Abstract
Background
The brain functional network plays a crucial role in cognitive impairment in temporal lobe epilepsy (TLE). Based on voxel-mirrored homotopic connectivity (VMHC), this study explored how directed functional connectivity changes and is associated with impaired cognition in right TLE (rTLE).
Methods
Twenty-seven patients with rTLE and twenty-seven healthy controls were included to perform VMHC and Granger causality analysis (GCA). Correlation analysis was performed based on GCA and cognitive function.
Results
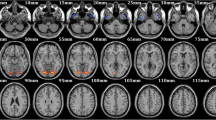
Bilateral middle frontal gyrus (MFG), middle temporal gyrus, dorsolateral superior frontal gyrus (SFGdor), and supramarginal gyrus (SMG) exhibited decreased VMHC values in the rTLE group. Brain regions with altered VMHC had abnormal directed functional connectivity with multiple brain regions, mainly belonging to the default mode network, sensorimotor network, and visual network. Besides, the Montreal Cognitive Assessment (MoCA) score was positively correlated with the connectivity from the left SFGdor to the right cerebellum crus2 and was negatively correlated with the connectivity from the left SMG to the right supplementary motor area (SMA) before correction. Before correction, both phasic and intrinsic alertness reaction time were positively correlated with the connectivity from the left MFG to the left precentral gyrus (PreCG), connectivity from the left SMG to the right PreCG, and the connectivity from the left SMG to the right SMA. The executive control effect reaction time was positively correlated with the connectivity from the left MFG to the left calcarine fissure surrounding cortex before correction.
Conclusion
The disordered functional network tended to be correlated with cognition impairment in rTLE.



Similar content being viewed by others
Data availability
Data is available upon request.
References
Dumlu SN, Ademoglu A, Sun W (2020) Investigation of functional variability and connectivity in temporal lobe epilepsy: a resting state fMRI study. Neurosci Lett 733:135076. https://doi.org/10.1016/j.neulet.2020.135076
Cataldi M, Avoli M, de Villers-Sidani E (2013) Resting state networks in temporal lobe epilepsy. Epilepsia 54:2048–2059. https://doi.org/10.1111/epi.12400
Gao Y, Xiong Z, Wang X et al (2022) Abnormal degree centrality as a potential imaging biomarker for right temporal lobe epilepsy: a resting-state functional magnetic resonance imaging study and support vector machine analysis. Neuroscience 487:198–206. https://doi.org/10.1016/j.neuroscience.2022.02.004
Besson P, Dinkelacker V, Valabregue R et al (2014) Structural connectivity differences in left and right temporal lobe epilepsy. Neuroimage 100:135–144. https://doi.org/10.1016/j.neuroimage.2014.04.071
Lemkaddem A, Daducci A, Kunz N et al (2014) Connectivity and tissue microstructural alterations in right and left temporal lobe epilepsy revealed by diffusion spectrum imaging. Neuroimage Clin 5:349–358. https://doi.org/10.1016/j.nicl.2014.07.013
Li X, Jiang Y, Li W et al (2022) Disrupted functional connectivity in white matter resting-state networks in unilateral temporal lobe epilepsy. Brain Imaging Behav 16:324–335. https://doi.org/10.1007/s11682-021-00506-8
Mancuso L, Costa T, Nani A et al (2019) The homotopic connectivity of the functional brain: a meta-analytic approach. Sci Rep 9:3346. https://doi.org/10.1038/s41598-019-40188-3
Shi K, Pang X, Wang Y, Li C, Long Q, Zheng J (2021) Altered interhemispheric functional homotopy and connectivity in temporal lobe epilepsy based on fMRI and multivariate pattern analysis. Neuroradiology 63:1873–1882. https://doi.org/10.1007/s00234-021-02706-x
Marinazzo D, Liao W, Chen H, Stramaglia S (2011) Nonlinear connectivity by Granger causality. Neuroimage 58:330–338. https://doi.org/10.1016/j.neuroimage.2010.01.099
Burianova H, Faizo NL, Gray M, Hocking J, Galloway G, Reutens D (2017) Altered functional connectivity in mesial temporal lobe epilepsy. Epilepsy Res 137:45–52. https://doi.org/10.1016/j.eplepsyres.2017.09.001
Jokeit H, Luerding R, Ebner A (2000) Cognitive impairment in temporal-lobe epilepsy. Lancet 355:1018–1019. https://doi.org/10.1016/S0140-6736(05)74765-6
Sun YM, Peng YX, Wen Q et al (2021) Resting-state fMRI in temporal lobe epilepsy patients with cognitive impairment: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 100:e27249. https://doi.org/10.1097/MD.0000000000027249
