Abstract
Introduction
To analyze the association between α-tocopherol intake and cadmium (Cd) exposure and osteoporosis in population ≥ 50 years.
Materials and methods
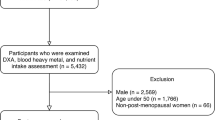
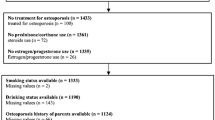
Sociodemographic data, physical examination, and laboratory indicators including serum Cd level and dietary α-tocopherol intake of 8459 participants were extracted from the National Health and Nutrition Examination Survey (NHANES) database in this cross-sectional study. The associations between α-tocopherol intake, serum Cd levels and osteoporosis were evaluated using univariate and multivariate logistic regression analyses, with the estimated value (β), odds ratios (ORs) and 95% confidence intervals (CIs). We further explored the impact of α-tocopherol intake on Cd exposure and the bone mineral density (BMD) in total femur and femur neck.
Results
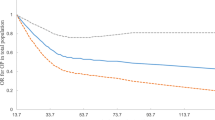
A total of 543 old adults suffered from osteoporosis. The serum Cd level (0.52 μg/L vs. 0.37 μg/L) and α-tocopherol intake (5.28 mg vs. 6.50 mg) were statistical different in osteoporosis group and non-osteoporosis group, respectively. High level of Cd exposure was related to the increased risk of osteoporosis [OR = 1.60, 95% CI (1.15–2.21)]. In the total femur, α-tocopherol intake may improve the loss of BMD that associated with Cd exposure [β = − 0.047, P = 0.037]. Moreover, high α-tocopherol intake combined with low Cd exposure [OR = 0.54, 95% CI (0.36–0.81)] was linked to the decreased risk of osteoporosis comparing with low α-tocopherol intake combined with high Cd exposure.
Conclusion
High α-tocopherol intake may improve the Cd-related osteoporosis and loss of BMD that could provide some dietary reference for prevention of osteoporosis in population ≥ 50 years old.




Similar content being viewed by others
References
Duan W, Meng X, Sun Y, Jia C (2018) Association between polycyclic aromatic hydrocarbons and osteoporosis: data from NHANES, 2005–2014. Arch Osteoporos 13:112. https://doi.org/10.1007/s11657-018-0527-4
Hsieh RL, Huang YL, Chen WJ, Chen HH, Shiue HS, Lin YC, Hsueh YM (2022) Associations between plasma folate and vitamin B12, blood lead, and bone mineral density among adults and elderly who received a health examination. Nutrients 14:4. https://doi.org/10.3390/nu14040911
Wang N, Wang Y, Zhang H, Guo Y, Chen C, Zhang W, Wan H, Han J, Lu Y (2020) Association of bone mineral density with nine urinary personal care and consumer product chemicals and metabolites: a national-representative, population-based study. Environ Int 142:105865. https://doi.org/10.1016/j.envint.2020.105865
Kim Y, Kim JH, Cho DS (2015) Gender difference in osteoporosis prevalence, awareness and treatment: based on the Korea national health and nutrition examination survey 2008–2011. J Korean Acad Nurs 45:293–305. https://doi.org/10.4040/jkan.2015.45.2.293
Elonheimo H, Lange R, Tolonen H, Kolossa-Gehring M (2021) Environmental substances associated with osteoporosis—a scoping review. Int J Environ Res Public Health 18:2. https://doi.org/10.3390/ijerph18020738
Hsueh YM, Huang YL, Chen HH, Shiue HS, Lin YC, Hsieh RL (2021) Alcohol consumption moderated the association between levels of high blood lead or total urinary arsenic and bone loss. Front Endocrinol Lausanne 12:782174. https://doi.org/10.3389/fendo.2021.782174
