Abstract
Objectives
While the significant roles of outer membrane vesicles (OMVs) from individual oral bacterial species in bacterial-host interactions are known, the involvement of saliva biofilm-derived OMVs in peri-implant disease pathogenesis remains unclear. This study aimed to investigate the effect of saliva biofilm-derived OMVs on regulating saliva biofilm formation and modulating the immune response of the epithelial cells on titanium surfaces.
Materials and methods
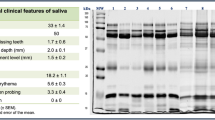
Saliva derived biofilms were cultured on tissue culture plates (TCP) for 4 days using pooled saliva from four healthy donors. OMVs secreted from the TCP bound biofilm (referred to as OMVs or healthy saliva biofilm OMVs) were enriched using the size-exclusion chromatography method. We then evaluated the effects of these OMVs on the viability, metabolic activity, and the presence of oral pathogens in saliva biofilm grown on titanium discs for 24 h and 72 h. Furthermore, the impact of OMVs on the mRNA expression and inflammatory cytokines [interleukin (IL)-6, IL-1α, and monocyte chemoattractant protein-1 (MCP-1)] in human oral epithelial cells (OKF6/TERT-2) was investigated using RT-qPCR and enzyme-linked immunosorbent assay (ELISA), respectively.
Results
Healthy saliva biofilm OMVs improved the biomass and activity of saliva biofilm cultured on the titanium surfaces, with inhibited Porphyromonas gingivalis and Fusobacterium nucleatum, and enhanced Streptococcus mutans expression. Additionally, OMVs increased pro-inflammatory cytokine IL-6 mRNA and IL-6 cytokine expression in human oral epithelial cells. However, IL-1α and MCP-1 cytokines were inhibited 24-hour post-incubation with OMVs.
Conclusion
Healthy saliva biofilm derived OMVs regulate the activity and pathogen composition of biofilms formed on titanium, while modulating the secretion of pro-inflammation factors of oral epithelial cells grown on titanium surfaces.
Clinical relevance
Healthy saliva biofilm OMVs may regulate the early biofilm formation on abutment surfaces and modulate epithelial cell immune response, which may alter the peri-implant niche and participate in the pathogenesis of peri-implant disease.






Similar content being viewed by others
Data Availability
All data collected and analysed within this study are available from the corresponding author on request.
References
Renvert S et al (2018) Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Clin Periodontol 45(Suppl 20):S278–s285
Salvi GE, Monje A, Tomasi C (2018) Long-term biological complications of dental implants placed either in pristine or in augmented sites: a systematic review and meta-analysis. Clin Oral Implants Res 29(Suppl 16):294–310
Salvi GE et al (2022) Physiopathology of peri-implant diseases. Clin Implant Dent Relat Res 25(4):629–639. https://doi.org/10.1111/cid.13167
Lasserre JF, Brecx MC, Toma S (2018) Oral microbes, biofilms and their role in periodontal and peri-implant diseases. Materials (Basel) 11(10):1802
Körtvélyessy G et al (2021) Bioactive coatings for dental implants: a review of alternative strategies to prevent peri-implantitis induced by anaerobic bacteria. Anaerobe 70:102404
Zheng H et al (2015) Subgingival microbiome in patients with healthy and ailing dental implants. Sci Rep 5:10948
Belibasakis GN, Manoil D (2021) Microbial community-driven etiopathogenesis of peri-implantitis. J Dent Res 100(1):21–28
Schwechheimer C, Kuehn MJ (2015) Outer-membrane vesicles from Gram-negative bacteria: biogenesis and functions. Nat Rev Microbiol 13(10):605–619
Chen H et al (2022) Recent advances in biomedical applications of bacterial outer membrane vesicles. J Mater Chem B 10(37):7384–7396
Han P, Bartold PM, Ivanovski S (2022) The emerging role of small extracellular vesicles in saliva and gingival crevicular fluid as diagnostics for periodontitis. J Periodontal Res 57(1):219–231
Ma L, Cao Z (2021) Membrane vesicles from periodontal pathogens and their potential roles in periodontal disease and systemic illnesses. J Periodontal Res 56(4):646–655
Okamura H et al (2021) Outer membrane vesicles of Porphyromonas gingivalis: novel communication tool and strategy. Jpn Dent Sci Rev 57:138–146