Raz A, Buhle J (2006) Typologies of attentional networks. Nat Rev Neurosci 7:367–379. https://doi.org/10.1038/nrn1903
Posner MI, Petersen SE (1990) The attention system of the human brain. Annu Rev Neurosci 13:25–42. https://doi.org/10.1146/annurev.ne.13.030190.000325
Fan J, McCandliss BD, Fossella J, Flombaum JI, Posner MI (2005) The activation of attentional networks. Neuroimage 26:471–479. https://doi.org/10.1016/j.neuroimage.2005.02.004
Fan J, Bernardi S, Van Dam NT et al (2012) Functional deficits of the attentional networks in autism. Brain Behav 2:647–660. https://doi.org/10.1002/brb3.90
Zhou X, Zhang Z, Liu J, Qin L, Pang X, Zheng J (2019) Disruption and lateralization of cerebellar-cerebral functional networks in right temporal lobe epilepsy: a resting-state fMRI study. Epilepsy Behav 96:80–86. https://doi.org/10.1016/j.yebeh.2019.03.020
Fan J, McCandliss BD, Sommer T, Raz A, Posner MI (2002) Testing the efficiency and independence of attentional networks. J Cogn Neurosci 14:340–347. https://doi.org/10.1162/089892902317361886
Posner MI (2008) Measuring alertness. Ann N Y Acad Sci 1129:193–199. https://doi.org/10.1196/annals.1417.011
Shi Y, Liu W, Liu R et al (2019) Investigation of the emotional network in depression after stroke: a study of multivariate Granger causality analysis of fMRI data. J Affect Disord 249:35–44. https://doi.org/10.1016/j.jad.2019.02.020
Qiao PF, Niu GM (2017) Resting-state fMRI findings in patients with first-episode idiopathic epilepsy before and after treatment. Neurosciences (Riyadh) 22:316–319. https://doi.org/10.17712/nsj.2017.4.20160650
Zhang Z, Zhou X, Liu J et al (2020) Longitudinal assessment of resting-state fMRI in temporal lobe epilepsy: a two-year follow-up study. Epilepsy Behav 103:106858. https://doi.org/10.1016/j.yebeh.2019.106858
Miller EK, Cohen JD (2001) An integrative theory of prefrontal cortex function. Annu Rev Neurosci 24:167–202. https://doi.org/10.1146/annurev.neuro.24.1.167
Michalski LJ, Demers CH, Baranger DAA et al (2017) Perceived stress is associated with increased rostral middle frontal gyrus cortical thickness: a family-based and discordant-sibling investigation. Genes Brain Behav 16:781–789. https://doi.org/10.1111/gbb.12404
Yang H, Zhang C, Liu C et al (2018) Brain network alteration in patients with temporal lobe epilepsy with cognitive impairment. Epilepsy Behav 81:41–48. https://doi.org/10.1016/j.yebeh.2018.01.024
Zhang C, Yang H, Qin W et al (2017) Characteristics of resting-state functional connectivity in intractable unilateral temporal lobe epilepsy patients with impaired executive control function. Front Hum Neurosci 11:609. https://doi.org/10.3389/fnhum.2017.00609
Thiebaut de Schotten M, Urbanski M, Valabregue R, Bayle DJ, Volle E (2014) Subdivision of the occipital lobes: an anatomical and functional MRI connectivity study. Cortex 56:121–137. https://doi.org/10.1016/j.cortex.2012.12.007
Gong L, Xu R, Liu D et al (2020) Abnormal functional connectivity density in patients with major depressive disorder with comorbid insomnia. J Affect Disord 266:417–423. https://doi.org/10.1016/j.jad.2020.01.088
Huang Q, Xiao M, Ai M et al (2021) Disruption of neural activity and functional connectivity in adolescents with major depressive disorder who engage in non-suicidal self-injury: a resting-state fMRI study. Front Psychiatry 12:571532. https://doi.org/10.3389/fpsyt.2021.571532
Yang YL, Deng HX, Xing GY, Xia XL, Li HF (2015) Brain functional network connectivity based on a visual task: visual information processing-related brain regions are significantly activated in the task state. Neural Regen Res 10:298–307. https://doi.org/10.4103/1673-5374.152386
Zhang Z, Lu G, Zhong Y et al (2009) Impaired perceptual networks in temporal lobe epilepsy revealed by resting fMRI. J Neurol 256:1705–1713. https://doi.org/10.1007/s00415-009-5187-2
Ji GJ, Zhang Z, Zhang H et al (2013) Disrupted causal connectivity in mesial temporal lobe epilepsy. PLoS ONE 8:e63183. https://doi.org/10.1371/journal.pone.0063183
Power JD, Cohen AL, Nelson SM et al (2011) Functional network organization of the human brain. Neuron 72:665–678. https://doi.org/10.1016/j.neuron.2011.09.006
Zhang R, Volkow ND (2019) Brain default-mode network dysfunction in addiction. Neuroimage 200:313–331. https://doi.org/10.1016/j.neuroimage.2019.06.036
