Abstract
Objective
To conduct a systematic review to determine the global prevalence of HPV in oral squamous cell carcinoma (OSCC) and oropharyngeal squamous cell carcinoma (OPSCC).
Materials and methods
Literature was searched through October 2022 in main databases to address the question “What is the global prevalence of Human Papillomavirus in oral and oropharyngeal cancer?” Studies had to identify HPV by PCR, ISH, or p16 immunohistochemistry to be eligible. Quality was assessed using the JBI checklist for prevalence studies. Meta-analyses were performed, and reporting followed PRISMA guidelines.
Results
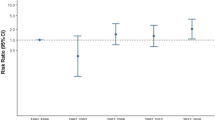
Sixty-five studies were included, and most of them had methodological limitations related to sampling and the HPV detection tool. The pooled prevalence of HPV-positivity was 10% (event rate = 0.1; 95% CI: 0.07, 0.13; P < 0.01; I2 = 88%) in the oral cavity and 42% (event rate = 0.42; 95% CI: 0.36, 0.49; P = 0.02; I2 = 97%) in oropharynx. The highest HPV prevalence in OSCC was reached by Japan, meanwhile, in OPSCC, Finland and Sweden were the most prevalent. HPV16 is the genotype most frequent with 69% in OSCC and 89% in OPSCC, being the tonsils the intraoral location more affected by HPV (63%, p < 0.01, I2 76%).
Conclusion
The evidence points to an apparent burden in HPV-related OPSCC, mostly in North America, Northern Europe, and Oceania, especially due to the HPV16 infection suggesting different trends across continents.
Clinical relevance
This updated systematic review and meta-analysis provide sufficient evidence about the global HPV prevalence in OSCC and OPSCC and the most frequent HPV subtype worldwide.





Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C (2015) Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol 33(29):3235–3242
O’Connor M, O’Donovan B, Waller J et al (2020) Communicating about HPV in the context of head and neck cancer: a systematic review of quantitative studies. Patient Educ Couns 103(3):462–472
Stevens TM, Bishop JA (2017) HPV-related carcinomas of the head and neck: morphologic features, variants, and practical considerations for the surgical pathologist. Virchows Arch 471(2):295–307
Nopmaneepaisarn T, Tangjaturonrasme N, Rawangban W, Vinayanuwattikun C, Keelawat S, Bychkov A (2019) Low prevalence of p16-positive HPV-related head-neck cancers in Thailand: tertiary referral center experience. BMC Cancer 19(1):1050
Berman TA, Schiller JT (2017) Human papillomavirus in cervical cancer and oropharyngeal cancer: one cause, two diseases. Cancer 123(12):2219–2229
Yakin M, Seo B, Hussaini H, Rich A, Hunter K (2019) Human papillomavirus and oral and oropharyngeal carcinoma: the essentials. Aust Dent J 64(1):11–18
Trzcinska A, Zhang W, Gitman M, Westra WH (2020) The prevalence, anatomic distribution and significance of HPV genotypes in head and neck squamous papillomas as detected by real-time PCR and Sanger sequencing. Head Neck Pathol 14(2):428–434
Eggersmann TK, Baumeister P, Kumbrink J et al (2020) Oropharyngeal HPV detection techniques in HPV-associated head and neck cancer patients. Anticancer Res 40(4):2117–2123
Chai RC, Lambie D, Verma M, Punyadeera C (2015) Current trends in the etiology and diagnosis of HPV-related head and neck cancers. Cancer Med 4(4):596–607
Amin MB, Greene FL, Edge SB et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67(2):93–99
de la Cour CD, Sperling CD, Belmonte F, Syrjanen S, Kjaer SK (2021) Human papillomavirus prevalence in oral potentially malignant disorders: systematic review and meta-analysis. Oral Dis 27(3):431–438
Syrjanen S, Lodi G, von Bultzingslowen I et al (2011) Human papillomaviruses in oral carcinoma and oral potentially malignant disorders: a systematic review. Oral Dis 17(Suppl 1):58–72