Lim HS, Lee HH, Kim TH, Lee BR (2016) Relationship between heavy metal exposure and bone mineral density in Korean adult. J Bone Metab 23:223–231. https://doi.org/10.11005/jbm.2016.23.4.223
Jalili C, Kazemi M, Taheri E, Mohammadi H, Boozari B, Hadi A, Moradi S (2020) Exposure to heavy metals and the risk of osteopenia or osteoporosis: a systematic review and meta-analysis. Osteoporos Int 31:1671–1682. https://doi.org/10.1007/s00198-020-05429-6
Scimeca M, Feola M, Romano L, Rao C, Gasbarra E, Bonanno E, Brandi ML, Tarantino U (2017) Heavy metals accumulation affects bone microarchitecture in osteoporotic patients. Environ Toxicol 32:1333–1342. https://doi.org/10.1002/tox.22327
Corrado A, Cici D, Rotondo C, Maruotti N, Cantatore FP (2020) Molecular basis of bone aging. Int J Mol Sci 21:10. https://doi.org/10.3390/ijms21103679
Michaelsson K, Wolk A, Byberg L, Arnlov J, Melhus H (2014) Intake and serum concentrations of alpha-tocopherol in relation to fractures in elderly women and men: 2 cohort studies. Am J Clin Nutr 99:107–114. https://doi.org/10.3945/ajcn.113.064691
Hu D, Cheng L, Jiang W (2018) Fruit and vegetable consumption and the risk of postmenopausal osteoporosis: a meta-analysis of observational studies. Food Funct 9:2607–2616. https://doi.org/10.1039/c8fo00205c
Domazetovic V, Marcucci G, Iantomasi T, Brandi ML, Vincenzini MT (2017) Oxidative stress in bone remodeling: role of antioxidants. Clin Cases Miner Bone Metab 14:209–216. https://doi.org/10.11138/ccmbm/2017.14.1.209
Odai T, Terauchi M, Hirose A, Kato K, Miyasaka N (2019) Bone mineral density in premenopausal women is associated with the dietary intake of alpha-tocopherol: a cross-sectional study. Nutrients 11:10. https://doi.org/10.3390/nu11102474
Cerullo F, Gambassi G, Cesari M (2012) Rationale for antioxidant supplementation in sarcopenia. J Aging Res 2012:316943. https://doi.org/10.1155/2012/316943
Kasai S, Ito A, Shindo K, Toyoshi T, Bando M (2015) High-dose alpha-tocopherol supplementation does not induce bone loss in normal rats. PLoS One 10:e0132059. https://doi.org/10.1371/journal.pone.0132059
Lefèvre T, Haude M, Neumann F-J, Stangl K, Skurk C, Slagboom T, Sabaté M, Goicolea J, Barragan P, Cook S, Macia J-C, Windecker S (2018) Comparison of a novel biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent. JACC Cardiovasc Interv 11:995–1002. https://doi.org/10.1016/j.jcin.2018.04.014
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older US adults from NHANES III. J Bone Miner Res 12:1761–1768. https://doi.org/10.1359/jbmr.1997.12.11.1761
Li R, Xia J, Zhang XI, Gathirua-Mwangi WG, Guo J, Li Y, McKenzie S, Song Y (2018) associations of muscle mass and strength with all-cause mortality among US older adults. Med Sci Sports Exerc 50:458–467. https://doi.org/10.1249/MSS.0000000000001448
Wallin M, Barregard L, Sallsten G, Lundh T, Karlsson MK, Lorentzon M, Ohlsson C, Mellstrom D (2016) Low-level cadmium exposure is associated with decreased bone mineral density and increased risk of incident fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 31:732–741. https://doi.org/10.1002/jbmr.2743
Lv YJ, Song J, Xiong LL, Huang R, Zhu P, Wang P, Liang XX, Tan JB, Wang J, Wu SX, Wei QZ, Yang XF (2021) Association of environmental cadmium exposure and bone remodeling in women over 50 years of age. Ecotoxicol Environ Saf 211:111897. https://doi.org/10.1016/j.ecoenv.2021.111897
Kim ES, Shin S, Lee YJ, Ha IH (2021) Association between blood cadmium levels and the risk of osteopenia and osteoporosis in Korean post-menopausal women. Arch Osteoporos 16:22. https://doi.org/10.1007/s11657-021-00887-9
