Abstract
Objective
The aim of this in vitro study is to evaluate the effect of antioxidant lycopene on human osteoblasts.
Material and method
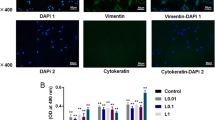
The human osteoblast cell line (CRL-11372) was obtained from the American Type Culture Collection (ATCC Manassas, Va) and grown in Dulbecco’s Modified Eagle’s medium (DMEM) supplemented with 10% fetal calf serum (FCS), penicillin (100 U/ml), and streptomycin (100 mg/ ml) at 37 °C in a humidified atmosphere of 5% CO2 and 95% air. The effective dose of lycopene was determined by MTT assay and a real-time cell analysis (RTCA) system. Proliferative effects were analyzed by in vitro wound healing model. Gene expressions of type 1 collagen (COL1A1), osteocalcin (OCN), and growth differentiation factor-5 (GDF-5) were measured by quantitative real-time polymerase chain reaction (qRT-PCR) at 72 h. Statistical differences between test groups were analyzed with a one-way ANOVA test.
Results
MTT assay showed that the doses between 10−5 and 1 µmol of lycopene had dose-dependent proliferative effects. The doses between 10−5 and 10−1 µmol were most effective at 72 h. Lycopene accelerates the healing rate by increasing osteoblast proliferation.
Conclusion
Results suggested that lycopene had proliferative effects on human osteoblasts, which may help to increase bone regeneration, and thus, it can be useful in tissue engineering procedures.
Clinical relevance
By the help of antioxidants like lycopene capacity, velocity and quality of new bone forming may be increased in periodontal and dental implant treatments.




Similar content being viewed by others
Data availability
Not applicable.
Notes
CRL-11372 cell line, ATCC Manassas, Va.
Lycopene, Sigma, Israel.
THF, Sigma, Israel.
Biological Industries, Beith Haemek, Israel.
Roche Applied Science, Mannheim, Germany.
Ibidi USA Inc., in Fitchburg, Wisconsin
High Pure RNA Isolation Kit, Roche, Mannheim, Germany
Roche, Mannheim, Germany
SPSS Inc., Chicago, IL
References
Van Dyke TE (2008) The management of inflammation in periodontal disease. J Periodontol 79:1601–1608
Hathaway-Schrader JD, Novince CM (2000) (2021) Maintaining homeostatic control of periodontal bone tissue. Periodontol 86:157–187
Kapila YL (2000) (2021) Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 87:11–16
Pamuk F, Kantarci A (2022) Inflammation as a link between periodontal disease and obesity. Periodontology 2000 90(1):186–196
Yucel-Lindberg T, Båge T (2013) Inflammatory mediators in the pathogenesis of periodontitis. Expert Reviews in Molecular Medicine 15(e-7):1–22
Sczepanik FSC, Grossi ML, Casati M, Goldberg M, Glogauer M (2000) Fine N and Tenenbaum HC (2020) Periodontitis is an inflammatory disease of oxidative stress: we should treat it that way. Periodontol 84:45–68
Dahiya P, Kamal R, Gupta R, Bhardwaj R, Chaudhary K, Kaur S (2013) Reactive oxygen species in periodontitis. J Indian Soc Periodontol 17:411
Sharma A, Sharma S (2011) Reactive oxygen species and antioxidants in periodontics: a review. Int J Dent Clin 3:44–48
Andrei M, Dinischiotu A, Didilescu AC, Ionita D, Demetrescu I (2018) Periodontal materials and cell biology for guided tissue and bone regeneration. Annals of Anatomy-Anatomischer Anzeiger 216:164–169
Sulijaya B, Takahashi N, Yamazaki K (2019) Host modulation therapy using anti-inflammatory and antioxidant agents in periodontitis: A review to a clinical translation. Arch Oral Biol 105:72–80
Castro MML, Duarte NN, Nascimento PC, Magno MB, Fagundes NCF, Flores-Mir C, Monteiro MC, Rösing CK, Maia LC, Lima RR (2019) Antioxidants as adjuvants in periodontitis treatment: a systematic review and meta-analysis. Oxidative Med Cell Longev 9187978
Corrêa M, Pires P, Ribeiro F, Pimentel S, Casarin R, Cirano F, Tenenbaum H, Casati M (2017) Systemic treatment with resveratrol and/or curcumin reduces the progression of experimental periodontitis in rats. J Periodontal Res 52:201–209
Rao AV, Ray M, Rao L (2006) Lycopene. Adv Food Nutr Res 51:99–164
Teodoro AJ, Oliveira FL, Martins NB, Maia GdA, Martucci RB, Borojevic R (2012) Effect of lycopene on cell viability and cell cycle progression in human cancer cell lines. Cancer Cell Int 12:1–9
