Abstract
Background
Aspiration is a common complication of poststroke dysphagia (PSD) and is associated with poor prognosis and mortality. There is no uniform criterion for determining aspiration associated with dysphagia. The aim of this study was to identify early predictors of aspiration, leading to the development of a simple nomogram for identifying aspiration risk associated with dysphagia in hospitalized patients after stroke.
Methods
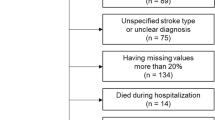
Demographic information and clinical characteristics of 330 patients with PSD in the training cohort were utilized to develop a nomogram. The LASSO regression method was used to screen variables, and logistic regression was used to construct the nomogram. Internal validation was performed with bootstrap in the training cohort, and external validation was performed in the validation cohort of another 82 patients. The area under the curve (AUC), calibration curves, and decision curve analysis (DCA) were used to evaluate the performance of the nomogram.
Results
Seven variables were selected based on LASSO and multivariate logistic regression. The AUC of the nomogram was 0.834 (95% CI, 0.790–0.878) in the training cohort, 0.806 (95% CI, 0.791–0.880) in the internal validation cohort, and 0.882 (95% CI, 0.810–0.954) in the external validation cohort, which indicated that the model had good discrimination. The calibration and DCA curves showed that the nomogram had good accuracy and clinical utility.
Conclusions
In this study, we established a nomogram that can be used to identify the risk of aspiration associated with dysphagia after stroke, and patients may benefit from early screening and preventive care.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
GBD 2019 Stroke Collaborators (2021) Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20:795–820. https://doi.org/10.1016/s1474-4422(21)00252-0
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R (2005) Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36:2756–2763. https://doi.org/10.1161/01.STR.0000190056.76543.eb
Ebihara S, Sekiya H, Miyagi M, Ebihara T, Okazaki T (2016) Dysphagia, dystussia, and aspiration pneumonia in elderly people. J Thorac Dis 8:632–639. https://doi.org/10.21037/jtd.2016.02.60
Lesa L, Brunelli L, Valent F et al (2021) The underestimated burden of aspiration event and pneumonia within hospitals: what happens after dysphagia. Ann Ig 33:555–563. https://doi.org/10.7416/ai.2021.2436
Bath PM, Lee HS, Everton LF (2018) Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev 10:CD000323. https://doi.org/10.1002/14651858.CD000323.pub3
Benjamin E, Haltmeier T, Chouliaras K, Siboni S, Durso J, Inaba K, Demetriades D (2015) Witnessed aspiration in trauma: frequent occurrence, rare morbidity--a prospective analysis. J Trauma Acute Care Surg 79:1030–1036; discussion 1036-1037. https://doi.org/10.1097/ta.0000000000000704
Brodsky MB, Suiter DM, González-Fernández M, Michtalik HJ, Frymark TB, Venediktov R, Schooling T (2016) Screening accuracy for aspiration using bedside water swallow tests: a systematic review and meta-analysis. Chest 150:148–163. https://doi.org/10.1016/j.chest.2016.03.059
Feng MC, Lin YC, Chang YH, Chen CH, Chiang HC, Huang LC, Yang YH, Hung CH (2019) The mortality and the risk of aspiration pneumonia related with dysphagia in stroke patients. J Stroke Cerebrovasc Dis 28:1381–1387. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.02.011
Dziewas R, Allescher HD, Aroyo I et al (2021) Diagnosis and treatment of neurogenic dysphagia - S1 guideline of the German Society of Neurology. Neurol Res Pract 3:23. https://doi.org/10.1186/s42466-021-00122-3
National Institute for Health and Care Excellence (NICE) (2019) Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. National Institute for Health and Care Excellence (NICE), London. https://www.nice.org.uk/guidance/ng128. Accessed 13 Apr 2022
Kiekens C, Tognonato C (2022) Which screening tool should be used for identifying aspiration risk associated with dysphagia in acute stroke? A Cochrane review summary with commentary. NeuroRehabilitation 51:533–535. https://doi.org/10.3233/nre-228024
Wirth R, Smoliner C, Jäger M, Warnecke T, Leischker AH, Dziewas R (2013) Guideline clinical nutrition in patients with stroke. Exp Transl Stroke Med 5:14. https://doi.org/10.1186/2040-7378-5-14
Dziewas R, Michou E, Trapl-Grundschober M et al (2021) European Stroke Organisation and European Society for Swallowing Disorders guideline for the diagnosis and treatment of post-stroke dysphagia. Eur Stroke J 6:Lxxxix-cxv. https://doi.org/10.1177/23969873211039721
