Abstract
Secondary acute myeloid leukemia (sAML) may develop following a prior therapy or may evolve from an antecedent hematological disorder such as Fanconi Anemia (FA). Pathophysiology of leukemic evolution is not clear. Etoposide (Eto) is a chemotherapeutic agent implicated in development of sAML. FA is an inherited bone marrow (BM) failure disease characterized by genomic instability and xenobiotic susceptibility. Here, we hypothesized that alterations in the BM niche may play a critical/driver role in development of sAML in both conditions. Expression of selected genes involved in xenobiotic metabolism, DNA double-strand break response, endoplasmic reticulum (ER) stress, heat shock response and cell cycle regulation were determined in BM mesenchymal stem cells (MSCs) of healthy controls and FA patients at steady state and upon exposure to Eto at different concentrations and in recurrent doses. Expression of CYPA1, p53, CCNB1, Dicer1, CXCL12, FLT3L and TGF-Beta genes were significantly downregulated in FA-MSCs compared with healthy controls. Eto exposure induced significant alterations in healthy BM-MSCs with increased expression of CYP1A1, GAD34, ATF4, NUPR1, CXCL12, KLF4, CCNB1 and nuclear localization of Dicer1. Interestingly, FA-MSCs did not show significant alterations in these genes upon Eto exposure. As opposed to healthy MSCs DICER1 gene expression and intracellular localization was not altered on FA BM-MSCs after Eto treatment. These results showed that Eto is a highly potent molecule and has pleiotropic effects on BM-MSCs, FA cells show altered expression profile compared to healthy controls and Eto exposure on FA cells shows differential profile than healthy controls.
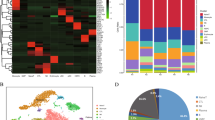
Graphical abstract







Similar content being viewed by others
Change history
09 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10238-023-01175-1
Abbreviations
- sAML:
-
Secondary acute myeloid leukemia
- AML:
-
Acute myeloid leukemia
- BM:
-
Bone marrow
- BrDU:
-
Bromodeoksiüridin
- DSB:
-
Double-strand breaks
- Eto:
-
Etoposide
- FA:
-
Fanconi anemia
- HSC:
-
Hematopoietic stem cell
- MSC:
-
Mesenchymal stem cell
- SA-Beta-Gal:
-
Senescence associated beta-galactosidase
References
Spees JL, Lee RH, Gregory CA. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res Ther. 2016;7(1):125.
Li AJ, Calvi LM. The microenvironment in myelodysplastic syndromes: Niche-mediated disease initiation and progression. Exp Hematol. 2017;55:3–18.
Brenner AK, Nepstad I, Bruserud O. Mesenchymal stem cells support survival and proliferation of primary human acute myeloid Leukemia cells through heterogeneous molecular mechanisms. Front Immunol. 2017;8:106.
Uçkan-Çetinkaya D., Muratoglu B., Response of the bone marrow stem cells and the microenvironment to stress. Handbook of stem cell therapy; 2022. p. 1–51.
Walkley CR, Shea CR, Sims NA, Purton LE, Orkin SH. Rb regulates interactions between hematopoietic stem cells and their bone marrow microenvironment. Cell. 2007;129(6):1081–95.
Raaijmakers MH, Mukherjee S, Guo S, et al. Bone progenitor dysfunction induces myelodysplasia and secondary leukaemia. Nature. 2010;464(7290):852–7.
Leimkuhler NB, Schneider RK. Inflammatory bone marrow microenvironment. Hematol Am Soc Hematol Educ Prog. 2019;2019(1):294–302.
Shallis RM, Weiss JJ, Deziel NC, Gore SD. Challenging the concept of de novo acute myeloid leukemia: Environmental and occupational leukemogens hiding in our midst. Blood Rev. 2021;47:100760.
Park M, Park CJ, Cho YW, et al. Alterations in the bone marrow microenvironment may elicit defective hematopoiesis: a comparison of aplastic anemia, chronic myeloid leukemia, and normal bone marrow. Exp Hematol. 2017;45:56–63.
Ezoe S. Secondary leukemia associated with the anti-cancer agent, etoposide, a topoisomerase II inhibitor. Int J Environ Res Public Health. 2012;9(7):2444–53.
