Abstract
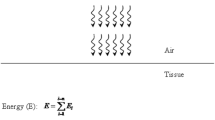
Non-invasive laser irradiation can induce photobiomodulation (PBM) effects in cells and tissues, which can help reduce inflammation and pain in several clinical scenarios. The purpose of this study is to review the current literature to verify whether PBM can produce dose effects in anti-inflammatory experiments by summarizing the clinical and experimental effects of different laser parameters of several diseases. The so-called Arndt-Schulz curve is often used to describe two-phase dose reactions, assuming small doses of therapeutic stimulation, medium doses of inhibition, and large doses of killing. In the past decade, more and more attention has been paid to the clinical application of PBM, especially in the field of anti-inflammation, because it represents a non-invasive strategy with few contraindications. Although there are different types of lasers available, their use is adjusted by different parameters. In general, the parameters involved are wavelength, energy density, power output, and radiation time. However, due to the biphasic effect, the scientific and medical communities remain puzzled by the ways in which the application of PBM must be modified depending on its clinical application. This article will discuss these parameter adjustments and will then also briefly introduce two controversial theories of the molecular and cellular mechanisms of PBM. A better understanding of the extent of dualistic dose response in low-intensity laser therapy is necessary to optimize clinical treatment. It also allows us to explore the most dependable mechanism for PBM use and, ultimately, standardize treatment for patients with various diseases.






Similar content being viewed by others
References
Ferrero-Miliani L et al (2007) Chronic inflammation: importance of NOD2 and NALP3 in interleukin-1beta generation. Clin Exp Immunol 147(2):227–235
Va A, Jnc B, Mkc A (2020) Fight fire with fire: neurobiology of capsaicin-induced analgesia for chronic pain - ScienceDirect. Pharmacol Ther
Scott A et al (2004) What is “inflammation”? Are we ready to move beyond Celsus? Br J Sports Med 38(3):248–249
Granger DN (2010) Inflammation and the microcirculation. Minerva 2(1):1–87
Soter N, Wasserman S (1980) Physical urticaria/angioedema: an experimental model of mast cell activation in humans. J Allergy Clin Immunol 66(5):358–365
Korniluk A et al (2017) From inflammation to cancer. Ir J Med Sci 186(1):57–62
Pelletier JP (2001) Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum 44(6):1237–47
Griffioen AW, Molema G (2000) Angiogenesis: potentials for pharmacologic intervention in the treatment of cancer, cardiovascular diseases, and chronic inflammation. Pharmacol Rev 52(2):237
Almekinders LC, Banes AJ, Ballenger CA (1993) Effects of repetitive motion on human fibroblasts. Med Sci Sports Exerc 25(5):603–607
Li N, Shi RH (2018) Updated review on immune factors in pathogenesis of Crohn’s disease. World J Gastroenterol 24(1):15–22
Maisch B (2019) Cardio-immunology of myocarditis: focus on immune mechanisms and treatment options. Front Cardiovasc Med 6:48
Vane JR, Botting RM (2003) The mechanism of action of aspirin. Thromb Res 110(5–6):255–258
Dmling A, Li X (2021) TNF-alpha: the shape of small molecules to come? Drug Discov Today (12)
Zanotta N et al (2020) Photobiomodulation modulates inflammation and oral microbiome: a pilot study. Biomarkers 25(8):677–684
Catao MH et al (2016) Green LED light has anti-inflammatory effects on burns in rats. Burns 42(2):392–396
Sun Q et al (2020) Role of E2F1/SPHK1 and HSP27 during irradiation in a PMA-induced inflammatory model. Photobiomodul Photomed Laser Surg 38(8):512–520
Hanna R et al (2020) Phototherapy as a rational antioxidant treatment modality in COVID-19 management; new concept and strategic approach: critical review. Antioxidants (Basel) 9(9):875
Arany PR (2016) Craniofacial wound healing with photobiomodulation therapy: new insights and current challenges. J Dent Res 95(9):977–984
Carroll JD et al (2014) Developments in low level light therapy (LLLT) for dentistry. Dent Mater 30(5):465–475
Assis L et al (2012) Low-level laser therapy (808 nm) reduces inflammatory response and oxidative stress in rat tibialis anterior muscle after cryolesion. Lasers Surg Med 44(9):726–735
Yang M et al (2021) Current application and future directions of photobiomodulation in central nervous diseases. Neural Regen Res 16(6):1177–1185
