Abstract
Introduction and objectives
The recurrence rate of incisional hernia (IH) repair is usually underestimated due to a lack of long-term follow-up. The objective of this study was to evaluate recurrence rate for patients operated on midline IH surgery, using a primary closure and prosthetic onlay technique, 5 years after the procedure.
Materials and methods
From January 2009 to January 2011, all 92 patients operated on elective midline IH repair by primary closure and prosthetic onlay technique in a General Surgery Department were retrospectively included in the study. Exclusion criteria were absence of follow-up or death. Recurrence rate and quality of life were assessed. Demographic, surgical data and quality of life in patients with and without 5-year recurrence were compared.
Results
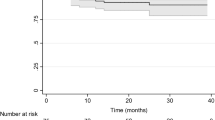
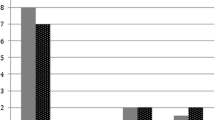
Mean follow-up was 64 months. Ultimately, 76 patients were included in the study, representing 82% of the selected patients during the study period (76/92), of whom 24 presented a recurrence (32%). Half (12) were diagnosed for recurrence more than 3 years after the surgery. Patients who developed a recurrence had more percentage of obesity (64 vs. 29%, p = 0.016), which denoted an odds ratio (OR) for recurrence of 4.4 (1.2–15.7; p = 0.01) and they punctuated lower in quality of life (6.0 ± 2.9 vs. 7.6 ± 2.6, p = 0.006).
Conclusions
Recurrence rate on midline IH repair is still a concern (32% at 5 years). It is advisable to look for other strategies and more efficient surgical techniques for IH surgery, especially in obese patients.

Similar content being viewed by others
References
Sugerman HJ, Kellum JM Jr, Reines HD et al (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171:80–84
Hodgson NC, Malthaner RA, Ostbye T et al (2000) The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 231:436–442
Hoer J, Lawong G, Klinge U et al (2002) Factors influencing the development of incisional hernia: a retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg 73:474–480
Andersen LP, Klein M, Gögenur I et al (2009) Long-term recurrence and complication rates after incisional hernia repair with the open onlay technique. BMC Surg. 28(9):6
Burger JW, Luijendijk RW, Hop WC et al (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583
Fink C, Baumann P, Wente MN et al (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101(2):51–54
Gillion JF, Sanders D, Miserez M, et al (2016) The economic burden of incisional ventral hernia repair: a multicentric cost analysis. Hernia (Epub ahead of print)
Oprea V, Matei O, Leucã D et al (2013) Late results and quality of life after Rives-Stoppa repair for incisional hernias: a prospective clinical study. Chirurgia 108:679–683 (No. 5)
Gysel C (1974) Adolphe Quetelet. The statistics and biometry of growth. Orthod Fr 45(1):643–677
World Health Organization (WHO): obesity and overweight. Fact Sheet No 311. Updated January 2015
Langer S, Christiansen J (1985) Long-term results after incisional hernia repair. Acta Chirst Scand 151(3):217–219
Klinge U, Fiebeler A (2010) Two controversial concepts: standard Procedure in a standard patient versus tailored surgery with procedures adjusted to individual patients. In: Volker S, Fitzgibbons RJ (eds) Hernia repair sequelae. Springer, Berlin, pp 467–472
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237(1):129–135
Cobb WS, Warren JA, Ewing JA et al (2015) Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg 220(4):606–613
Carter SA, Hicks SC, Brahmbhatt R et al (2014) Recurrence and pseudorecurrence after laparoscopic ventral hernia repair: predictors and patient-focused outcomes. Am Surg 80(2):138–148
Vilallonga R, Fort JM, Gonzalez O et al (2011) Management of patients with hernia or incisional hernia undergoing surgery for morbid obesity. J Obes 2011:860942
Raziel A, Sakran N, Szold A et al (2014) Concomitant bariatric and ventral/incisional hernia surgery in morbidly obese patients. Surg Endosc 16(4):1209–1212
Langer C, Schaper A, Liersch T et al (2005) Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia 9(1):16–21
Froylich D, Segal M, Weinstein A et al (2016) Laparoscopic versus open ventral hernia repair in obese patients: a long-term follow-up. Surg Endosc 30(2):670–675
Den Hartog D, Dur AH, Tuinebreijer WE et al (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006438.pub2
Timmermans L, de Goede B, van Dijk SM et al (2014) Meta-analysis of sublay versus onlay mesh repair in incisional hernia surgery. Am J Surg 207(6):980–988
Hernandez-Granados P, Pereira JA, Feliu X, Lopez-Cano M, Fernandez F, Delgado I (2014) Spanish registry of incisional hernia. Preliminary results after 1 year of implementation. Hernia 18(suppl. 2):S31
Kokotovic D, Gögenur I, Helgstrand F (2017) Substantial variation among hernia experts in the decision for treatment of patients with incisional hernia: a descriptive study on agreement. Hernia 21(2):271–278
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526
Cornette B, De Bacquer D, Berrevoet F (2017) Component separation technique for giant incisional hernia: a systematic review. Am J Surg. https://doi.org/10.1016/j.amsurg.2017.07.032
Pauli EM, Rosen MJ (2013) Open ventral hernia repair with component separation. Surg Clin North Am 93(5):1111–1133
Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, Orenstein SB (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264(2):226–232
Sauerland S, Walgenbach M, Habermalz B et al (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007781.pub2
Al Chalabi H, Larkin J, Mehigan B et al (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74
López-Cano M (2013) Evidence-based surgery. Rev Hispanoam Hernia 1(1):18–26
Hoyuela C, Trias M, Juvany M et al (2015) Preoperative progressive pneumoperitoneum and anterior component separation techniques for the treatment of a huge incisional hernia with loss of domain. Cir Esp 93(Special Congress):919
Bueno-Lledó J, Torregrosa A, Ballester N, Carreño O, Carbonell F, Pastor PG, Pamies J, Cortés V, Bonafé S, Iserte J (2017) Preoperative progressive pneumoperitoneum and botulinum toxin type A in patients with large incisional hernia. Hernia 21(2):233–243
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors (MJ, CH, FC, MT, AM, JA) have any conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This study does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Juvany, M., Hoyuela, C., Carvajal, F. et al. Long-term follow-up (at 5 years) of midline incisional hernia repairs using a primary closure and prosthetic onlay technique: recurrence and quality of life. Hernia 22, 319–324 (2018). https://doi.org/10.1007/s10029-018-1730-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1730-3