Galvez-Fernandez M, Grau-Perez M, Garcia-Barrera T, Ramirez-Acosta S, Gomez-Ariza JL, Perez-Gomez B, Galan-Labaca I, Navas-Acien A, Redon J, Briongos-Figuero LS, Duenas-Laita A, Perez-Castrillon JL, Tellez-Plaza M, Martin-Escudero JC (2021) Arsenic, cadmium, and selenium exposures and bone mineral density-related endpoints: the HORTEGA study. Free Radic Biol Med 162:392–400. https://doi.org/10.1016/j.freeradbiomed.2020.10.318
Horiguchi H, Oguma E, Sasaki S, Miyamoto K, Ikeda Y, Machida M, Kayama F (2005) Environmental exposure to cadmium at a level insufficient to induce renal tubular dysfunction does not affect bone density among female Japanese farmers. Environ Res 97:83–92. https://doi.org/10.1016/j.envres.2004.03.004
Luo H, Gu R, Ouyang H, Wang L, Shi S, Ji Y, Bao B, Liao G, Xu B (2021) Cadmium exposure induces osteoporosis through cellular senescence, associated with activation of NF-kappaB pathway and mitochondrial dysfunction. Environ Pollut 290:118043. https://doi.org/10.1016/j.envpol.2021.118043
Manolagas SC (2010) From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev 31:266–300. https://doi.org/10.1210/er.2009-0024
Mulligan AA, Hayhoe RPG, Luben RN, Welch AA (2021) Positive associations of dietary intake and plasma concentrations of vitamin e with skeletal muscle mass, heel bone ultrasound attenuation and Fracture Risk in the EPIC-Norfolk cohort. Antioxidants (Basel) 10:2. https://doi.org/10.3390/antiox10020159
Fujita K, Iwasaki M, Ochi H, Fukuda T, Ma C, Miyamoto T, Takitani K, Negishi-Koga T, Sunamura S, Kodama T, Takayanagi H, Tamai H, Kato S, Arai H, Shinomiya K, Itoh H, Okawa A, Takeda S (2012) Vitamin E decreases bone mass by stimulating osteoclast fusion. Nat Med 18:589–594. https://doi.org/10.1038/nm.2659
Muhammad N, Luke DA, Shuid AN, Mohamed N, Soelaiman IN (2012) Two different isomers of vitamin e prevent bone loss in postmenopausal osteoporosis rat model. Evid Based Complement Alternat Med 2:161527. https://doi.org/10.1155/2012/161527
Wolf RL, Cauley JA, Pettinger M, Jackson R, Lacroix A, Leboff MS, Lewis CE, Nevitt MC, Simon JA, Stone KL, Wactawski-Wende J (2005) Lack of a relation between vitamin and mineral antioxidants and bone mineral density: results from the Women’s Health Initiative. Am J Clin Nutr 82:581–588. https://doi.org/10.1093/ajcn.82.3.581
Ahmad NS, Khalid BA, Luke DA, Ima Nirwana S (2005) Tocotrienol offers better protection than tocopherol from free radical-induced damage of rat bone. Clin Exp Pharmacol Physiol 32:761–770. https://doi.org/10.1111/j.1440-1681.2005.04264.x
Kim DE, Cho SH, Park HM, Chang YK (2016) Relationship between bone mineral density and dietary intake of beta-carotene, vitamin C, zinc and vegetables in postmenopausal Korean women: a cross-sectional study. J Int Med Res 44:1103–1114. https://doi.org/10.1177/0300060516662402
Zhang J, Hu X, Zhang J (2017) Associations between serum vitamin E concentration and bone mineral density in the US elderly population. Osteoporos Int 28:1245–1253. https://doi.org/10.1007/s00198-016-3855-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Li, R., Qu, H., Xu, J. et al. Association between dietary intake of α-tocopherol and cadmium related osteoporosis in population ≥ 50 years. J Bone Miner Metab 41, 501–511 (2023). https://doi.org/10.1007/s00774-023-01418-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01418-x