Muniz XC et al (2021) Efficacy of low-level laser therapy in nerve injury repair-a new era in therapeutic agents and regenerative treatments. Neurol Sci 42(10):4029–4043
Sert G et al (2021) Photobiomodulation with polychromatic light (600–1200 nm) improves fat graft survival by increasing adipocyte viability, neovascularization, and reducing inflammation in a rat model. Lasers Surg Med 54(2):268–280
Rochkind S, Almog M (2021) Protective effect of photobiomodulation on denervated and crushed muscle. Photobiomodul Photomed Laser Surg 39(7):435–436
Hamblin MR, Nelson ST, Strahan JR (2018) Photobiomodulation and cancer: what is the truth? Photomed Laser Surg 36(5):241–245
Kim Y-D et al (2007) Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: an experimental study in rats. Lasers Surg Med 39(5):441–450
Aliodoust M et al (2014) Evaluating the effect of low-level laser therapy on healing of tentomized Achilles tendon in streptozotocin-induced diabetic rats by light microscopical and gene expression examinations. Lasers Med Sci 29(4):1495–1503
Ramos L et al (2018) Characterization of skeletal muscle strain lesion induced by stretching in rats: effects of laser photobiomodulation. Photomed Laser Surg 36(9):460–467
Zecha JA et al (2016) Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 1: mechanisms of action, dosimetric, and safety considerations. Support Care Cancer 24(6):2781–2792
Tang E, Arany P (2013) Photobiomodulation and implants: implications for dentistry. J Periodontal Implant Sci 43(6):262–268
Arora V, Campbell JN, Chung MK (2021) Fight fire with fire: neurobiology of capsaicin-induced analgesia for chronic pain. Pharmacol Ther 220:107743
Tuner J, Hosseinpour S, Fekrazad R (2019) Photobiomodulation in temporomandibular disorders. Photobiomodul Photomed Laser Surg 37(12):826–836
Abreu Villela P et al (2017) Antimicrobial photodynamic therapy (aPDT) and photobiomodulation (PBM - 660 nm) in a dog with chronic gingivostomatitis. Photodiagnosis Photodyn Ther 20:273–275
Gupta A et al (2015) Superpulsed (Ga-As, 904 nm) low-level laser therapy (LLLT) attenuates inflammatory response and enhances healing of burn wounds. J Biophotonics 8(6):489–501
Chu YH et al (2018) Low-level laser therapy prevents endothelial cells from TNF-alpha/cycloheximide-induced apoptosis. Lasers Med Sci 33(2):279–286
Ustaoglu G, Ercan E, Tunali M (2017) Low-level laser therapy in enhancing wound healing and preserving tissue thickness at free gingival graft donor sites: a randomized, controlled clinical study. Photomed Laser Surg 35(4):223–230
Rosso MPO et al (2019) Photobiomodulation therapy (PBMT) applied in bone reconstructive surgery using bovine bone grafts: a systematic review. Materials (Basel) 12(24):4051
Albarracin R, Eells J, Valter K (2011) Photobiomodulation protects the retina from light-induced photoreceptor degeneration. Invest Ophthalmol Vis Sci 52(6):3582–3592
Wooff Y et al (2020) Small-medium extracellular vesicles and their miRNA cargo in retinal health and degeneration: mediators of homeostasis, and vehicles for targeted gene therapy. Front Cell Neurosci 14:160
Fu JC-M et al (2022) The adjuvant therapy of intravenous laser irradiation of blood (ILIB) on pain and sleep disturbance of musculoskeletal disorders. J Personal Med 12(8):1333
Lan C-H et al (2022) Effects of intravascular photobiomodulation on motor deficits and brain perfusion images in intractable myasthenia gravis: a case report. World J Clin Cases 10(24):8718–8727
Chang Y-L, Chang S-T (2022) The effects of intravascular photobiomodulation on sleep disturbance caused by Guillain-Barré syndrome after Astrazeneca vaccine inoculation: Case report and literature review. Medicine 101(6):e28758
Liu C-C et al (2021) Effects of intravascular laser phototherapy on delayed neurological sequelae after carbon monoxide intoxication as evaluated by brain perfusion imaging: a case report and review of the literature. World J Clin Cases 9(13):3048–3055
Yang W-H, Lin S-P, Chang S-T (2017) Case report: rapid improvement of crossed cerebellar diaschisis after intravascular laser irradiation of blood in a case of stroke. Medicine 96(2):e5646
Huan Y-Y et al. (2009) Biphasic dose response in low level light therapy. Dose-Response 7(4)
Chow RT, Armati PJ (2016) Photobiomodulation: implications for anesthesia and pain relief. Photomed Laser Surg 34(12):599–609
Grandinetti V et al (2019) Photobiomodulation therapy combined with carvedilol attenuates post-infarction heart failure by suppressing excessive inflammation and oxidative stress in rats. Sci Rep 9(1):9425
