Abstract
Background
Hyperselective neurectomy is a reliable treatment for spasticity. This research was designed to quantify the surgical parameters of hyperselective neurectomy of thoracodorsal nerve for shoulder spasticity through anatomical studies, as well as to retrospectively assess patients who underwent this procedure to provide an objective basis for clinical practice.
Methods
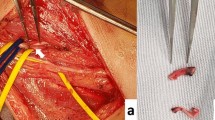
On nine embalmed adult cadavers (18 shoulders), we dissected and observed the branching patterns of thoracodorsal nerve, counted the number of nerve branches, measured the distribution of branch origin point, and determined the length of the surgical incision. Next, we selected five patients who underwent this procedure for shoulder spasticity and retrospectively evaluated (ethic committee: 2022–37) their shoulder function with active/passive range of motion (AROM/PROM) and modified Ashworth scale (MAS).
Results
The anatomical study revealed that the main trunk of thoracodorsal nerve sends out one to three medial branches, with the pattern of only one medial branch being the most common (61.1%); there were significant variations in the branch numbers and nerve distributions; the location of thoracodorsal nerve branches’ entry points into the muscle varied from 27.2 to 67.8% of the length of the arm. Clinical follow-up data showed significant improvement in shoulder mobility in all patients. AROM of shoulder abduction increased by 39.4° and PROM increased by 64.2° (P < 0.05). AROM and PROM of shoulder flexion increased by 36.6° and 54.4°, respectively (P < 0.05). In addition, the MAS of shoulder abduction (1.8) and flexion (1.2) was both significantly reduced in all patients (P < 0.05).
Conclusion
Hyperselective neurectomy of thoracodorsal nerve is effective and stable in the treatment of shoulder spasticity. Intraoperative attention is required to the numbers of the medial branch of thoracodorsal nerve. We recommend an incision in the mid-axillary line that extends from 25 to 70% of the arm length to fully expose each branch.


Similar content being viewed by others
Data availability
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author.
Abbreviations
- AROM:
-
Active range of motion
- PROM:
-
Passive range of motion
- MAS:
-
Modified Ashworth scale
- HSN:
-
Hyperselective neurectomy
References
Bini N, Leclercq C (2020) Anatomical study of the deep branch of the ulnar nerve and application to selective neurectomy in the treatment of spasticity of the first web space. Surg Radiol Anat 42:253–258
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67:206–207
Brunelli G, Brunelli F (1983) Partial selective denervation in spastic palsies (hyponeurotization). Microsurgery 4:221–224
Buffenoir K, Rigoard P, Ferrand-Sorbets S, Lapierre F (2009) Retrospective study of the long-term results of selective peripheral neurotomy for the treatment of spastic upper limb. Neurochirurgie 55(Suppl 1):S150–S160
Buffenoir K, Decq P, Hamel O, Lambertz D, Perot C (2013) Long-term neuromechanical results of selective tibial neurotomy in patients with spastic equinus foot. Acta Neurochir (Wien) 155:1731–1743
Cambon-Binder A, Leclercq C (2015) Anatomical study of the musculocutaneous nerve branching pattern: application for selective neurectomy in the treatment of elbow flexors spasticity. Surg Radiol Anat 37:341–348
Decq P, Filipetti P, Feve A, Djindjian M, Saraoui A, Kéravel Y (1997) Peripheral selective neurotomy of the brachial plexus collateral branches for treatment of the spastic shoulder: anatomical study and clinical results in five patients. J Neurosurg 86:648–653
Delgado MR, Tilton A, Carranza-Del Río J, Dursun N, Bonikowski M, Aydin R, Maciag-Tymecka I, Oleszek J, Dabrowski E, Grandoulier A, Picaut P (2021) Efficacy and safety of abobotulinumtoxin A for upper limb spasticity in children with cerebral palsy: a randomized repeat-treatment study. Dev Med Child Neurol 63:592–600