Winick NJ, McKenna RW, Shuster JJ, et al. Secondary acute myeloid leukemia in children with acute lymphoblastic leukemia treated with etoposide. J Clin Oncol. 1993;11(2):209–17.
Weintraub M, Revel-Vilk S, Charit M, Aker M, Pe’er J. Secondary acute myeloid leukemia after etoposide therapy for retinoblastoma. J Pediatr Hematol Oncol. 2007;29(9):646–8.
Kourtis N, Tavernarakis N. Cellular stress response pathways and ageing: intricate molecular relationships. EMBO J. 2011;30(13):2520–31.
Hidaka T, Fujimura T, Aiba S. Aryl hydrocarbon receptor modulates carcinogenesis and maintenance of skin cancers. Front Med (Lausanne). 2019;6:194.
Carrancio S, Blanco B, Romo C, et al. Bone marrow mesenchymal stem cells for improving hematopoietic function: an in vitro and in vivo model. Part 2: Effect on bone marrow microenvironment. PLoS One. 2011;6(10):e26241.
Alessio N, Aprile D, Cappabianca S, Peluso G, Di Bernardo G, Galderisi U. Different stages of quiescence, senescence, and cell stress identified by molecular algorithm based on the expression of ki67, rps6, and beta-galactosidase activity. Int J Mol Sci. 2021;22(6):3102.
Nepal M, Che R, Zhang J, Ma C, Fei P. Fanconi anemia signaling and cancer. Trends Cancer. 2017;3(12):840–56.
Nicolay NH, Ruhle A, Perez RL, et al. Mesenchymal stem cells exhibit resistance to topoisomerase inhibition. Cancer Lett. 2016;374(1):75–84.
Wu Y, Wang Z, Cao Y, et al. Cotransplantation of haploidentical hematopoietic and umbilical cord mesenchymal stem cells with a myeloablative regimen for refractory/relapsed hematologic malignancy. Ann Hematol. 2013;92(12):1675–84.
Aqmasheh Shamsasanjan K, Akbarzadehlaleh P, Pashoutan Sarvar D, et al. Effects of mesenchymal stem cell derivatives on hematopoiesis and hematopoietic stem cells. Adv Pharm Bull. 2017;7(2):165–77.
Fajardo-Orduna GR, Mayani H, Montesinos JJ. Hematopoietic support capacity of mesenchymal stem cells: biology and clinical potential. Arch Med Res. 2015;46(8):589–96.
Savage SA, Walsh MF. Myelodysplastic syndrome, acute myeloid leukemia, and cancer surveillance in fanconi anemia. Hematol Oncol Clin North Am. 2018;32(4):657–68.
Xu J, Li X, Cole A, Sherman Z, Du W. Reduced cell division control protein 42 activity compromises hematopoiesis-supportive function of fanconi anemia mesenchymal stromal cells. Stem Cells. 2018;36(5):785–95.
Cagnan I, Keles M, Keskus AG, et al. Global miRNA expression of bone marrow mesenchymal stem/stromal cells derived from Fanconi anemia patients. Hum Cell. 2022;35(1):111–24.
Lecourt S, Vanneaux V, Leblanc T, et al. Bone marrow microenvironment in fanconi anemia: a prospective functional study in a cohort of fanconi anemia patients. Stem Cells Dev. 2010;19(2):203–8.
Amarachintha S, Sertorio M, Wilson A, Li X, Pang Q. Fanconi anemia mesenchymal stromal cells-derived glycerophospholipids skew hematopoietic stem cell differentiation through toll-like receptor signaling. Stem Cells. 2015;33(11):3382–96.
Mantelli M, Avanzini MA, Rosti V, et al. Comprehensive characterization of mesenchymal stromal cells from patients with Fanconianaemia. Br J Haematol. 2015;170(6):826–36.
Wang C, Zhang F, Cao Y, et al. Etoposide induces apoptosis in activated human hepatic stellate cells via ER stress. Sci Rep. 2016;6:34330.
Avril T, Vauleon E, Chevet E. Endoplasmic reticulum stress signaling and chemotherapy resistance in solid cancers. Oncogenesis. 2017;6(8):e373.
Vianello F, Villanova F, Tisato V, et al. Bone marrow mesenchymal stromal cells non-selectively protect chronic myeloid leukemia cells from imatinib-induced apoptosis via the CXCR4/CXCL12 axis. Haematologica. 2010;95(7):1081–9.