O’Rorke MA, Ellison MV, Murray LJ, Moran M, James J, Anderson LA (2012) Human papillomavirus related head and neck cancer survival: a systematic review and meta-analysis. Oral Oncol 48(12):1191–1201
Miller CS, Johnstone BM (2001) Human papillomavirus as a risk factor for oral squamous cell carcinoma: a meta-analysis, 1982–1997. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91(6):622–635
Saulle R, Semyonov L, Mannocci A et al (2015) Human papillomavirus and cancerous diseases of the head and neck: a systematic review and meta-analysis. Oral Dis 21(4):417–431
Kreimer AR, Clifford GM, Boyle P, Franceschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomark Prev 14(2):9
Page JM, McKenzie JE, Bossuyt PM, et al (2020) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189
Institute JB (2016) JBI critical appraisal checklist for analytical prevalence studies. The Joanna Briggs Institute, Adelaide, SA
El-Naggar A, Chan J, Grandis J, Takata T, editor (2017) WHO classification of head and neck tumours. 4th ed. Lyon: lnternational Agency for Research on Cancer
Akhiwu BI, Akhiwu HO, Afolaranmi T, et al (2021) Characterization of high risk human papilloma virus genotypes associated with oropharyngeal cancers in a Nigerian population. PanAfrican Medical Journal 15(38):40
Bustos D, Pavan J, Carricart S et al (1999) Human papillomavirus detection in oral cancer lesions in the city of Córdoba. Rev Fac Cienc Med 56(1):65–71
Mahal BA, Catalano PJ, Haddad RI et al (2019) Incidence and demographic burden of HPV-associated oropharyngeal head and neck cancers in the United States. Cancer Epidemiol Biomarkers Prev 28(10):1660–1667
Miguel R, Villa L, Cordeiro A, Prado J, Sobrinho J, Kowalski L (1998) Low prevalence of human papillomavirus in a geographic region with a high incidence of head and neck cancer. Amer J Surg 176(5):428-9
Ribeiro KB, Levi JE, Pawlita M et al (2011) Low human papillomavirus prevalence in head and neck cancer: results from two large case-control studies in high-incidence regions. Int J Epidemiol 40(2):489–502
Tsai SC, Huang JY, Lin C, Liaw YP, Lin FC (2019) The association between human papillomavirus infection and head and neck cancer: a population-based cohort study. Medicine (Baltimore) 98(7):e14436
Liao CI, Francoeur AA, Kapp DS, Caesar MAP, Huh WK, Chan JK (2022) Trends in human papillomavirus-associated cancers, demographic characteristics, and vaccinations in the US, 2001–2017. JAMA Netw Open 5(3):e222530
Satgunaseelan L, Gao K, Low TH et al (2021) Profiling high-risk human papillomavirus HPV subtypes in oral squamous cell carcinoma OSCC. Histopathology 79:5–35
Venkatesh A, Elengkumaran S, Ravindran C, Malathi N (2021) Association of human papilloma virus in oral squamous cell carcinoma: an alarming need for human papillomavirus 16 screening in cancer patients. J Pharm Bioallied Sci 13(Suppl 2):S1224–S1227
Adilbay D, Adilbayev G, Kidirbayeva G et al (2018) HPV infection and P16 expression in oral and oropharyngeal cancer in Kazakhstan. Infect Agent Cancer 13:2
Alsbeih G, Al-Harbi N, Bin Judia S, et al (2019) Prevalence of human papillomavirus (HPV) infection and the association with survival in Saudi patients with head and neck squamous cell carcinoma. Cancers (Basel) 11(6):820
Amit M, Ilana K, Avraham SP et al (2016) Trends in human papillomavirus-related oropharyngeal cancer in Israel. Head Neck 38(Suppl 1):E274-278
Antonsson A, Neale RE, Boros S et al (2015) Human papillomavirus status and p16(INK4A) expression in patients with mucosal squamous cell carcinoma of the head and neck in Queensland. Australia Cancer Epidemiol 39(2):174–181
Argirion I, Zarins KR, McHugh J et al (2020) Increasing prevalence of HPV in oropharyngeal carcinoma suggests adaptation of p16 screening in Southeast Asia. J Clin Virol 132:104637