Garland DE, Thompson R, Waters RL (1980) Musculocutaneous neurectomy for spastic elbow flexion in non-functional upper extremities in adults. J Bone Joint Surg Am 62:108–112
Gracies J, Brashear A, Jech R, McAllister P, Banach M, Valkovic P, Walker H, Marciniak C, Deltombe T, Skoromets A, Khatkova S, Edgley S, Gul F, Catus F, De Fer BB, Vilain C, Picaut P (2015) Safety and efficacy of abobotulinumtoxin A for hemiparesis in adults with upper limb spasticity after stroke or traumatic brain injury: a double-blind randomised controlled trial. Lancet Neurol 14:992–1001
Gras M, Leclercq C (2017) Spasticity and hyperselective neurectomy in the upper limb. Hand Surg Rehabil 36:391–401
Helin M, Bachy M, Stanchina C, Fitoussi F (2018) Pronator teres selective neurectomy in children with cerebral palsy. J Hand Surg Eur 43:879–884
Iwanaga J, Singh V, Ohtsuka A, Hwang Y, Kim H, Moryś J, Ravi KS, Ribatti D, Trainor PA, Sañudo JR, Apaydin N, Şengül G, Albertine KH, Walocha JA, Loukas M, Duparc F, Paulsen F, Del Sol M, Adds P, Hegazy A, Tubbs RS (2021) Acknowledging the use of human cadaveric tissues in research papers: recommendations from anatomical journal editors. Clin Anat 34:2–4
Iwanaga J, Singh V, Takeda S, Ogeng’O J, Kim H, Moryś J, Ravi KS, Ribatti D, Trainor PA, Sañudo JR, Apaydin N, Sharma A, Smith HF, Walocha JA, Hegazy AMS, Duparc F, Paulsen F, Del Sol M, Adds P, Louryan S, Fazan VPS, Boddeti RK, Tubbs RS (2022) Standardized statement for the ethical use of human cadaveric tissues in anatomy research papers: recommendations from Anatomical Journal Editors-in-Chief. Clin Anat 35:526–528
Koman LA, Smith BP, Shilt JS (2004) Cerebral palsy. Lancet 363:1619–1631
Koman LA, Smith BP, Williams R, Richardson R, Naughton M, Griffin L, Evans P (2013) Upper extremity spasticity in children with cerebral palsy: a randomized, double-blind, placebo-controlled study of the short-term outcomes of treatment with botulinum A toxin. J Hand Surg Am 38:435–446
Kong KH, Chua KS (1999) Neurolysis of the musculocutaneous nerve with alcohol to treat poststroke elbow flexor spasticity. Arch Phys Med Rehabil 80:1234–1236
Kwakkel G, Meskers CGM (2015) Botulinum toxin A for upper limb spasticity. Lancet Neurol 14:969–971
Leclercq C (2003) General assessment of the upper limb. Hand Clin 19:557–564
Leclercq C (2018) Selective neurectomy for the spastic upper extremity. Hand Clin 34:537–545
Lee K (2007) Variation of the spinal nerve compositions of thoracodorsal nerve. Clin Anat 20:660–662
Lee H, Chen JJ, Wu Y, Wang Y, Huang S, Piotrkiewicz M (2008) Time course analysis of the effects of botulinum toxin type a on elbow spasticity based on biomechanic and electromyographic parameters. Arch Phys Med Rehabil 89:692–699
Lu W, Xu J, Wang D, Gu Y (2008) Microanatomical study on the functional origin and direction of the thoracodorsal nerve from the trunks of brachial plexus. Clin Anat 21:509–513
Maarrawi J, Mertens P, Luaute J, Vial C, Chardonnet N, Cosson M, Sindou M (2006) Long-term functional results of selective peripheral neurotomy for the treatment of spastic upper limb: prospective study in 31 patients. J Neurosurg 104:215–225
Msaddi AK, Mazroue AR, Shahwan S, Al Amri N, Dubayan N, Livingston D, Moutaery KR (1997) Microsurgical selective peripheral neurotomy in the treatment of spasticity in cerebral-palsy children. Stereotact Funct Neurosurg 69:251–258
Paolini G, Longo B, Laporta R, Sorotos M, Amoroso M, Santanelli F (2013) Permanent latissimus dorsi muscle denervation in breast reconstruction. Ann Plast Surg 71:639–642
Parot C, Leclercq C (2016) Anatomical study of the motor branches of the median nerve to the forearm and guidelines for selective neurectomy. Surg Radiol Anat 38:597–604
Paulos R, Leclercq C (2015) Motor branches of the ulnar nerve to the forearm: an anatomical study and guidelines for selective neurectomy. Surg Radiol Anat 37:1043–1048
Pecak F, Trontelj JV, Dimitrijevic MR (1980) Scoliosis in neuromuscular disorders. Int Orthop 3:323–328
Penn RD, Kroin JS (1985) Continuous intrathecal baclofen for severe spasticity. Lancet 2:125–127
