Abstract
Background
The informed consent is a defining moment that should allow patients to understand their condition, what procedure they are undergoing, and what consequences may follow. This process should foster trust and promote confidence, without increasing patients’ anxiety. New immersive 3D imaging technologies may serve as a tool to facilitate this endeavor.
Methods
In a prospective, single-center, randomized controlled clinical trial (SPLICE Study: Surgical Planning and Informed Consent Study; ClinicalTrials.gov NCT03503487), 40 patients undergoing surgery for intracranial tumors were enrolled. After undergoing a traditional surgical informed consent acquisition, 33 patients were randomized 1:1:1 to 3 groups: in 2 experimental groups, patients underwent a 3D, immersive informed consent with two different surgical planners (group 1 and group 2); in the control group, patients underwent an informed consent supported by traditional 2D radiological images.
Results
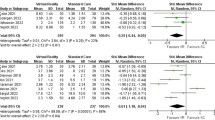
Patients in the experimental groups appreciated this communication experience, while their objective comprehension was higher ((score mean (SD)): group 1 82.65 (6.83); group 2 77.76 (10.19)), as compared with the control group (57.70 (12.49); P < 0.001). Subjective comprehension and anxiety levels did not differ between experimental groups and control group.
Conclusions
3D virtual reality can help surgeons and patients in building a better relationship before surgery; immersive 3D-supported informed consent improves patients’ comprehension of their condition without increasing anxiety. This new paradigm may foster trust between surgeons and patients, possibly restraining medical-legal acts.
Trail registration
ClinicalTrials.gov NCT03503487


Similar content being viewed by others
References
Alfonso F, Ibañez L, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. WNEU 75:709–715
AMA Code of Medical Ethics. https://www.ama-assn.org/delivering-care/informed-consent. Accessed 27 Jul 2018
Bernat JL, Peterson LM (2006) Patient-centered informed consent in surgical practice. Arch Surg 141(1):86–92
Braddock CH, Fihn SD, Levinson W, Jonsen AR, Pearlman RA (1997) How doctors and patients discuss routine clinical decisions: informed decision making in the outpatient setting. J Gen Intern Med 12(6):339–345
Cecchetto C, Di Domenico A, Garraffa M, Papagno C (2012) Comprendo. Batteria per la Comprensione di frasi negli adulti. Raffaele Cortina
Contreras López WO, Navarro PA, Crispin S (2019) Intraoperative clinical application of augmented reality in neurosurgery: a systematic review. Clin Neurol Neurosurg 177:6–11
Edwards WS, Yahne C (1987) Surgical informed consent: what it is and is not. Am J Surg 154(6):574–578
Epstein NE (2011) A review of edicallegal malpractice suits involving cervical spine. J Spinal Disord Tech 24(1):15–20
Flory J (2014) Interventions to improve research in informed consent for research. J Am Med Assoc 292(13):1593–1601
Hall DE, Prochazka AV, Fink AS (2012) Informed consent for clinical treatment. CMAJ. https://doi.org/10.1503/cmaj.112120
Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P (2002) Patient complaints and malpractice risk. JAMA 287(22):2951–2957
Jena AB, Seabury S, Lakdawalla D, Chandra A (2011) Malpractice risk according to physician specialty. N Engl J Med 365(7):629–636
Kerrigan DD, Thevasagayam RS, Woods TO, McWelch I, Thomas WE, Shorthouse AJ, Dennison AR (1993) Who’s afraid of informed consent? BMJ 306(6873):298–300
Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM (1997) Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA 277(7):553–559
Matiasek J, Wynia MK (2008) Reconceptualizing the informed consent process at eight innovative hospitals. Jt Comm J Qual Patient Saf 34(3):127–137
McKneally MF, Ignagni E, Martin DK, D’Cruz J (2004) The leap to trust: perspective of cholecystectomy patients on informed decision making and consent. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2004.02.021
McKneally MF, Martin DK (2000) An entrustment model of consent for surgical treatment of life-threatening illness: perspective of patients requiring esophagectomy. J Thorac Cardiovasc Surg. https://doi.org/10.1067/mtc.2000.106525
Mondini S, Mapelli D, Vestri A, Bisiacchi PS (2003) Esame neuropsicologico breve. Raffaello Cortina Editore
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Paasche-Orlow MK, Taylor HA, Brancati FL (2003) Readability standards for informed-consent forms as compared with actual readability. N Engl J Med 348(8):721–726
Perin A, DiMeco F (2015) Health literacy and pseudoliteracy in neurosurgery: the “C. Besta” experience. World Neurosurg 84(6):1541–1543
Rothberg MB, Sivalingam SK, Ashraf J, Visintainer P, Joelson J, Kleppel R, Vallurupalli N, Schweiger MJ (2010) Patients’ and cardiologists’ perceptions of the benefits of percutaneous coronary intervention for stable coronary disease. Ann Intern Med 153(5):307–313
Schenker Y, Meisel A (2011) Informed consent in clinical care. JAMA 305(11):1130–1131
Spielberger CD (2010) State-trait anxiety inventory. Wiley Online Library
Tait AR, Voepel-Lewis T (2015) Digital multimedia: a new approach for informed consent? Jama 313(5):463–464
Acknowledgments
We deeply thank Ms Nina Ravelli for her generous and continuous support to the Besta NeuroSim Center.
Funding
The study was partly funded by the European Commission through the FP7-Health Research Project TheraGlio (Grant Agreement ID: 602923); Dr Hagit Silberberg was paid by Surgical Theater while conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hagit Silberberg worked at Surgical Theater.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Electronic supplementary material
ESM 1
(MPG 25554 kb)
Rights and permissions
About this article
Cite this article
Perin, A., Galbiati, T.F., Ayadi, R. et al. Informed consent through 3D virtual reality: a randomized clinical trial. Acta Neurochir 163, 301–308 (2021). https://doi.org/10.1007/s00701-020-04303-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04303-y