Attner P, Du J, Nasman A et al (2010) The role of human papillomavirus in the increased incidence of base of tongue cancer. Int J Cancer 126(12):2879–2884
Avnstorp MB, Jensen RG, Garnaes E et al (2013) Human papillomavirus and oropharyngeal cancer in Greenland in 1994–2010. Int J Circumpolar Health 72:22386
Baboci L, Holzinger D, Boscolo-Rizzo P et al (2016) Low prevalence of HPV-driven head and neck squamous cell carcinoma in North-East Italy. Papillomavirus Res 2:133–140
Baez A, Almodovar JI, Cantor A et al (2004) High frequency of HPV16-associated head and neck squamous cell carcinoma in the Puerto Rican population. Head Neck 26(9):778–784
Carlander AF, Gronhoj Larsen C, Jensen DH et al (2017) Continuing rise in oropharyngeal cancer in a high HPV prevalence area: a Danish population-based study from 2011 to 2014. Eur J Cancer 70:75–82
Cerezo L, de la Torre A, Hervas A et al (2014) Oropharyngeal cancer related to human papilloma virus: incidence and prognosis in Madrid. Spain Clin Transl Oncol 16(3):301–306
Chaturvedi AK, Engels EA, Pfeiffer RM et al (2011) Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 29(32):4294–4301
Chenevert J, Chiosea S (2012) Incidence of human papillomavirus in oropharyngeal squamous cell carcinomas: now and 50 years ago. Hum Pathol 43(1):17–22
de Abreu PM, Co ACG, Azevedo PL et al (2018) Frequency of HPV in oral cavity squamous cell carcinoma. BMC Cancer 18(1):324
Deng Z, Hasegawa M, Matayoshi S et al (2011) Prevalence and clinical features of human papillomavirus in head and neck squamous cell carcinoma in Okinawa, southern Japan. Eur Arch Otorhinolaryngol 268(11):1625–1631
Dona MG, Rollo F, Pichi B, et al (2020) Evolving profile of HPV-driven oropharyngeal squamous cell carcinoma in a National Cancer Institute in Italy: a 10-year retrospective study. Microorganisms8(10):1498
D’Souza G, Westra WH, Wang SJ et al (2017) Differences in the prevalence of human papillomavirus (HPV) in head and neck squamous cell cancers by sex, race, anatomic tumor site, and HPV detection method. JAMA Oncol 3(2):169–177
Ernster JA, Sciotto CG, O’Brien MM et al (2007) Rising incidence of oropharyngeal cancer and the role of oncogenic human papilloma virus. Laryngoscope 117(12):2115–2128
Faust H, Eldenhed Alwan E, Roslin A, Wennerberg J, Forslund O (2016) Prevalence of human papillomavirus types, viral load and physical status of HPV16 in head and neck squamous cell carcinoma from the South Swedish Health Care Region. J Gen Virol 97(11):2949–2956
Garcia-de Marcos JA, Perez-Zafrilla B, Arriaga A, Arroyo-Rodriguez S, Poblet E (2014) Human papillomavirus in carcinomas of the tongue: clinical and prognostic implications. Int J Oral Maxillofac Surg 43(3):274–280
Garnaes E, Kiss K, Andersen L et al (2015) A high and increasing HPV prevalence in tonsillar cancers in Eastern Denmark, 2000–2010: the largest registry-based study to date. Int J Cancer 136(9):2196–2203
Girardi FM, Wagner VP, Martins MD, Abentroth AL, Hauth LA (2020) Prevalence of p16 expression in oropharyngeal squamous cell carcinoma in southern Brazil. Oral Surg Oral Med Oral Pathol Oral Radiol 130(6):681-691
Habbous S, Chu KP, Lau H et al (2017) Human papillomavirus in oropharyngeal cancer in Canada: analysis of 5 comprehensive cancer centres using multiple imputation. CMAJ 189(32):E1030–E1040
Habbous S, Chu KP, Qiu X et al (2013) The changing incidence of human papillomavirus-associated oropharyngeal cancer using multiple imputation from 2000 to 2010 at a Comprehensive Cancer Centre. Cancer Epidemiol 37(6):820–829
Haeggblom L, Attoff T, Yu J et al (2019) Changes in incidence and prevalence of human papillomavirus in tonsillar and base of tongue cancer during 2000–2016 in the Stockholm region and Sweden. Head Neck 41(6):1583–1590
Hama T, Tokumaru Y, Fujii M et al (2014) Prevalence of human papillomavirus in oropharyngeal cancer: a multicenter study in Japan. Oncology 87(3):173–182
