking a single cigarette rapidly reduces combined concentrations of nitrate and nitrite and concentrations of antioxidants in plasma. Circulation. 2002;105(10):1155–7.
Janssens HJ, van de Lisdonk EH, Janssen M, van den Hoogen HJ, Verbeek AL. Gout, not induced by diuretics? A case-control study from primary care. Ann Rheum Dis. 2006;65(8):1080–3.
Acknowledgements
Not applicable.
Funding
The Ministry of Science and Technology (MOST), Taiwan funded our study (MOST 111-2121-M-040-002).
Author information
Authors and Affiliations
Contributions
H-HT, DMT, C-HH, J-HZ, C-YC, and Y-PL did the literature search, conceived, and designed the study. C-HH, J-HZ, and Y-PL analyzed the data. H-HT, DMT, and C-YC drafted the manuscript. DMT edited the paper. All the authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The Institutional Review Board (IRB) of the Chung Shan Medical University Hospital granted ethical approval for this study (IRB: CS1-20009). Each participant signed an informed consent letter before enrolling in the Taiwan Biobank project. All methods were carried out in accordance with relevant guidelines and regulations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsai, HH., Tantoh, D.M., Hsiao, CH. et al. Risk of gout in Taiwan Biobank participants pertaining to their sex and family history of gout among first-degree relatives. Clin Exp Med 23, 5315–5325 (2023). https://doi.org/10.1007/s10238-023-01167-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01167-1