Son YG, Shin J, Ryu HG (2017) Pneumonitis and pneumonia after aspiration. J Dent Anesth Pain Med 17:1–12. https://doi.org/10.17245/jdapm.2017.17.1.1
Kollmeier BR, Keenaghan M, Doerr C (2023) Aspiration risk (nursing). StatPearls Publishing, Treasure Island, FL
Boaden E, Burnell J, Hives L, Dey P, Clegg A, Lyons MW, Lightbody CE, Hurley MA, Roddam H, McInnes E, Alexandrov A, Watkins CL (2021) Screening for aspiration risk associated with dysphagia in acute stroke. Cochrane Database Syst Rev 10:CD012679. https://doi.org/10.1002/14651858.CD012679.pub2
Smithard DG, Smeeton NC, Wolfe CD (2007) Long-term outcome after stroke: does dysphagia matter? Age Ageing 36:90–94. https://doi.org/10.1093/ageing/afl149
Giraldo-Cadavid LF, Pantoja JA, Forero YJ, Gutiérrez HM, Bastidas AR (2020) Aspiration in the fiberoptic endoscopic evaluation of swallowing associated with an increased risk of mortality in a cohort of patients suspected of oropharyngeal dysphagia. Dysphagia 35:369–377. https://doi.org/10.1007/s00455-019-10036-7
Helldén J, Bergström L, Karlsson S (2018) Experiences of living with persisting post-stroke dysphagia and of dysphagia management - a qualitative study. Int J Qual Stud Health Well-being 13:1522194. https://doi.org/10.1080/17482631.2018.1522194
Daniels SK, Pathak S, Rosenbek JC, Morgan RO, Anderson JA (2016) Rapid aspiration screening for suspected stroke: part 1: development and validation. Arch Phys Med Rehabil 97:1440–1448. https://doi.org/10.1016/j.apmr.2016.03.025
McCullough GH, Rosenbek JC, Wertz RT, McCoy S, Mann G, McCullough K (2005) Utility of clinical swallowing examination measures for detecting aspiration post-stroke. J Speech Lang Hear Res 48:1280–1293. https://doi.org/10.1044/1092-4388(2005/089)
Mazumder R, Friedman JH, Hastie T (2011) SparseNet: coordinate descent with nonconvex penalties. J Am Stat Assoc 106:1125–1138. https://doi.org/10.1198/jasa.2011.tm09738
Taylor JK, Fleming GB, Singanayagam A, Hill AT, Chalmers JD (2013) Risk factors for aspiration in community-acquired pneumonia: analysis of a hospitalized UK cohort. Am J Med 126:995–1001. https://doi.org/10.1016/j.amjmed.2013.07.012
Smith CH, Logemann JA, Colangelo LA, Rademaker AW, Pauloski BR (1999) Incidence and patient characteristics associated with silent aspiration in the acute care setting. Dysphagia 14:1–7. https://doi.org/10.1007/pl00009579
Winstein CJ, Stein J, Arena R et al (2016) Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47:e98–e169. https://doi.org/10.1161/str.0000000000000098
Prust ML, Nutakki A, Habanyama G, Chishimba L, Chomba M, Mataa M, Yumbe K, Zimba S, Gottesman RF, Bahouth MN, Saylor DR (2021) Aspiration pneumonia in adults hospitalized with stroke at a large academic hospital in Zambia. Neurol Clin Pract 11:e840–e847. https://doi.org/10.1212/cpj.0000000000001111
Min SW, Oh SH, Kim GC, Sim YJ, Kim DK, Jeong HJ (2018) Clinical importance of peak cough flow in dysphagia evaluation of patients diagnosed with ischemic stroke. Ann Rehabil Med 42:798–803. https://doi.org/10.5535/arm.2018.42.6.798
Schimmel M, Ono T, Lam OL, Müller F (2017) Oro-facial impairment in stroke patients. J Oral Rehabil 44:313–326. https://doi.org/10.1111/joor.12486
Acknowledgements
The authors would like to thank the study participants and clinical staff for their support and contributions to this study.
Funding
This work was supported by funding from the National Natural Science Foundation of China (Program No. 72364005).
Author information
Authors and Affiliations
Contributions
Lihua Chen and Juan Li carried out the conception and design of the research.
Lihua Chen and Fang Tian participated in the acquisition of data.
Huan Tang and Juan Xue participated in data curation.
Zuoxiu Chen, Mingqing Hao, and Chao Xue performed the statistical analysis.
Juan Li participated in obtaining funding.
Lihua Chen and Juan Li drafted the manuscript and participated in revision of the manuscript for important intellectual content.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study received ethical approval from the Guizhou Provincial People’s Hospital Ethics Committee under the reference number “Ethical Approval Word (Research) [2022] No. 130.”
Informed consent
All patients or their consultees signed a written informed consent for participation and publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Li, J., Tian, F. et al. A simple nomogram for predicting aspiration associated with dysphagia in hospitalized patients after stroke. Neurol Sci 45, 2729–2736 (2024). https://doi.org/10.1007/s10072-024-07312-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-024-07312-2