Kabagenyi F, Otiti J, Namwagala J, Kamulegeya A, Kalungi S (2020) A descriptive study of human papilloma virus in upper aero-digestive squamous cell carcinoma at Uganda cancer institute assessed by P16 immunohistochemistry. Cancers Head Neck 5:10
Lam EW, Chan JY, Chan AB et al (2016) Prevalence, clinicopathological characteristics, and outcome of human papillomavirus-associated oropharyngeal cancer in southern Chinese patients. Cancer Epidemiol Biomarkers Prev 25(1):165–173
Liang XH, Lewis J, Foote R, Smith D, Kademani D (2008) Prevalence and significance of human papillomavirus in oral tongue cancer: the Mayo Clinic experience. J Oral Maxillofac Surg 66(9):1875–1880
Lucas-Roxburgh R, Benschop J, Lockett B, van den Heever U, Williams R, Howe L (2017) The prevalence of human papillomavirus in oropharyngeal cancer in a New Zealand population. PLoS ONE 12(10):e0186424
Luginbuhl A, Sanders M, Spiro JD (2009) Prevalence, morphology, and prognosis of human papillomavirus in tonsillar cancer. Annal Otol, Rhinol Laryngol 118(10):742–749
Lundberg M, Leivo I, Saarilahti K, Makitie AA, Mattila PS (2011) Increased incidence of oropharyngeal cancer and p16 expression. Acta Otolaryngol 131(9):1008–1011
Melchers LJ, Mastik MF, Samaniego Cameron B et al (2015) Detection of HPV-associated oropharyngeal tumours in a 16-year cohort: more than meets the eye. Br J Cancer 112(8):1349–1357
Melkane AE, Auperin A, Saulnier P et al (2014) Human papillomavirus prevalence and prognostic implication in oropharyngeal squamous cell carcinomas. Head Neck 36(2):257–265
Mena M, Frias-Gomez J, Taberna M et al (2020) Epidemiology of human papillomavirus-related oropharyngeal cancer in a classically low-burden region of southern Europe. Sci Rep 10(1):13219
Mirghani H, Bellera C, Delaye J et al (2019) Prevalence and characteristics of HPV-driven oropharyngeal cancer in France. Cancer Epidemiol 61:89–94
Nasman A, Attner P, Hammarstedt L et al (2009) Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int J Cancer 125(2):362–366
Nasman A, Nordfors C, Holzhauser S et al (2015) Incidence of human papillomavirus positive tonsillar and base of tongue carcinoma: a stabilisation of an epidemic of viral induced carcinoma? Eur J Cancer 51(1):55–61
Ni G, Huang K, Luan Y et al (2019) Human papillomavirus infection among head and neck squamous cell carcinomas in southern China. PLoS ONE 14(9):e0221045
Nichols AC, Palma DA, Dhaliwal SS et al (2013) The epidemic of human papillomavirus and oropharyngeal cancer in a Canadian population. Curr Oncol 20(4):212–219
Ou P, Gear K, Rahnama F et al (2018) Human papillomavirus and oropharyngeal squamous cell carcinoma: a New Zealand cohort study. ANZ J Surg 88(4):E278–E283
Pennacchiotti G, Sáez R, Martínez MJ, Cárcamo M, Montes R (2016) Prevalencia del virus papiloma humano en pacientes con diagnóstico de carcinoma escamoso de la cavidad oral. Rev Chil Cir 68(2):137–142
Portugal LG, Goldenberg JD, Wenig M et al (1997) Human papillomavirus expression and p53 gene mutations in squamous cell carcinoma. Arch Otolaryngol Head Neck Surg. 123:1230–1234
Purwanto DJ, Soedarsono N, Reuwpassa JO, Adisasmita AC, Ramli M, Djuwita R (2019) The prevalence of oral high-risk HPV infection in Indonesian oral squamous cell carcinoma patients. Oral Dis 26(1):72–80
Rivero ERC, Nunes FD (2006) HPV in oral squamous cell carcinomas of a Brazilian population: amplification by PCR. Braz Oral Res 20(1):21–24
Rodrigo JP, Heideman DA, Garcia-Pedrero JM et al (2014) Time trends in the prevalence of HPV in oropharyngeal squamous cell carcinomas in northern Spain (1990–2009). Int J Cancer 134(2):487–492