Mohan A, Roberto AJ, Mohan A et al (2016) The significance of the default mode network (DMN) in neurological and neuropsychiatric disorders: a review. Yale J Biol Med 89:49–57
MacEachern SJ, Santoro JD, Hahn KJ et al (2020) Children with epilepsy demonstrate macro- and microstructural changes in the thalamus, putamen, and amygdala. Neuroradiology 62:389–397. https://doi.org/10.1007/s00234-019-02332-8
Li W, Qin W, Liu H et al (2013) Subregions of the human superior frontal gyrus and their connections. Neuroimage 78:46–58. https://doi.org/10.1016/j.neuroimage.2013.04.011
Levy R, Goldman-Rakic PS (2000) Segregation of working memory functions within the dorsolateral prefrontal cortex. Exp Brain Res 133:23–32. https://doi.org/10.1007/s002210000397
Desgranges B, Baron JC, Eustache F (1998) The functional neuroanatomy of episodic memory: the role of the frontal lobes, the hippocampal formation, and other areas. Neuroimage 8:198–213. https://doi.org/10.1006/nimg.1998.0359
Corbetta M, Patel G, Shulman GL (2008) The reorienting system of the human brain: from environment to theory of mind. Neuron 58:306–324. https://doi.org/10.1016/j.neuron.2008.04.017
Buckner RL (2013) The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron 80:807–815. https://doi.org/10.1016/j.neuron.2013.10.044
Guell X, Gabrieli JDE, Schmahmann JD (2018) Triple representation of language, working memory, social and emotion processing in the cerebellum: convergent evidence from task and seed-based resting-state fMRI analyses in a single large cohort. Neuroimage 172:437–449. https://doi.org/10.1016/j.neuroimage.2018.01.082
Hoche F, Guell X, Vangel MG, Sherman JC, Schmahmann JD (2018) The cerebellar cognitive affective/Schmahmann syndrome scale. Brain 141:248–270. https://doi.org/10.1093/brain/awx317
Schmahmann JD, Guell X, Stoodley CJ, Halko MA (2019) The theory and neuroscience of cerebellar cognition. Annu Rev Neurosci 42:337–364. https://doi.org/10.1146/annurev-neuro-070918-050258
Schmahmann JD, Macmore J, Vangel M (2009) Cerebellar stroke without motor deficit: clinical evidence for motor and non-motor domains within the human cerebellum. Neuroscience 162:852–861. https://doi.org/10.1016/j.neuroscience.2009.06.023
Chen Z, Zhang R, Huo H, Liu P, Zhang C, Feng T (2022) Functional connectome of human cerebellum. Neuroimage 251:119015. https://doi.org/10.1016/j.neuroimage.2022.119015
Zanao TA, Lopes TM, de Campos BM, Yasuda CL, Cendes F (2021) Patterns of default mode network in temporal lobe epilepsy with and without hippocampal sclerosis. Epilepsy Behav 121:106523. https://doi.org/10.1016/j.yebeh.2019.106523
Vaccaro MG, Trimboli M, Scarpazza C et al (2018) Neuropsychological profile of mild temporal lobe epilepsy. Epilepsy Behav 85:222–226. https://doi.org/10.1016/j.yebeh.2018.06.013
Labate A, Aguglia U, Tripepi G et al (2016) Long-term outcome of mild mesial temporal lobe epilepsy: a prospective longitudinal cohort study. Neurology 86:1904–1910. https://doi.org/10.1212/WNL.0000000000002674
Lopez SM, Aksman LM, Oxtoby NP et al (2022) Event-based modeling in temporal lobe epilepsy demonstrates progressive atrophy from cross-sectional data. Epilepsia 63:2081–2095. https://doi.org/10.1111/epi.17316
Acknowledgements
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided. A previous version of this manuscript has been preprinted on Authorea (https://doi.org/10.22541/au.167146514.42115408/v1).
Funding
The work is supported by the Natural Science Foundation of Guangxi Province (2018GXNSFAA050149).
Author information
Authors and Affiliations
Contributions
The contributions are as follows. Ke Shi: data analysis and writing of the paper draft. Lu Yu: methodology and modification of paper draft. Yiling Wang: literature research and visualization. Zhekun Li, Chunyan Li, and Qijia Long: data acquisition. Jinou Zheng: conceptualization, study design, and supervision.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Medical Research Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (2020-KY-GUOJI-010).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, K., Yu, L., Wang, Y. et al. Impaired interhemispheric synchrony and effective connectivity in right temporal lobe epilepsy. Neurol Sci 45, 2211–2221 (2024). https://doi.org/10.1007/s10072-023-07198-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07198-6