Abstract
Study objective
This study aims to investigate the characteristics of patients with an initial diagnosis of systemic lupus erythematosus (SLE) in an emergency department (ED) and their outcomes.
Methods
A total of 147 SLE patients (119 females and 28 males, mean age 26 ± 19 years) who visited the ED of the Peking University People’s Hospital between January 2017 and June 2022 were enrolled in the study. Data on demographic information, clinical characteristics, comorbidities, therapy, and outcomes were collected.
Results
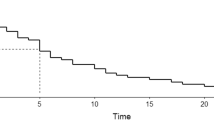
Most patients visit ED because of symptoms related to SLE (74.8%, 110/147). The remaining 37 patients (25.2%) visited ED due to infection (43.2%, 16/37), gastrointestinal bleeding (10.8%, 4/37), coronary heart or cerebrovascular disease (18.9%, 7/37), macrophage activation syndrome or thrombotic microangiopathy (18.9%, 7/37), leukemia (5.4%, 2/37), and hepatic encephalopathy (2.7%, 1/37). Of the patients, 54.4% (80/147) were first diagnosed with SLE at the time of their ED visit. Thrombocytopenia events occurred significantly more frequently in this group of patients (OR 3.664, 95% CI 1.586–8.464, p = 0.002). Pulse steroid therapy was administered to 32.5% (26/80) of the patients with an initial diagnosis of SLE, and 26.3% (21/80) of these patients also received IVIG therapy during their ED visit. SLEDAI scores were significantly decreased after 6 months of therapy. The rate of mortality was 6.8% (10/147) in the 6-month follow-up period, and all the ten deaths happened in patients with disease-established SLE. The main causes of death were infections (two patients) and SLE flare (four patients).
Conclusion
Understanding disease patterns can contribute to physicians providing accurate diagnosis and efficient care for SLE patients in ED.
Key Points |
• Systemic lupus erythematosus, a complex autoimmune disorder, can have either a chronic or a relapsing and remitting disease course. The disease can involve acute events or severe comorbidities, and frequent visits to the emergency department (ED) are inevitable. • It is essential to better understand which comorbidities can lead to emergency department visits. Accurate clinical diagnosis and appropriate interventions from ED physicians can have a strong impact on the prognosis of the disease. • Hematologic compromise attributed to SLE flare is the most common reason for ED visits. Owing to aggressive treatments, the clinical outcomes in patients with initial diagnosis of SLE have improved notably. • Our study highlights that early recognition and appropriate management of SLE-related conditions and other comorbidity in ED are crucial. |



Similar content being viewed by others
Data availability
The original contributions presented in the study are included in the article, and further inquiries can be directed to the corresponding author.
References
Durcan L, O’Dwyer T, Petri M (2019) Management strategies and future directions for systemic lupus erythematosus in adults. Lancet 393(10188):2332–2343. https://doi.org/10.1016/S0140-6736(19)30237-5
Prianka P, Jiang SH, Yang Y, Fabienne M, Di Y (2021) Understand SLE heterogeneity in the era of omics, big data, and artificial intelligence. Rheumatol Autoimmun 01(1):40–51. https://doi.org/10.1002/rai2.12010
Rahman P, Gladman DD, Urowitz MB, Hallett D, Tam LS (2001) Early damage as measured by the SLICC/ACR damage index is a predictor of mortality in systemic lupus erythematosus. Lupus 10(2):93–96. https://doi.org/10.1191/096120301670679959
Barber M, Drenkard C, Falasinnu T et al (2021) Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol 17(9):515–532. https://doi.org/10.1038/s41584-021-00668-1
Arnaud L, Tektonidou MG (2020) Long-term outcomes in systemic lupus erythematosus: trends over time and major contributors. Rheumatology (Oxford) 59(Suppl5):v29–v38. https://doi.org/10.1093/rheumatology/keaa382
Wang Z, Wang Y, Zhu R et al (2015) Long-term survival and death causes of systemic lupus erythematosus in China: a systemic review of observational studies. Medicine (Baltimore) 94(17):e794. https://doi.org/10.1097/MD.0000000000000794