Zhang Z et al (2022) Porphyromonas gingivalis outer membrane vesicles inhibit the invasion of Fusobacterium nucleatum into oral epithelial cells by downregulating FadA and FomA. J Periodontol 93(4):515–525
Uemura Y et al (2022) Porphyromonas gingivalis outer membrane vesicles stimulate gingival epithelial cells to induce pro-inflammatory cytokines via the MAPK and STING pathways. Biomedicines 10(10):2643
Oscarsson J et al (2019) Tools of Aggregatibacter actinomycetemcomitans to evade the host response. J Clin Med 8(7):1079
Duan XB et al (2017) Marginal bone loss around non-submerged implants is associated with salivary microbiome during bone healing. Int J Oral Sci 9(2):95–103
Pallos D et al (2021) Salivary microbial dysbiosis is associated with peri-implantitis: a case-control study in a Brazilian population. Front Cell Infect Microbiol 11:696432
Han P et al (2021) Salivary outer membrane vesicles and DNA methylation of small extracellular vesicles as biomarkers for periodontal status: a pilot study. Int J Mol Sci 22(5):2423
Ramachandra SS et al (2023) Fabrication and characterization of a 3D polymicrobial microcosm biofilm model using melt electrowritten scaffolds. Biomater Adv 145:213251
Han P et al (2023) TNF-α and OSX mRNA of salivary small extracellular vesicles in periodontitis: a pilot study. Tissue Eng Part C Methods 29(7):298–306
Liaw A et al (2023) Salivary histone deacetylase in periodontal disease: a cross-sectional pilot study. J Periodontal Res 58(2):433–443
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Clin Periodontol 45(Suppl 20):S149–s161
Ramachandra SS et al (2023) An in vitro dynamic bioreactor model for evaluating antimicrobial effectiveness on periodontal polymicrobial biofilms: a proof-of-concept study. J Periodontol. https://doi.org/10.1002/JPER.23-0086. Epub ahead of print
Han PA-O et al (2022) Iron accumulation is associated with periodontal destruction in a mouse model of HFE-related haemochromatosis. J Periodontal Res 57(2) (1600-0765 (Electronic)):294–304
Han P et al (2023) Saliva diagnosis using small extracellular vesicles and salivaomics. Methods Mol Biol 2588:25–39
Han P et al (2023) TNF-αand OSX mRNA of salivary small extracellular vesicles in periodontitis: a pilot study. Tissue Eng 29(7):298–306. https://doi.org/10.1089/ten.TEC.2023.0051
Han P et al (2023) Effects of periodontal cells-derived extracellular vesicles on mesenchymal stromal cell function. J Periodontal Res 58(6):1188–1200. https://doi.org/10.1111/jre.13171
Théry C et al (2018) Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles 7(1):1535750
Walker SA et al (2022) Sucrose-based cryoprotective storage of extracellular vesicles. Extracell Vesicle 1:100016
Guo T et al (2021) Influence of sterilization on the performance of anodized nanoporous titanium implants. Mater Sci Eng: C 130:112429
Jayasree A et al (2022) Electrochemically nano-engineered titanium: influence of dual micro-nanotopography of anisotropic nanopores on bioactivity and antimicrobial activity. Mater Today Adv 15:100256
Chen X et al (2020) Influence of biofilm growth age, media, antibiotic concentration and exposure time on Staphylococcus aureus and Pseudomonas aeruginosa biofilm removal in vitro. BMC Microbiol 20(1):1–11
Sauer K et al (2022) The biofilm life cycle: expanding the conceptual model of biofilm formation. Nat Rev Microbiol 20(10):608–620
Jayasree A et al (2022) Gallium-doped dual micro-nano titanium dental implants towards soft-tissue integration and bactericidal functions. Mater Today Adv 16:100297
Han P et al (2020) Detection of salivary small extracellular vesicles associated inflammatory cytokines gene methylation in gingivitis. Int J Mol Sci 21(15):5273
Rajasekar A, Varghese SS (2022) Microbiological profile in periodontitis and peri-implantitis: a systematic review. J Long Term Eff Med Implants 32(4):83–94
Quirynen M et al (2006) Dynamics of initial subgingival colonization of ‘pristine’ peri-implant pockets. Clin Oral Implants Res 17(1):25–37
Fürst MM et al (2007) Bacterial colonization immediately after installation on oral titanium implants. Clin Oral Implants Res 18(4):501–508
