Abstract
Objective
This is a retrospective analysis of clinical data from individuals diagnosed with neurosyphilis, aiming to enhance healthcare professionals’ understanding of the disease and expedite early diagnosis and intervention.
Methods
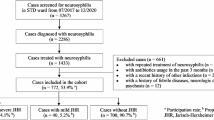
A retrospective analysis was conducted on the clinical records of 50 patients who received a diagnosis of symptomatic neurosyphilis and were admitted to the Neurology Department during the period spanning January 2012 to December 2022.
Results
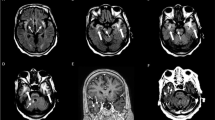
Clinical manifestations encompassed diverse phenotypes, with syphilitic meningitis accounting for 16% of cases, characterized by symptoms such as headache, blepharoptosis, paralysis, blurred vision, and tinnitus. Meningovascular syphilis presented in 36% of cases, exhibiting episodic loss of consciousness, limb numbness, and limb convulsion. Paralytic dementia manifested in 36% of cases, featuring symptoms such as memory loss, sluggish response, and slow movement. Tabes dorsalis was observed in 12% of cases, presenting with weakness, numbness, and staggering. Routine cerebrospinal fluid (CSF) analysis indicated abnormal white blood cell counts in 60% of patients, while biochemical testing revealed abnormal protein content in 52% of patients. Notably, statistically significant differences were observed between patients with interstitial and parenchymatous neurosyphilis (Z = 2.023, P = 0.044) in terms of CSF protein content. Electroencephalogram (EEG) results were abnormal in six patients, and imaging studies unveiled diverse findings in 46 patients.
Conclusion
The study highlights the importance of neurological and/or ocular symptoms in diagnosing symptomatic neurosyphilis. Individuals with hypomnesia should be closely monitored for potential neurosyphilis. Integrating clinical manifestations, laboratory tests, EEG, and imaging can reduce misdiagnosis. This comprehensive approach shows promise in improving early identification and management of neurosyphilis.



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
World Health Organization (2018) Report on global sexually transmitted infection surveillance
Tang W, Huang S, Chen L et al (2017) Late neurosyphilis and tertiary syphilis in Guangdong Province, China: results from a cross-sectional study. Sci Rep 7:45339. https://doi.org/10.1038/srep45339. (Published 2017 Mar 24)
Yue XL, Gong XD, Li J et al (2021) Epidemiological trends and features of syphilis in China, 2014–2019. Chin J Dermatol 54(8):5. https://doi.org/10.35541/cjd.20210098
Du FZ, Zhang HN, Li JJ et al (2022) Neurosyphilis in China: a systematic review of cases from 2009–2021. Front Med (Lausanne) 9:894841. https://doi.org/10.3389/fmed.2022.894841. (Published 2022 May)
Workowski KA, Bachmann LH, Chan PA et al (2021) Sexually transmitted infections treatment guidelines [J]. MMWR Recomm Rep 70(4):1–187
Nagappa M, Sinha S, Taly AB et al (2013) Neurosyphilis: MRI features and their phenotypic correlation in a cohort of 35 patients from a tertiary care university hospital. Neuroradiology 55(4):379–388. https://doi.org/10.1007/s00234-012-1017-9
Chen Y, Gu HY, Zhang L et al (2015) The analysis of the clinical and epidemiological features of 117 cases of neurosyphilis. Chin J AIDS STD 21(10):879–883. https://doi.org/10.13419/j.cnki.aids.2015.10.15
Li SL, Lin ZF, Zhang HS et al (2012) Relationship between syphilis serofast reaction and neurosyphilis. Chin J Hosp Infect 22(10):2235–2238
Drago F, Merlo G, Ciccarese G et al (2016) Changes in neurosyphilis presentation: a survey on 286 patients. J Eur Acad Dermatol Venereol 30(11):1886–1900. https://doi.org/10.1111/jdv.13753
Dombrowski JC, Pedersen R, Marra CM, Kerani RP, Golden MR (2015) Prevalence estimates of complicated syphilis. Sex Transm Dis 42(12):702–704. https://doi.org/10.1097/OLQ.0000000000000368
Landry T, Smyczek P, Cooper R et al (2019) Retrospective review of tertiary and neurosyphilis cases in Alberta, 1973–2017. BMJ Open 9(6):e025995. https://doi.org/10.1136/bmjopen-2018-025995. (Published 2019 Jun 22)
Bazewicz M, Lhoir S, Makhoul D et al (2021) Neurosyphilis cerebrospinal fluid findings in patients with ocular syphilis. Ocul Immunol Inflamm 29(1):95–101. https://doi.org/10.1080/09273948.2019.1672193
Klein M, Angstwurm K, Esser S et al (2020) German guidelines on the diagnosis and treatment of neurosyphilis. Neurol Res Pract 2:33. https://doi.org/10.1186/s42466-020-00081-1. (Published 2020 Nov 17)