Tanaka Y, O’Neill S, Li M, Tsai IC, Yang YW (2022) Systemic lupus erythematosus: targeted literature review of the epidemiology, current treatment, and disease burden in the Asia Pacific Region. Arthritis Care Res (Hoboken) 74(2):187–198. https://doi.org/10.1002/acr.24431
Thomas G, Mancini J, Jourde-Chiche N et al (2014) Mortality associated with systemic lupus erythematosus in France assessed by multiple-cause-of-death analysis. Arthritis Rheumatol 66(9):2503–2511. https://doi.org/10.1002/art.38731
Panopalis P, Gillis JZ, Yazdany J et al (2010) Frequent use of the emergency department among persons with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 62(3):401–408. https://doi.org/10.1002/acr.20107
Chen Y, Chen GL, Zhu CQ, Lu X, Ye S, Yang CD (2011) Severe systemic lupus erythematosus in emergency department: a retrospective single-center study from China. Clin Rheumatol 30(11):1463–1469. https://doi.org/10.1007/s10067-011-1826-y
Wen LS, Xu J, Steptoe AP et al (2013) Emergency department characteristics and capabilities in Beijing China. J Emerg Med 44(6):1174–1179.e4. https://doi.org/10.1016/j.jemermed.2012.07.083
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Petri M, Orbai AM, Alarcón GS et al (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Isenberg DA, Rahman A, Allen E et al (2005) BILAG 2004. Development and initial validation of an updated version of the British Isles Lupus Assessment Group’s disease activity index for patients with systemic lupus erythematosus. Rheumatology (Oxford) 44(7):902-906. https://doi.org/10.1093/rheumatology/keh624
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Crayne CB, Albeituni S, Nichols KE, Cron RQ (2019) The immunology of macrophage activation syndrome. Front Immunol 10:119. https://doi.org/10.3389/fimmu.2019.00119
Yue C, Su J, Gao R et al (2018) Characteristics and outcomes of patients with systemic lupus erythematosus-associated thrombotic microangiopathy, and their acquired ADAMTS13 inhibitor profiles. J Rheumatol 45(11):1549–1556. https://doi.org/10.3899/jrheum.170811
Jiang H, An X, Li Y et al (2014) Clinical features and prognostic factors of thrombotic thrombocytopenic purpura associated with systemic lupus erythematosus: a literature review of 105 cases from 1999 to 2011. Clin Rheumatol 33(3):419–427. https://doi.org/10.1007/s10067-013-2312-5
Costa Pires T, Caparrós-Ruiz R, Gaspar P, Isenberg DA (2021) Prevalence and outcome of thrombocytopenia in systemic lupus erythematous: single-centre cohort analysis. Clin Exp Rheumatol 39(3):601–605. https://doi.org/10.55563/clinexprheumatol/bz64na
Kokori SI, Ioannidis JP, Voulgarelis M, Tzioufas AG, Moutsopoulos HM (2000) Autoimmune hemolytic anemia in patients with systemic lupus erythematosus. Am J Med 108(3):198–204. https://doi.org/10.1016/s0002-9343(99)00413-1
Kasitanon N, Louthrenoo W, Piyasirisilp S, Sukitawu W, Wichainun R (2002) Neuropsychiatric manifestations in Thai patients with systemic lupus erythematosus. Asian Pac J Allergy Immunol 20(3):179–185
Thomas G, Cohen Aubart F, Chiche L et al (2017) Lupus myocarditis: initial presentation and longterm outcomes in a multicentric series of 29 patients. J Rheumatol 44(1):24–32. https://doi.org/10.3899/jrheum.160493
Li D, Yoshida K, Feldman CH et al (2020) Initial disease severity, cardiovascular events and all-cause mortality among patients with systemic lupus erythematosus. Rheumatology (Oxford) 59(3):495–504. https://doi.org/10.1093/rheumatology/kez288
Kernder A, Richter JG, Fischer-Betz R et al (2021) Delayed diagnosis adversely affects outcome in systemic lupus erythematosus: cross sectional analysis of the LuLa cohort. Lupus 30(3):431–438. https://doi.org/10.1177/0961203320983445
Nagai Y, Yokogawa N, Shimada K, Sugii S (2019) Characteristics and risk factors of an emergency department visit in patients with systemic lupus erythematosus. Rheumatol Int 39(9):1567–1573. https://doi.org/10.1007/s00296-019-04377-7
Liang H, Pan HF, Tao JH, Ye DQ (2019) Causes and factors associated with frequent hospitalization in chinese patients with systemic lupus erythematosus: an ambispective cohort study. Med Sci Monit 25:8061–8068. https://doi.org/10.12659/MSM.919381
Lee J, Peschken CA, Muangchan C et al (2013) The frequency of and associations with hospitalization secondary to lupus flares from the 1000 Faces of Lupus Canadian cohort. Lupus 22(13):1341–1348. https://doi.org/10.1177/0961203313505689
