Abstract
Purpose
Adjacent segment disease (ASD) requiring revision surgery is the most serious complication that can occur in patients undergoing posterior lumbar interbody fusion (PLIF) surgery. This study aimed to determine the risk factors for surgical ASD requiring revision surgery after PLIF with screw fixation surgery. We especially focused on paraspinal muscle, facet joint, and disc degeneration.
Methods
Among the patients who underwent PLIF with screw fixation due to degenerative spinal disease from January 2010 to December 2019, patients who underwent revision surgery for the development of ASD were enrolled. To evaluate the risk factors for surgical ASD, we selected a control group. Each patient in the control group was matched by age, sex, fusion level, number of fused segments, secondary MRI follow-up interval, and follow-up duration with a patient in the surgical ASD group. The radiographic and demographic data were compared between the surgical ASD and control groups.
Results
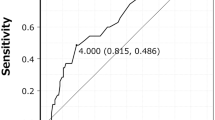
There were statistically significant differences between the two groups in radiological parameters of preoperative facet degeneration, facet effusion, facet angle, and fatty degeneration of the multifidus muscle. Multivariable logistic regression analysis revealed that preoperative facet effusion (odds ratio [OR] 6.48), preoperative facet angle (OR 1.24), and progression of fatty degeneration in the multifidus muscle (OR 1.07) were significant risk factors for surgical ASD.
Conclusions
Preexisting high-grade adjacent facet effusion, sagittally oriented facet joint angle, and progressive fatty degeneration of the multifidus muscle are associated with the development of surgical ASD after PLIF surgery.




Similar content being viewed by others
References
Alentado VJ, Lubelski D, Healy AT, Orr RD, Steinmetz MP, Benzel EC, Mroz TE (2016) Predisposing characteristics of adjacent segment disease after lumbar fusion. Spine (Phila Pa 1976) 41:1167–1172. doi:https://doi.org/10.1097/BRS.0000000000001493
Anandjiwala J, Seo JY, Ha KY, Oh IS, Shin DC (2011) Adjacent segment degeneration after instrumented posterolateral lumbar fusion: a prospective cohort study with a minimum five-year follow-up. Eur Spine J 20:1951–1960. https://doi.org/10.1007/s00586-011-1917-0
Anderson PA, Andersson GB, Arnold PM, Brodke DS, Brodt ED, Chapman JR, Chou D, Dekutoski M, Dettori JR, DeVine JG, Ely CG, Fehlings MG, Fischer DJ, Fourney DR, Hansen MA, Harrod CC, Hashimoto R, Hermsmeyer JT, Hilibrand AS, Kasliwal MK, Kelly MP, Kim HJ, Kraemer P, Lawrence BD, Lee MJ, Lenke LG, Norvell DC, Raich A, Riew KD, Shaffrey CI, Skelly AC, Smith JS, Standaert CJ, Van Alstyne EM, Wang JC (2012) Terminology. Spine (Phila Pa 1976) 37:S8–9. doi:https://doi.org/10.1097/BRS.0b013e31826d62ed
Bastian L, Lange U, Knop C, Tusch G, Blauth M (2001) Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J 10:295–300. https://doi.org/10.1007/s005860100278
Chang MY, Park Y, Ha JW, Zhang HY, Lee SH, Hong TH, Lee SH (2019) Paraspinal lean muscle mass measurement using spine MRI as a predictor of adjacent segment disease after lumbar fusion: a propensity score-matched case-control analysis. AJR Am J Roentgenol:1–8. doi:https://doi.org/10.2214/AJR.18.20441
Chaput C, Padon D, Rush J, Lenehan E, Rahm M (2007) The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine (Phila Pa 1976) 32:1883–1887. doi:https://doi.org/10.1097/BRS.0b013e318113271a
Cho BY, Murovic JA, Park J (2009) Imaging correlation of the degree of degenerative L4–5 spondylolisthesis with the corresponding amount of facet fluid. J Neurosurg Spine 11:614–619. https://doi.org/10.3171/2009.6.SPINE08413
Cho KS, Kang SG, Yoo DS, Huh PW, Kim DS, Lee SB (2009) Risk factors and surgical treatment for symptomatic adjacent segment degeneration after lumbar spine fusion. J Korean Neurosurg Soc 46:425–430. https://doi.org/10.3340/jkns.2009.46.5.425
Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL (1994) Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976) 19:1745–1751. doi:https://doi.org/10.1097/00007632-199408000-00015
Di Martino A, Quattrocchi CC, Scarciolla L, Papapietro N, Beomonte Zobel B, Denaro V (2014) Estimating the risk for symptomatic adjacent segment degeneration after lumbar fusion: analysis from a cohort of patients undergoing revision surgery. Eur Spine J 23(Suppl 6):693–698. https://doi.org/10.1007/s00586-014-3551-0
Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X (2010) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19:316–324. https://doi.org/10.1007/s00586-009-1191-6
Fortin M, Battie MC (2012) Quantitative paraspinal muscle measurements: inter-software reliability and agreement using OsiriX and ImageJ. Phys Ther 92:853–864. https://doi.org/10.2522/ptj.20110380
Grobler LJ, Robertson PA, Novotny JE, Pope MH (1993) Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine (Phila Pa 1976) 18:80–91
Ha KY, Schendel MJ, Lewis JL, Ogilvie JW (1993) Effect of immobilization and configuration on lumbar adjacent-segment biomechanics. J Spinal Disord 6:99–105
Helgeson MD, Bevevino AJ, Hilibrand AS (2013) Update on the evidence for adjacent segment degeneration and disease. Spine J 13:342–351. https://doi.org/10.1016/j.spinee.2012.12.009
Hides JA, Richardson CA, Jull GA (1996) Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine (Phila Pa 1976) 21:2763–2769. doi:https://doi.org/10.1097/00007632-199612010-00011
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190S-194S. https://doi.org/10.1016/j.spinee.2004.07.007
Hyun SJ, Kim YB, Kim YS, Park SW, Nam TK, Hong HJ, Kwon JT (2007) Postoperative changes in paraspinal muscle volume: comparison between paramedian interfascial and midline approaches for lumbar fusion. J Korean Med Sci 22:646–651. https://doi.org/10.3346/jkms.2007.22.4.646
Kamaz M, Kiresi D, Oguz H, Emlik D, Levendoglu F (2007) CT measurement of trunk muscle areas in patients with chronic low back pain. Diagn Interv Radiol 13:144–148
Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, Kim KH, Park JY, Chin DK, Kim KS, Cho YE, Kuh SU (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16:867–875. https://doi.org/10.1016/j.spinee.2016.03.010
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10:314–319. https://doi.org/10.1007/s005860000239
Lattig F, Fekete TF, Grob D, Kleinstuck FS, Jeszenszky D, Mannion AF (2012) Lumbar facet joint effusion in MRI: a sign of instability in degenerative spondylolisthesis? Eur Spine J 21:276–281. https://doi.org/10.1007/s00586-011-1993-1
Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, Lee MY (2009) Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J 18:1637–1643. https://doi.org/10.1007/s00586-009-1060-3
Lee JC, Kim Y, Soh JW, Shin BJ (2014) Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion: comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine (Phila Pa 1976) 39:E339–345. doi:https://doi.org/10.1097/BRS.0000000000000164
Liang J, Dong Y, Zhao H (2014) Risk factors for predicting symptomatic adjacent segment degeneration requiring surgery in patients after posterior lumbar fusion. J Orthop Surg Res 9:97. https://doi.org/10.1186/s13018-014-0097-0
Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Takahashi Y, Iwasaki M (2018) Adjacent segment disease after single segment posterior lumbar interbody fusion for degenerative spondylolisthesis: minimum 10 years follow-up. Spine (Phila Pa 1976) 43:E1384-E1388. doi:https://doi.org/10.1097/BRS.0000000000002710
Okuda S, Yamashita T, Matsumoto T, Nagamoto Y, Sugiura T, Takahashi Y, Maeno T, Iwasaki M (2018) Adjacent segment disease after posterior lumbar interbody fusion: a case series of 1000 patients. Global Spine J 8:722–727. https://doi.org/10.1177/2192568218766488