Purohit AK, Raju BS, Kumar KS, Mallikarjun KD (1998) Selective musculocutaneous fasciculotomy for spastic elbow in cerebral palsy: a preliminary study. Acta Neurochir (Wien) 140:473–478
Rousseaux M, Buisset N, Daveluy W, Kozlowski O, Blond S (2009) Long-term effect of tibial nerve neurotomy in stroke patients with lower limb spasticity. J Neurol Sci 278:71–76
Sindou MP, Simon F, Mertens P, Decq P (2007) Selective peripheral neurotomy (SPN) for spasticity in childhood. Childs Nerv Syst 23:957–970
Sitthinamsuwan B, Chanvanitkulchai K, Phonwijit L, Nunta-Aree S, Kumthornthip W, Ploypetch T (2013) Surgical outcomes of microsurgical selective peripheral neurotomy for intractable limb spasticity. Stereotact Funct Neurosurg 91:248–257
Stoffel A (1913) The treatment of spastic contractures. Am J Orthop Surg 10:611–644
Waxweiler C, Remy S, Merlini L, Leclercq C (2022) Nerve transfer in the spastic upper limb: anatomical feasibility study. Surg Radiol Anat 44:183–190
Yu A, Shen Y, Qiu Y, Jiang S, Yu Y, Yin H, Xu W (2020) Hyperselective neurectomy in the treatment of elbow and wrist spasticity: an anatomical study and incision design. Br J Neurosurg 9:1–6
Zhao J, Zhao Q, Liu Z, Deng S, Cheng L, Zhu W, Zhang R, Ma R, Yan H, Li Q (2020) The anatomical mechanism of C5 palsy after expansive open-door laminoplasty. Spine J 20:1776–1784
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude [3]. The authors thank all the participants and researchers who participated in this study.
Funding
This work was supported by the National Natural Science Foundation of China under Grants 81830063, 81801363, 81873766, and 82021002; CAMS Innovation Fund for Medical Sciences under Grant 2019-I2M-5–007; Special Project of Clinical and Translational Medicine Research Cultivating Program under Grant 2021-I2M-C&T-B-100; Program of Shanghai Municipal Commission of Health and Family Planning under Grant 20184Y0111; Shanghai Municipal Clinical Medical Center Project under Grant 2017ZZ01006; and Shanghai Municipal Key Clinical Specialty under Grant shslczdzk05601.
Author information
Authors and Affiliations
Contributions
Each author made substantial contributions to this work. Weishan Lin and Yundong Shen contributed to the conception and design of the work. Weishan Lin and Tie Li contributed to the acquisition of the study data. Weishan Lin and Tie Li contributed to the analysis and interpretation of the data. Wendong Xu, Yundong Shen, and Weishan Lin contributed to the surgical technical support. Weishan Lin and Tie Li contributed to the drafting of the manuscript. Wendong Xu, Yundong Shen, and Wenjun Qi contributed to the revision of the manuscript. All authors approved the submitted version. Weishan Lin and Tie Li contributed equally to this work.
Corresponding author
Ethics declarations
Ethics approval
The procedures used in this study adhere to the tenets of the Declaration of Helsinki. The studies involving human participants were reviewed and approved by the ethics committee of Jing’an District Central Hospital (Jing’an Branch of Huashan Hospital) (Approved No. of ethic committee: 2022–37). Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Conflict of interest
The authors declare no competing interests.
Additional information
Comments
Hyperselective neurectomy (HSN) for the treatment of spasticity is adequately proved by Leclercq et al. to be the effected choice of treatment for shoulder spasticity in order to improve passive and active range of movement. This study confirms with further five operated cases the efficacy of HSN. It also contributes with anatomical study of thoracodorsal nerve branches and measurements to orient the surgeon intraoperatively.
Ridvan Alimehmeti.
Tirana, Albania.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, W., Li, T., Qi, W. et al. Hyperselective neurectomy of thoracodorsal nerve for treatment of the shoulder spasticity: anatomical study and preliminary clinical results. Acta Neurochir 165, 1179–1188 (2023). https://doi.org/10.1007/s00701-023-05553-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05553-2