Chen J, Song Y, Zhang L (2013) Effect of lycopene supplementation on oxidative stress: an exploratory systematic review and meta-analysis of randomized controlled trials. J Med Food 16:361–374
Kim L, Rao AV, Rao LG (2003) Lycopene II—effect on osteoblasts: the carotenoid lycopene stimulates cell proliferation and alkaline phosphatase activity of SaOS-2 cells. J Med Food 6:79–86
Russo C, Ferro Y, Maurotti S, Salvati MA, Mazza E, Pujia R, Terracciano R, Maggisano G, Mare R, Giannini S (2020) Lycopene and bone: an in vitro investigation and a pilot prospective clinical study. J Transl Med 18:1–11
Tripathi P, Blaggana V, Upadhyay P, Jindal M, Gupta S, Nishat S (2019) Antioxidant therapy (lycopene and green tea extract) in periodontal disease: a promising paradigm. J Indian Soc of Periodontol 23:25
Viswa Chandra R, Sandhya YP, Nagarajan S, Harish Reddy B, Naveen A, Murthy KRV (2012) Efficacy of lycopene as a locally delivered gel in the treatment of chronic periodontitis: smokers vs nonsmokers. Quintessence Int 43(5):401–411
Chandra RV, Srinivas G, Reddy AA, Reddy BH, Reddy C, Nagarajan S, Naveen A (2013) Locally delivered antioxidant gel as an adjunct to nonsurgical therapy improves measures of oxidative stress and periodontal disease. J Periodont Implant Sci 43:121–129
Rao SM, Ugale GM, Warad SB (2013) Bone morphogenetic proteins: periodontal regeneration. N Am J Med Sci 5:161
Moore YR, Dickinson DP, Wikesjö UM (2010) Growth/differentiation factor-5: a candidate therapeutic agent for periodontal regeneration? A review of pre-clinical data. J Clin Periodontol 37:288–298
Jin L, Li X (2013) Growth differentiation factor 5 regulation in bone regeneration. Curr Pharm Des 19:3364–3373
Florencio-Silva R, Sasso GRdS, Sasso-Cerri E, Simões MJ, Cerri PS (2015) Biology of bone tissue: structure, function, and factors that influence bone cells. BioMed Res Int 2015:421746
Nizam N, Discioglu F, Saygun I, Bal V, Avcu F, Ozkan CK, Serdar MA (2014) The effect of α-tocopherol and selenium on human gingival fibroblasts and periodontal ligament fibroblasts in vitro. J Periodontol 85:636–644
Öztürk F, Malkoc S, Ersöz M, Hakki SS, Bozkurt BS (2011) Real-time cell analysis of the cytotoxicity of the components of orthodontic acrylic materials on gingival fibroblasts. Am J Orthod Dentofac Orthop 140:e243–e249
Zhang H, Chen X, Wang D, Zheng X, Chen Z (2007) The effect of lycopene on osteoblasts which have incurred oxidative stress. Chinese J Osteoporosis 13:86
Hughes FJ, Turner W (2000) Belibasakis G and Martuscelli G (2006) Effects of growth factors and cytokines on osteoblast differentiation. Periodontol 41:48–72
Griffiths G, Moulson A, Petrie A, James I (1998) Evaluation of osteocalcin and pyridinium crosslinks of bone collagen as markers of bone turnover in gingival crevicular fluid during different stages of orthodontic treatment. J Clin Periodontol 25:492–498
Lee J, Wikesjö UM (2014) Growth/differentiation factor-5: pre-clinical and clinical evaluations of periodontal regeneration and alveolar augmentation–review. J Clin Periodontol 41:797–805
Funding
This study is supported by the Gulhane Military Medical Academy, Ankara, Turkey, (Project no: AR2013/31).
Author information
Authors and Affiliations
Contributions
Vahdi Umut Bengi and Isil Saygun conceived the presented idea and developed the theory.
Vahdi Umut Bengi wrote the manuscript with support from Isil Saygun, Vehbi Bal, and Ferit Avcu.
Cansel Kose Ozkan and Deniz Torun performed the analysis and designed the tables and figures.
Erkan Ozcan and Alpdogan Kantarcı contributed to the design and implementation of the research, to the analysis of the results, and to the writing of the manuscript.
All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study has been ethically approved by the Gulhane Military Medical Academy Ethics Committee on the 3rd of April 2013.
Competing interests
The authors report no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bengi V., U., Saygun, I., Bal, V. et al. Effect of antioxidant lycopene on human osteoblasts. Clin Oral Invest 27, 1637–1643 (2023). https://doi.org/10.1007/s00784-022-04789-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04789-z