Nice JB et al (2018) Aggregatibacter actinomycetemcomitans leukotoxin is delivered to host cells in an LFA-1-indepdendent manner when associated with outer membrane vesicles. Toxins (Basel) 10(10):414
Lim Y et al (2022) Activation of bone marrow-derived dendritic cells and CD4(+) T cell differentiation by outer membrane vesicles of periodontal pathogens. J Oral Microbiol 14(1):2123550
Lynch JB, Alegado RA (2017) Spheres of hope, packets of doom: the good and bad of outer membrane vesicles in interspecies and ecological dynamics. J Bacteriol 199(15). https://doi.org/10.1128/jb.00012-17
Kamaguchi A et al (2003) Effect of Porphyromonas gingivalis vesicles on coaggregation of Staphylococcus aureus to oral microorganisms. Curr Microbiol 47(6):485–491
Yonezawa H et al (2009) Outer membrane vesicles of Helicobacter pylori TK1402 are involved in biofilm formation. BMC Microbiol 9:197
Seike S et al (2020) Outer membrane vesicles released from Aeromonas strains are involved in the biofilm formation. Front Microbiol 11:613650
Zhao Z et al (2022) Regulation of the formation and structure of biofilms by quorum sensing signal molecules packaged in outer membrane vesicles. Sci Total Environ 806(Pt 4):151403
da Silva Barreira D et al (2023) Membrane vesicles released by Lacticaseibacillus casei BL23 inhibit the biofilm formation of Salmonella enteritidis. Sci Rep 13(1):1163
Wang Y et al (2021) Inhibition of Streptococcus mutans biofilms with bacterial-derived outer membrane vesicles. BMC Microbiol 21(1):234
Furuta N et al (2009) Porphyromonas gingivalis outer membrane vesicles enter human epithelial cells via an endocytic pathway and are sorted to lysosomal compartments. Infect Immun 77(10):4187–4196
Cañas MA et al (2018) Outer membrane vesicles from probiotic and commensal Escherichia coli activate NOD1-mediated immune responses in intestinal epithelial cells. Front Microbiol 9:498
Ahmadi Badi S et al (2019) Induction effects of Bacteroides fragilis derived outer membrane vesicles on toll like receptor 2, toll like receptor 4 genes expression and cytokines concentration in human intestinal epithelial cells. Cell J 21(1):57–61
Fábrega MJ et al (2017) Intestinal anti-inflammatory effects of outer membrane vesicles from Escherichia coli Nissle 1917 in DSS-experimental colitis in mice. Front Microbiol 8:1274
Caruana JC, Walper SA (2020) Bacterial membrane vesicles as mediators of microbe-microbe and microbe-host community interactions. Front Microbiol 11:432
Funding
This work was supported by the National Natural Science Foundation of China (No. 82271005), the Guangdong Basic and Applied Basic Research Foundation, China (No. 2021A1515010821), the International Team for Implantology (ITI, grant number 1586_2021), Osteology Foundation (Grant No. 20-162), and grant from the China Scholarship Council to BH.
Author information
Authors and Affiliations
Contributions
B.H., P.H., and S.I. conceptualized this study. C.L. collected the samples. J.Y. prepared the titanium disc. B.H., C.L., and E.X. performed the experiments, and data analysis and drafted the manuscript. P.H. and S.I. guided B.H. and C.L. on data interpretation, and critically reviewed and revised the manuscript. All authors approved the article submission.
Corresponding authors
Ethics declarations
Ethics approval
The current study was conducted in accordance with the World Medical Association Declaration of Helsinki (version, 2013). The ethical approval was obtained from The University of Queensland, institutional human ethics committee, approval number HREC2019/HE001113.
Consent to participate
The written informed consent of all the participating subjects was obtained prior to enrolling in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 750 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, B., Liu, C., Yang, J. et al. Saliva biofilm-derived outer membrane vesicles regulate biofilm formation and immune response of oral epithelial cells on titanium surfaces. Clin Oral Invest 28, 75 (2024). https://doi.org/10.1007/s00784-023-05454-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05454-9