Abstract
Background
Endovascular treatment (EVT) is effective for large vessel occlusion (LVO) stroke with smaller volumes of CT perfusion (CTP)-defined core. However, the influence of perfusion imaging during thrombectomy on the functional outcomes of patients with large ischemic core (LIC) stroke at both early and late time windows is uncertain in real-world practice.
Method
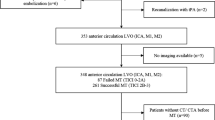
A retrospective analysis was performed on 99 patients who underwent computed tomography angiography (CTA) and CT perfusion (CTP)-Rapid Processing of Perfusion and Diffusion (RAPID) before EVT and had a baseline ischemic core ≥ 50 mL and/or Alberta Stroke Program Early CT Score (ASPECTS) score of 0–5. The primary outcome was the three-month modified Rankin Scale (mRS) score. Data were analyzed by binary logistic regression and receiver operating characteristic (ROC) curves.
Results
A fair outcome (mRS, 0–3) was found in 34 of the 99 patients while 65 had a poor prognosis (mRS, 4–6). The multivariate logistic regression analysis showed that onset-to-reperfusion (OTR) time (odds ratio [OR], 1.004; 95% confidence interval [CI], 1.001–1.007; p = 0.008), ischemic core (OR, 1.066; 95% CI, 1.024–1.111; p = 0.008), and the hypoperfusion intensity ratio (HIR) (OR, 70.898; 95% CI, 1.130-4450.152; p = 0.044) were independent predictors of outcome. The combined results of ischemic core, HIR, and OTR time showed good performance with an area under the ROC curve (AUC) of 0.937, significantly higher than the individual variables (p < 0.05) using DeLong’s test.
Conclusions
Higher HIR and longer OTR time in large core stroke patients were independently associated with unfavorable three-month outcomes after EVT.


Similar content being viewed by others
Data sharing statement
The datasets are available from the corresponding author on reasonable request.
References
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between Deficit and Infarct. N Engl J Med 378:11–21
Albers GW, Marks MP, Kemp S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Huang X, Yang Q, Shi X et al Predictors of malignant brain edema after mechanical thrombectomy for acute ischemic stroke. J Neurointerv Surg 2019:994–998
Yoshimura S, Sakai N, Yamagami H et al (2022) Endovascular therapy for Acute Stroke with a large ischemic region. N Engl J Med 386(14):1303–1313
Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN et al (2023) Trial of endovascular therapy for Acute ischemic stroke with large infarct. N Engl J Med 388(14):1272–1283
Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS et al (2023) Trial of Endovascular Thrombectomy for large ischemic strokes. N Engl J Med 388(14):1259–1271
Yoshimoto T, Inoue M, Tanaka K et al (2021) Identifying large ischemic core volume ranges in acute stroke that can benefit from mechanical thrombectomy. J Neurointerv Surg 13:1081–1087
Campbell BCV, Majoie C, Albers GW et al (2019) Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy: a meta-analysis of individual patient-level data. Lancet Neurol 18:46–55
Yoshimoto T, Inoue M, Yamagami H et al (2019) Use of Diffusion-Weighted Imaging-Alberta Stroke Program Early computed tomography score (DWI-ASPECTS) and ischemic core volume to Determine the Malignant Profile in Acute Stroke. J Am Heart Assoc 8:e012558
Ballout AA (2023 Apr) Endovascular thrombectomy of large ischemic strokes: reimagining the boundaries of reperfusion. Interv Neuroradiol 17:15910199231170283
Olivot JM, Mlynash M, Inoue M et al (2014) Hypoperfusion intensity ratio predicts infarct progression and functional outcome in the DEFUSE 2 Cohort. Stroke 45:1018–1023
Guenego A, Marcellus DG, Martin BW et al (2019) Hypoperfusion intensity ratio is correlated with patient eligibility for Thrombectomy. Stroke 50:917–922
van Horn N, Broocks G, Kabiri R et al (2022) Cerebral hypoperfusion intensity ratio is linked to progressive early edema formation. J Clin Med ;11
Faizy TD, Kabiri R, Christensen S et al (2021) Perfusion imaging-based tissue-level collaterals predict ischemic lesion net water uptake in patients with acute ischemic stroke and large vessel occlusion. J Cereb Blood Flow Metab 41:2067–2075
Saver JL, Goyal M, van der Lugt A et al (2016) Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 316:1279–1288
Tao C, Nogueira RG, Zhu Y et al (2022) Trial of Endovascular Treatment of Acute basilar-artery occlusion. N Engl J Med 387:1361–1372
Lansberg MG, Cereda CW, Mlynash M et al (2015) Response to endovascular reperfusion is not time-dependent in patients with salvageable tissue. Neurology 85:708–714
Powers WJ, Rabinstein AA, Ackerson T et al (2018) 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. ;49:e46-e110
Adams HP Jr., Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Zaidat OO, Yoo AJ, Khatri P et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663
Wityk RJ, Pessin MS, Kaplan RF et al (1994) Serial assessment of acute stroke using the NIH stroke scale. Stroke 25:362–365
Zhang X, Yuan K, Wang H et al (2020) Nomogram to Predict Mortality of Endovascular Thrombectomy for ischemic stroke despite successful recanalization. J Am Heart Association :e014899
Yoo AJ, Simonsen CZ, Prabhakaran S et al (2013) Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke 44:2509–2512
Demeestere J, Christensen S, Mlynash M et al (2021) Effect of sex on clinical outcome and imaging after Endovascular Treatment of large-vessel ischemic stroke. J Stroke Cerebrovasc Dis 30:105468
Tanaka K, Goyal M, Menon BK et al (2022) Significance of baseline ischemic core volume on Stroke Outcome after Endovascular Therapy in patients Age ≥ 75 years: a pooled analysis of individual Patient Data from 7 trials. Stroke 53:3564–3571
Ma G, Yu Z, Jia B et al (2022) Time to endovascular reperfusion and outcome in Acute ischemic stroke: a nationwide prospective Registry in China. Clin Neuroradiol 32:997–1009
Rao VL, Mlynash M, Christensen S et al (2020) Collateral status contributes to differences between observed and predicted 24-h infarct volumes in DEFUSE 3. J Cereb Blood Flow Metab 40:1966–1974
Mohammaden MH, Haussen DC, Pisani L et al (2021) Baseline ASPECTS and hypoperfusion intensity ratio influence the impact of first pass reperfusion on functional outcomes. J Neurointerv Surg 13:124–129
Baek JH, Kim YD, Lee KJ et al (2021) Low hypoperfusion intensity ratio is Associated with a favorable outcome even in large ischemic core and delayed recanalization time. J Clin Med 10(9):1869
Acknowledgements
We thank all the participants in the study.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors have given final approval of the version to be published. Zhengyang Wang: Conceptualization, Methodology, Software, Data curation, Writing - Original Draft. Ling Li: Conceptualization - Review & Editing.
Corresponding author
Ethics declarations
Ethics approval and consent statement
Jiangsu Taizhou People’s Hospital issued approval KY_2022_005_01. Informed consent was waived by the ethics committee due to the retrospective nature.
Conflict of interest
The authors have no conflicts of interest to declare.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Li, L. Long term outcome after endovascular treatment for large ischemic core acute stroke is associated with hypoperfusion intensity ratio and onset-to-reperfusion time. Neurosurg Rev 47, 182 (2024). https://doi.org/10.1007/s10143-024-02417-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02417-w