Saghravanian N, Zamanzadeh M, Meshkat Z, Afzal Aghaee M, Salek R (2016) Evaluation of the prevalence rate and the prognostic effect of human papilloma virus infection in a group of patients with oral cavity squamous cell carcinoma. Iran J Cancer Prev 9(3):e3998
Shima K, Kobayashi I, Saito I et al (2000) Incidence of human papillomavirus 16 and 18 infection and p53 mutation in patients with oral squamous cell carcinoma in Japan. Br J Oral Maxillofac Surg 38(5):445–450
Simoens C, Gorbaslieva I, Gheit T et al (2021) HPV DNA genotyping, HPV E6*I mRNA detection, and p16(INK4a)/Ki-67 staining in Belgian head and neck cancer patient specimens, collected within the HPV-AHEAD study. Cancer Epidemiol 72:101925
St Guily JL, Jacquard AC, Pretet JL et al (2011) Human papillomavirus genotype distribution in oropharynx and oral cavity cancer in France–the EDiTH VI study. J Clin Virol 51(2):100–104
Strojan P, Zadnik V, Sifrer R et al (2015) Incidence trends in head and neck squamous cell carcinoma in Slovenia, 1983–2009: role of human papillomavirus infection. Eur Arch Otorhinolaryngol 272(12):3805–3814
Tinhofer I, Johrens K, Keilholz U et al (2015) Contribution of human papilloma virus to the incidence of squamous cell carcinoma of the head and neck in a European population with high smoking prevalence. Eur J Cancer 51(4):514–521
Van Limbergen EJ, Dok R, Laenen A et al (2014) HPV-related oropharyngeal cancers in Flanders (Belgium): a multicenter study. B-ENT 10:7–14
Van Rensburg EJ, Engelbrecht S, Van Heerden WFP, Raubennheimer EJ, Schoub BD (1996) Human papillomavirus DNA in oral squamous cell carcinomas from an African population sample. Anticancer Res 16:969–974
Vanshika S, Preeti A, Sumaira Q et al (2021) Incidence OF HPV and EBV in oral cancer and their clinico-pathological correlation- a pilot study of 108 cases. J Oral Biol Craniofac Res 11(2):180–184
Villagomez-Ortiz VJ, Paz-Delgadillo DE, Marino-Martinez I, Cesenas-Falcon LA, Sandoval-de la Fuente A, Reyes-Escobedo A (2016) Prevalence of human papillomavirus infection in squamous cell carcinoma of the oral cavity, oropharynx and larynx. Cir Cir 84(5):363–368
Wang XI, Thomas J, Zhang S (2012) Changing trends in human papillomavirus-associated head and neck squamous cell carcinoma. Ann Diagn Pathol 16(1):7–12
Windon MJ, D’Souza G, Rettig EM et al (2018) Increasing prevalence of human papillomavirus-positive oropharyngeal cancers among older adults. Cancer 124(14):2993–2999
Wittekindt C, Wagner S, Bushnak A et al (2019) Increasing incidence rates of oropharyngeal squamous cell carcinoma in Germany and significance of disease burden attributed to human papillomavirus. Cancer Prev Res (Phila) 12(6):375–382
Naz F, Verma H, Tanveer N, Sudheer AK, Kakkar A, Tanwar P (2022) Demographic profile of p16 immunopositive and HPV DNA PCR positive oral squamous cell carcinoma in a large cohort of Indian patients. Asian Pac J Cancer Prev 23(2):529–536
Oliva C, Carrillo-Beltran D, Boettiger P, Gallegos I, Aguayo F (2022) Human papillomavirus detected in oropharyngeal cancers from Chilean subjects. Viruses 14(6):1212
Rubio-Casadevall J, Ciurana E, Puigdemont M, et al (2022) Population-based analysis of trends in incidence and survival of human papilloma virus-related oropharyngeal cancer in a low-burden region of southern Europe. Int J Environ Res Public Health 19(8):4802
Verma G, Aggarwal N, Chhakara S et al (2021) Detection of human papillomavirus infection in oral cancers reported at dental facility: assessing the utility of FFPE tissues. Med Oncol 39(1):13
Wang CP, Chen TC, Hsu WL et al (2022) Rising incidence of HPV positive oropharyngeal cancer in Taiwan between 1999 and 2014 where betel nut chewing is common. BMC Cancer 22(1):296
Stein AP, Saha S, Kraninger JL et al (2015) Prevalence of human papillomavirus in oropharyngeal cancer: a systematic review. Cancer J 21(3):138–146