Ferraresi C, Huang YY, Hamblin MR (2016) Photobiomodulation in human muscle tissue: an advantage in sports performance? J Biophotonics 9(11–12):1273–1299
Huang Y-Y et al. (2011) Biphasic dose response in low level light therapy – an update. Dose-Response 9(4)
Pastore D et al (1994) Increase in ←H+/e- ratio of the cytochrome c oxidase reaction in mitochondria irradiated with helium-neon laser. Biochem Mol Biol Int 34(4):817–826
Pelletier JP (2001) Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum 44(6):1237–1247
Heiskanen V, Hamblin MR (2018) Photobiomodulation: lasersvs.light emitting diodes? Photochem Photobiol Sci 17(8):1003–1017
Gholami L et al (2019) Photobiomodulation in periodontology and implant dentistry: part 1. Photobiomodul Photomed Laser Surg 37(12):739–765
Berman MH, Nichols TW (2019) Treatment of neurodegeneration: integrating photobiomodulation and neurofeedback in Alzheimer’s dementia and Parkinson’s: a review. Photobiomodul Photomed Laser Surg 37(10):623–634
Tatmatsu-Rocha JC et al (2018) Mitochondrial dynamics (fission and fusion) and collagen production in a rat model of diabetic wound healing treated by photobiomodulation: comparison of 904 nm laser and 850 nm light-emitting diode (LED). J Photochem Photobiol B 187:41–47
Langella LG et al (2018) Photobiomodulation therapy (PBMT) on acute pain and inflammation in patients who underwent total hip arthroplasty—a randomized, triple-blind, placebo-controlled clinical trial. Lasers Med Sci 33(9):1933–1940
Falcone D et al (2018) Effects of blue light on inflammation and skin barrier recovery following acute perturbation. Pilot study results in healthy human subjects. Photodermatol, Photoimmunol Photomed 34(3):184–193
Li Y et al (2020) Low-level laser therapy induces human umbilical vascular endothelial cell proliferation, migration and tube formation through activating the PI3K/Akt signaling pathway. Microvasc Res 129:103959
Pereira FC et al (2017) Antinociceptive effects of low-level laser therapy at 3 and 8 j/cm2in a rat model of postoperative pain: possible role of endogenous opioids. Lasers Surg Med 49(9):844–851
Harorli OT, Hatipoglu M, Erin N (2019) Effect of photobiomodulation on secretion of IL-6 and IL-8 by human gingival fibroblasts in vitro. Photobiomodul, Photomed Laser Surg 37(8):457–464
Rupel K et al (2018) Photobiomodulation at multiple wavelengths differentially modulates oxidative stress in vitro and in vivo. Oxid Med Cell Longev 2018:1–11
Xu YY, Liu CY, Cheng L (2012) Photobiomodulation process. Int J Photoenergy 2012. https://doi.org/10.1155/2012/374861
Liu CY et al (2012) Photobiomodulation on stress. Int J Photoenergy 2012 (2012-08-9), 2012:10178–10182
Wang ZX, Kim SH (2020) Effect of photobiomodulation therapy (660 nm) on wound healing of rat skin infected by Staphylococcus. Photobiomodul Photomed Laser Surg 38(7):419–424
Chow RT, Heller GZ, Barnsley L (2006) The effect of 300 mW, 830 nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain 124(1–2):201–210
Hawkins D, Abrahamse H (2006) Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg 24(6):705
Brindley GS (1952) The Bunsen-Roscoe law for the human eye at very short durations. J Physiol 118(1):135–139
Lubart R et al (2006) Photochemistry and photobiology of light absorption by living cells. Photomed Laser Surg 24(2):179–185
Dolgova D et al (2019) Anti-inflammatory and cell proliferative effect of the 1270 nm laser irradiation on the BALB/c nude mouse model involves activation of the cell antioxidant system. Biomed Opt Express 10(8):4261–4275
Tomazoni SS et al (2017) Effects of photobiomodulation therapy and topical non-steroidal anti-inflammatory drug on skeletal muscle injury induced by contusion in rats—part 2: biochemical aspects. Lasers Med Sci 32(8):1879–1887
Neves LMS et al (2018) Photobiomodulation therapy improves acute inflammatory response in mice: the role of cannabinoid receptors/ATP-sensitive K(+) channel/p38-MAPK signalling pathway. Mol Neurobiol 55(7):5580–5593
Lee HS et al (2020) Transoral low-level laser therapy via a cylindrical device to treat oral ulcers in a rodent model. Lasers Surg Med 52(7):647–652
Pigatto GR, Silva CS, Parizotto NA (2019) Photobiomodulation therapy reduces acute pain and inflammation in mice. J Photochem Photobiol B 196:111513
Li W-H et al (2018) Low-level red LED light inhibits hyperkeratinization and inflammation induced by unsaturated fatty acid in anin vitromodel mimicking acne. Lasers Surg Med 50(2):158–165