Lee JW, Park DJ, Kang JH et al (2016) The rate of and risk factors for frequent hospitalization in systemic lupus erythematosus: results from the Korean lupus network registry. Lupus 25(13):1412–1419. https://doi.org/10.1177/0961203316640916
Manadan AM, Kambhatla S, Gauto-Mariotti E, Okoli C, Block JA (2020) Reasons for hospitalization and in-hospital mortality in adult systemic lupus erythematosus. ACR Open Rheumatol 2(11):683–689. https://doi.org/10.1002/acr2.11195
Han GM, Han XF (2017) Comorbid conditions are associated with emergency department visits, hospitalizations, and medical charges of patients with systemic lupus erythematosus. J Clin Rheumatol 23(1):19–25. https://doi.org/10.1097/RHU.0000000000000437
Wu W, Ma J, Zhou Y et al (2019) Mortality risk prediction in lupus patients complicated with invasive infection in the emergency department: LUPHAS score. Ther Adv Musculoskelet Dis 11:1759720X19885559. https://doi.org/10.1177/1759720X19885559
Parra Sánchez AR, Voskuyl AE, van Vollenhoven RF (2022) Treat-to-target in systemic lupus erythematosus: advancing towards its implementation. Nat Rev Rheumatol 18(3):146–157. https://doi.org/10.1038/s41584-021-00739-3
Pivovarova AI, Thongprayoon C, Hansrivijit P et al (2020) Thrombotic microangiopathy among hospitalized patients with systemic lupus erythematosus in the United States. Diseases 9(1):3. https://doi.org/10.3390/diseases9010003
Long B, Bridwell RE, Manchanda S, Gottlieb M (2021) Evaluation and management of thrombotic thrombocytopenic purpura in the emergency department. J Emerg Med 61(6):674–682. https://doi.org/10.1016/j.jemermed.2021.07.045
Nam SH, Ahn SM, Oh JS et al (2022) Macrophage activation syndrome in rheumatic disease: clinical characteristics and prognosis of 20 adult patients. PLoS One 17(5):e0267715. https://doi.org/10.1371/journal.pone.0267715
Kim JM, Kwok SK, Ju JH, Kim HY, Park SH (2012) Reactive hemophagocytic syndrome in adult Korean patients with systemic lupus erythematosus: a case-control study and literature review. J Rheumatol 39(1):86–93. https://doi.org/10.3899/jrheum.110639
Gavand PE, Serio I, Arnaud L et al (2017) Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: a study of 103 episodes in 89 adult patients. Autoimmun Rev 16(7):743–749. https://doi.org/10.1016/j.autrev.2017.05.010
Liu AC, Yang Y, Li MT et al (2018) Macrophage activation syndrome in systemic lupus erythematosus: a multicenter, case-control study in China. Clin Rheumatol 37(1):93–100. https://doi.org/10.1007/s10067-017-3625-6
Morrissette K, Bridwell R, Lentz S et al (2021) Hemophagocytic lymphohistiocytosis in the emergency department: recognizing and evaluating a hidden threat. J Emerg Med 60(6):743–751. https://doi.org/10.1016/j.jemermed.2021.02.006
Funding
This work was supported by Peking University People’s Hospital Research and Development Funds (RDJ2022-18 and RD 2022-66).
Author information
Authors and Affiliations
Contributions
XZ, XS, CC, and JZ were responsible for the study concept and design. SL, JL, YJ, JJ, and MS were responsible for data acquisition. XZ, XS, and CC analyzed and interpreted the data. XZ and XS drafted the manuscript. CC provided statistical expertise. All authors were responsible for critical revisions of the article and for the intellectual content.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from the ethical committee of the Peking University People’s Hospital (2023PHB178-001). All research adhered to the tenets of the Declaration of Helsinki. The funding organization had no input on how we conducted the study. Patients and hospital staff were not involved in or aware of the study. The data sharing agreement and the research ethics board approval preclude the sharing of original data.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Song, X., Lv, S. et al. Characteristics of patients with initial diagnosis of systemic lupus erythematosus in emergency department and their outcomes: a retrospective single-center study. Clin Rheumatol 43, 667–676 (2024). https://doi.org/10.1007/s10067-023-06845-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06845-9