Mariz B, Kowalski LP, William WN Jr et al (2020) Global prevalence of human papillomavirus-driven oropharyngeal squamous cell carcinoma following the ASCO guidelines: a systematic review and meta-analysis. Crit Rev Oncol Hematol 156:103116
Matos LL, Miranda GA, Cernea CR (2015) Prevalence of oral and oropharyngeal human papillomavirus infection in Brazilian population studies: a systematic review. Braz J Otorhinolaryngol 81(5):554–567
Nandi S, Mandal A, Chhebbi M (2021) The prevalence and clinicopathological correlation of human papillomavirus in head and neck squamous cell carcinoma in India: a systematic review article. Cancer Treat Res Commun 26:100301
Oliveira AC, Cavalcanti de Lima IC, Frez Marques VM, Alves de Araujo WH, de Campos FC (2022) Human papillomavirus prevalence in oral and oropharyngeal squamous cell carcinoma in South America: a systematic review and meta-analysis. Oncol Rev 16(1):552
Stjernstrom KD, Jensen JS, Jakobsen KK, Gronhoj C, von Buchwald C (2019) Current status of human papillomavirus positivity in oropharyngeal squamous cell carcinoma in Europe: a systematic review. Acta Otolaryngol 139(12):1112–1116
Jayaprakash V, Reid M, Hatton E et al (2011) Human papillomavirus types 16 and 18 in epithelial dysplasia of oral cavity and oropharynx: a meta-analysis, 1985–2010. Oral Oncol 47(11):1048–1054
Kreimer AR, Clifford GM, Boyle P et al (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol, Biomarkers Prevent 14:467–475
Smitha T, Mohan CV, Hemavathy S (2017) Prevalence of human papillomavirus16 DNA and p16(INK4a) protein in oral squamous cell carcinoma: a systematic review and meta-analysis. J Oral Maxillofac Pathol 21(1):76–81
Menezes FDS, Fernandes GA, Antunes JLF, Villa LL, Toporcov TN (2021) Global incidence trends in head and neck cancer for HPV-related and -unrelated subsites: a systematic review of population-based studies. Oral Oncol 115:105177
Castellsague X, Alemany L, Quer M et al (2016) HPV involvement in head and neck cancers: comprehensive assessment of biomarkers in 3680 patients. J Natl Cancer Inst. 108(6):djv403
Clifford GM, Smith JS, Plummer M, Munoz N, Franceschi S (2003) Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 88(1):63–73
Acknowledgements
The authors would like to thank Professor Tina Dalianis, Professor Wei Xu, Professor Christian von Buchwald, and Dr Amanda-Louise Fenger Carlander who kindly answered the e-mails and provided, when necessary, the additional information requested.
Author information
Authors and Affiliations
Contributions
Thamyres Fonseca: Conceptualization, Methodology, Software, Validation, Investigation, Data Curation, Writing—Original Draft, Writing—Review & Editing, Visualization, Project administration.
Lucas Jural: Software, Validation, Investigation, Prepared all figures.
Guido Marañón-Vásquez: Software, formal analysis, Prepared all figures.
Marcela Magno: Software, formal analysis, Data Curation, Prepared all figures.
Ana Luiza Roza: Writing—Original Draft, Writing—Review & Editing.
Daniele Ferreira: Methodology, Software, Data Curation.
Lucianne Coplemaia: Methodology, Validation, Investigation, Writing—Review & Editing, Supervision, Project administration.
Mário Romañach: Writing—Original Draft, Writing—Review & Editing, Visualization.
Michelle Agostini: Conceptualization, Writing—Original Draft, Writing—Review & Editing.
Aline Abrahão: Conceptualization, Writing—Original Draft, Writing—Review & Editing, Visualization, Supervision, Project administration.
All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fonsêca, T.C., Jural, L.A., Marañón-Vásquez, G.A. et al. Global prevalence of human papillomavirus-related oral and oropharyngeal squamous cell carcinomas: a systematic review and meta-analysis. Clin Oral Invest 28, 62 (2024). https://doi.org/10.1007/s00784-023-05425-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05425-0