Ebrahiminaseri A et al (2021) Combination treatment of dendrosomal nanocurcumin and low-level laser therapy develops proliferation and migration of mouse embryonic fibroblasts and alter TGF-beta, VEGF, TNF-alpha and IL-6 expressions involved in wound healing process. PLoS One 16(5):e0247098
Li K et al (2020) Attenuation of the inflammatory response and polarization of macrophages by photobiomodulation. Lasers Med Sci 35(7):1509–1518
Prabhu V et al (2012) Spectroscopic and histological evaluation of wound healing progression following low level laser therapy (LLLT). J Biophotonics 5(2):168–184
Petrellis MC et al (2017) Laser photobiomodulation of pro-inflammatory mediators on Walker tumor 256 induced rats. J Photochem Photobiol, B 177:69–75
Lamaro-Cardoso A et al (2019) Photobiomodulation associated to cellular therapy improve wound healing of experimental full thickness burn wounds in rats. J Photochem Photobiol, B 194:174–182
Liang Z, et al (2020) Photobiomodulation by diffusing optical fiber on spinal cord: a feasibility study in piglet model. J Biophotonics 13(4):e201960022
Alves A et al (2013) Effect of low-level laser therapy on the expression of inflammatory mediators and on neutrophils and macrophages in acute joint inflammation. Arthritis Res Ther 15(5):R116
Sutherland JC (2002) Biological effects of polychromatic light. Photochem Photobiol 76(2):164–170
Karu T (1989) Laser biostimulation: a photobiological phenomenon. J Photochem Photobiol, B 3(4):638–638
Karu TI, Kolyakov SF (2005) Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg 23(4):355–361
Micheli L et al (2017) Photobiomodulation therapy by NIR laser in persistent pain: an analytical study in the rat. Lasers Med Sci 32(8):1835–1846
Yang L et al (2018) Photobiomodulation therapy promotes neurogenesis by improving post-stroke local microenvironment and stimulating neuroprogenitor cells. Exp Neurol 299(Pt A):86–96
Li Y, et al. (2020) The inflammation and reactive oxygen species regulated by Nrf2 and NF-kappaB signaling pathways in 630-nm light-emitting diode irradiation treated THP-1 monocytes/macrophages. Lasers Med Sci
Li H et al (2020) Photobiomodulation (450 nm) alters the infection of periodontitis bacteria via the ROS/MAPK/mTOR signaling pathway. Free Radic Biol Med 152:838–853
de Brito Sousa K et al (2020) Differential expression of inflammatory and anti-inflammatory mediators by M1 and M2 macrophages after photobiomodulation with red or infrared lasers. Lasers Med Sci 35(2):337–343
Caruso-Davis MK et al (2011) Efficacy of low-level laser therapy for body contouring and spot fat reduction. Obes Surg 21(6):722–729
Thunshelle C, Hamblin MR (2016) Transcranial low-level laser (light) therapy for brain injury. Photomed Laser Surg 34(12):587–598
Yang B et al (2020) Photobiomodulation therapy for repeated closed head injury in rats. J Biophotonics 13(2):e201960117
Yamada EF et al (2020) Photobiomodulation therapy in knee osteoarthritis reduces oxidative stress and inflammatory cytokines in rats. J Biophotonics 13(1):e201900204
Wan Z et al (2020) NIR light-assisted phototherapies for bone-related diseases and bone tissue regeneration: a systematic review. Theranostics 10(25):11837–11861
Tsai S-R et al (2015) Low-level light therapy potentiates NPe6-mediated photodynamic therapy in a human osteosarcoma cell line via increased ATP. Photodiagn Photodyn Ther 12(1):123–130
McColloch A. et al. (2020) Alterted adipogenesis of human mesenchymal stem cells by photobiomodulation using 1064 nm laser light. Lasers Surg Med
Ferroni L et al (2020) Fluorescent light energy (FLE) acts on mitochondrial physiology improving wound healing. J Clin Med 9(2):559
Zamani A et al (2020) Modulatory effect of photobiomodulation on stem cell epigenetic memory: a highlight on differentiation capacity. Lasers Med Sci 35(2):299–306
Funding
This work was supported by the National Natural Science Foundation of China (grant no. 81901241) and Beijing Tongzhou District Science and Technology Development Plan (grant no. KJ2021CX008-24).
Author information
Authors and Affiliations
Contributions
Idea: Fang Nie, YuChuan Ding, Wei Han, and Yan Zhang. Literature search: Fang Nie, Melissa Will, and Hao Sun. Data analysis: Fang Nie, Yu Ji, Zeqian Lee, Yan Zhang, and Yu Ji. Writing—original draft preparation: Fang Nie, Melissa Will, Yu Ji, Wei Han, YuChuan Ding, and Hao Sun. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, F., Hao, S., Ji, Y. et al. Biphasic dose response in the anti-inflammation experiment of PBM. Lasers Med Sci 38, 66 (2023). https://doi.org/10.1007/s10103-022-03664-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-022-03664-3