Chandran RR, Xie Y, Gallardo-Vara E, et al. Distinct roles of KLF4 in mesenchymal cell subtypes during lung fibrogenesis. Nat Commun. 2021;12(1):7179.
Cho DI, Kang WS, Hong MH, et al. The optimization of cell therapy by combinational application with apicidin-treated mesenchymal stem cells after myocardial infarction. Oncotarget. 2017;8(27):44281–94.
Fattizzo B, Giannotta JA, Barcellini W. Mesenchymal stem cells in aplastic anemia and myelodysplastic syndromes: the “seed and soil” crosstalk. Int J Mol Sci. 2020;21(15):5438.
Agarwal P, Isringhausen S, Li H, et al. Mesenchymal niche-specific expression of Cxcl12 controls quiescence of treatment-resistant leukemia stem cells. Cell Stem Cell. 2019;24(5):769–84.
Jamil S, Lam I, Majd M, Tsai SH, Duronio V. Etoposide induces cell death via mitochondrial-dependent actions of p53. Cancer Cell Int. 2015;15:79.
Kojima K, McQueen T, Chen Y, et al. p53 activation of mesenchymal stromal cells partially abrogates microenvironment-mediated resistance to FLT3 inhibition in AML through HIF-1alpha-mediated down-regulation of CXCL12. Blood. 2011;118(16):4431–9.
Androutsopoulos VP, Tsatsakis AM, Spandidos DA. Cytochrome P450 CYP1A1: wider roles in cancer progression and prevention. BMC Cancer. 2009;9:187.
Singh KP, Bennett JA, Casado FL, Walrath JL, Welle SL, Gasiewicz TA. Loss of aryl hydrocarbon receptor promotes gene changes associated with premature hematopoietic stem cell exhaustion and development of a myeloproliferative disorder in aging mice. Stem Cells Dev. 2014;23(2):95–106.
Schultz KAP, Stewart DR, Kamihara J, et al. DICER1 tumor predisposition. In: Adam MP, et al., editors. Gene reviews (R). WA: Seattle; 1993.
Flynn CM, Kaufman DS. Donor cell leukemia: insight into cancer stem cells and the stem cell niche. Blood. 2007;109(7):2688–92.
Ozdogan H, Gur Dedeoglu B, Oztemur Islakoglu YA, et al. DICER1 gene and miRNA dysregulation in mesenchymal stem cells of patients with myelodysplastic syndrome and acute myeloblastic leukemia. Leuk Res. 2017;63:62–71.
Burger K, Gullerova M. Nuclear re-localization of dicer in primary mouse embryonic fibroblast nuclei following DNA damage. PLoS Genet. 2018;14(2):e1007151.
Wan G, Zhang X, Langley RR, et al. DNA-damage-induced nuclear export of precursor microRNAs is regulated by the ATM-AKT pathway. Cell Rep. 2013;3(6):2100–12.
Acknowledgements
We thank BMT Unit of Childrens Hospital of Hacettepe University for providing bone marrow samples of healthy donors and Fanconi patients.
Funding
This study has been supported by Hacettepe University Scientific Research Projects Coordination Unit with project Number: THD-2019–17607 and partially supported by Turkish Academy of Sciences (TUBA).
Author information
Authors and Affiliations
Contributions
DUÇ, CÖ and BNÖ were involved in conceptualization; CÖ, BNÖ, EAB, GT and BM helped in methodology; CÖ, BNÖ and BM contributed to formal analysis and investigation; CÖ and DUÇ helped in writing—original draft; DUÇ, ŞÜ and BNÖ contributed to review and editing; CÖ, BM and DUÇ were involved in ; DUÇ and CÖ helped in supervision; Ş.Ü provided FA patient samples
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict of interest.
Ethical approval
Signed informed consent for collection, storage and use of cells for research purposes was obtained and the study was approved by the Institutional Review Board of Hacettepe University (Study approval number: GO 21/230 and GO18/916–35).
Informed consent
Informed consent was obtained from all individual participants/their parents included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Full first names have been updated in the author group.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Özdemir, C., Muratoğlu, B., Özel, B.N. et al. Multiparametric analysis of etoposide exposed mesenchymal stem cells and Fanconi anemia cells: implications in development of secondary myeloid malignancy. Clin Exp Med 23, 4511–4524 (2023). https://doi.org/10.1007/s10238-023-01087-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01087-0