Ou CY, Lee TC, Lee TH, Huang YH (2015) Impact of body mass index on adjacent segment disease after lumbar fusion for degenerative spine disease. Neurosurgery 76:396–401; discussion 401–392; quiz 402. doi:https://doi.org/10.1227/NEU.0000000000000627
Panjabi MM (1992) The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 5:390–396; discussion 397. doi:https://doi.org/10.1097/00002517-199212000-00002
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. doi:https://doi.org/10.1097/01.brs.0000137069.88904.03
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878. doi:https://doi.org/10.1097/00007632-200109010-00011
Rihn JA, Lee JY, Khan M, Ulibarri JA, Tannoury C, Donaldson WF, 3rd, Kang JD (2007) Does lumbar facet fluid detected on magnetic resonance imaging correlate with radiographic instability in patients with degenerative lumbar disease? Spine (Phila Pa 1976) 32:1555–1560. doi:https://doi.org/10.1097/BRS.0b013e318067dc55
Rothenfluh DA, Mueller DA, Rothenfluh E, Min K (2015) Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 24:1251–1258. https://doi.org/10.1007/s00586-014-3454-0
Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11:11–20. https://doi.org/10.1016/j.spinee.2010.09.026
Stokes IA, Gardner-Morse M (1995) Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine (Phila Pa 1976) 20:2168–2169
Tamai K, Kato M, Konishi S, Matsumura A, Hayashi K, Nakamura H (2017) Facet effusion without radiographic instability has no effect on the outcome of minimally invasive decompression surgery. Global Spine J 7:21–27. https://doi.org/10.1055/s-0036-1583173
Throckmorton TW, Hilibrand AS, Mencio GA, Hodge A, Spengler DM (2003) The impact of adjacent level disc degeneration on health status outcomes following lumbar fusion. Spine (Phila Pa 1976) 28:2546–2550. doi:https://doi.org/10.1097/01.BRS.0000092340.24070.F3
Wang G, Karki SB, Xu S, Hu Z, Chen J, Zhou Z, Fan S (2015) Quantitative MRI and X-ray analysis of disc degeneration and paraspinal muscle changes in degenerative spondylolisthesis. J Back Musculoskelet Rehabil 28:277–285. https://doi.org/10.3233/BMR-140515
Wang H, Ma L, Yang D, Wang T, Liu S, Yang S, Ding W (2017) Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine (Baltimore) 96:e6032. https://doi.org/10.1097/MD.0000000000006032
Weinstein JN, Boden SD, An H (2003) Emerging technology in spine: should we rethink the past or move forward in spite of the past? Spine (Phila Pa 1976) 28:S1. doi:https://doi.org/10.1097/01.BRS.0000076840.37272.11
Weishaupt D, Zanetti M, Boos N, Hodler J (1999) MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol 28:215–219. https://doi.org/10.1007/s002560050503
Yamasaki K, Hoshino M, Omori K, Igarashi H, Nemoto Y, Tsuruta T, Matsumoto K, Iriuchishima T, Ajiro Y, Matsuzaki H (2017) Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 42:E86-E92. doi:https://doi.org/10.1097/BRS.0000000000001728
Zheng G, Wang C, Wang T, Hu W, Ji Q, Hu F, Li J, Chaudhary SK, Song K, Song D, Zhang Z, Hao Y, Wang Y, Li J, Zheng Q, Zhang X, Wang Y (2020) Relationship between postoperative lordosis distribution index and adjacent segment disease following L4–S1 posterior lumbar interbody fusion. J Orthop Surg Res 15:129. https://doi.org/10.1186/s13018-020-01630-9
Funding
This work was supported by the 2021 Yeungnam University Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standard. For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Rights and permissions
About this article
Cite this article
Yun, Y.I., Jeon, I., Kim, S.W. et al. Risk factors for adjacent segment disease requiring reoperation after posterior lumbar interbody fusion with screw fixation: focus on paraspinal muscle, facet joint, and disc degeneration. Acta Neurochir 164, 913–922 (2022). https://doi.org/10.1007/s00701-021-05073-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-05073-x