Zhu L, Gu X, Peng RR et al (2014) Comparison of the cerebrospinal fluid (CSF) toluidine red unheated serum test and the CSF rapid plasma reagin test with the CSF venereal disease research laboratory test for diagnosis of neurosyphilis among HIV-negative syphilis patients in China. J Clin Microbiol 52(3):736–740. https://doi.org/10.1128/JCM.02522-13
Castro R, Prieto ES, da Luz Martins Pereira F (2008) Nontreponemal tests in the diagnosis of neurosyphilis: an evaluation of the Venereal Disease Research Laboratory (VDRL) and the Rapid Plasma Reagin (RPR) tests. J Clin Lab Anal 22(4):257–261. https://doi.org/10.1002/jcla.20254
Zhou J, Zhang H, Tang K, Liu R, Li J (2022) An updated review of recent advances in neurosyphilis. Front Med (Lausanne) 9:800383. https://doi.org/10.3389/fmed.2022.800383. (Published 2022 Sep 20)
Vanhaecke C, Grange P, Benhaddou N et al (2016) Clinical and biological characteristics of 40 patients with neurosyphilis and evaluation of Treponema pallidum nested polymerase chain reaction in cerebrospinal fluid samples. Clin Infect Dis 63(9):1180–1186. https://doi.org/10.1093/cid/ciw499
Lu Y, Ke W, Yang L et al (2019) Clinical prediction and diagnosis of neurosyphilis in HIV-negative patients: a case-control study. BMC Infect Dis 19(1):1017. https://doi.org/10.1186/s12879-019-4582-2. (Published 2019 Dec)
Davis AP, Maxwell CL, Mendoza H et al (2021) Cognitive impairment in syphilis: does treatment based on cerebrospinal fluid analysis improve outcome? PLoS One. 16(7):e0254518. https://doi.org/10.1371/journal.pone.0254518. (Published 2021 Jul 13
Ghanem KG (2010) REVIEW: Neurosyphilis: a historical perspective and review. CNS Neurosci Ther 16(5):e157–e168. https://doi.org/10.1111/j.1755-5949.2010.00183.x
Zheng LL, Chen JZ, Zhuang XR, Miao JY (2022) Comparison of electroencephalography in patients with seizures caused by neurosyphilis and viral encephalitis. Front Neurol. 13:879643. https://doi.org/10.3389/fneur.2022.879643. (Published 2022 May 27)
Chow F (2021) Neurosyphilis. Continuum (Minneap Minn) 27(4):1018–1039. https://doi.org/10.1212/CON.0000000000000982
Miklossy J (2015) Historic evidence to support a causal relationship between spirochetal infections and Alzheimer’s disease. Front Aging Neurosci 7:46. https://doi.org/10.3389/fnagi.2015.00046. (Published 2015 Apr 16)
Wang J, Guo Q, Zhou P, Zhang J, Zhao Q, Hong Z (2011) Cognitive impairment in mild general paresis of the insane: AD-like pattern. Dement Geriatr Cogn Disord 31(4):284–290. https://doi.org/10.1159/000326908
Hampel H, Kötter HU, Padberg F, Körschenhausen DA, Möller HJ (1999) Oligoclonal bands and blood–cerebrospinal-fluid barrier dysfunction in a subset of patients with Alzheimer disease: comparison with vascular dementia, major depression, and multiple sclerosis. Alzheimer Dis Assoc Disord 13(1):9–19. https://doi.org/10.1097/00002093-199903000-00002
Milano C, Hoxhaj D, Del Chicca M et al (2023) Alzheimer’s disease and neurosyphilis: meaningful commonalities and differences of clinical phenotype and pathophysiological biomarkers. J Alzheimers Dis 94(2):611–625. https://doi.org/10.3233/JAD-230170
Ewers M, Sperling RA, Klunk WE, Weiner MW, Hampel H (2011) Neuroimaging markers for the prediction and early diagnosis of Alzheimer’s disease dementia. Trends Neurosci 34(8):430–442. https://doi.org/10.1016/j.tins.2011.05.005
Qu C, Liu L, Xu QQ, Xian YF, Lin ZX (2021) Neuroprotective effects of San-Jia-Fu-Mai decoction: studies on the in vitro and in vivo models of Parkinson’s disease. World J Tradit Chin Med 7:192–200
Ewers M, Frisoni GB, Teipel SJ et al (2011) Staging Alzheimer’s disease progression with multimodality neuroimaging. Prog Neurobiol 95(4):535–546. https://doi.org/10.1016/j.pneurobio.2011.06.004
Hampel H, Shaw LM, Aisen P et al (2022) State-of-the-art of lumbar puncture and its place in the journey of patients with Alzheimer’s disease. Alzheimers Dement 18(1):159–177. https://doi.org/10.1002/alz.12372
Acknowledgements
We are particularly grateful to all the people who have given us help on our article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Beijing Tiantan Hospital, Capital Medical University (No.KY2023). Written informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, YS., Li, Q., Zhou, H. et al. Enhancing clinical awareness: retrospective analysis of neurosyphilis cases and diagnostic predictors for early recognition and treatment. Neurol Sci 45, 2825–2833 (2024). https://doi.org/10.1007/s10072-023-07285-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07285-8