Abstract
Purpose
Pediatric sedation is commonly required to obtain high-quality images in magnetic resonance imaging (MRI). We performed a systematic review and meta-analysis to assess the effects of dexmedetomidine sedation for MRI in children.
Methods
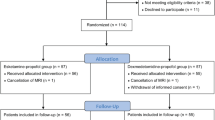
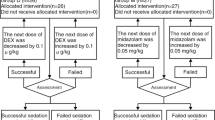
A systematic review was conducted to find all randomized controlled trials concerning dexmedetomidine sedation for MRI in children. We searched databases using the Ovid platform in the Cochrane Controlled Trials Register, MEDLINE, and EMBASE. This study was registered in the PROSPERO database: CRD42020198368.
Results
Seven studies and 753 participants were included. Dexmedetomidine sedation showed a significantly delayed onset time [weighted mean differences (WMD) = 8.13 min, 95% confidence interval (CI) 4.64 to 11.63, I2 = 98%] and recovery time (WMD = 5.22 min, 95% CI 0.35 to 10.09, I2 = 92%) compared to propofol, ketamine, and midazolam sedation. There was no difference in quality of sedation [risk ratio (RR) = 1.25, 95% CI 0.92 to 1.69, I2 = 89%], or incidence of sedation failure (RR = 1.39, 95% CI 0.53 to 3.66, I2 = 83%) between groups. Although a significantly decreased heart rate (WMD = − 17.34 beats/minute, 95% CI − 22.42 to − 12.26, I2 = 96%) was observed, bradycardia that required treatment was not increased (RR = 8.00, 95% CI 1.02 to 62.64, I2 = 0%). Dexmedetomidine sedation had a lower incidence of desaturation events (RR = 0.42, 95% CI 0.20 to 0.86, I2 = 4%). However, there was no difference in incidence of postoperative vomiting (RR = 0.42, 95% CI 0.15 to 1.17, I2 = 17%) between groups.
Conclusions
Dexmedetomidine sedation provided a similar sedation quality with a reduced incidence of desaturation events. However, the delayed onset and recovery times were drawbacks. The clinical significance of bradycardia is considered to be low. GRADE assessment revealed the quality of the evidence in this meta-analysis ranged from very low to moderate.




Similar content being viewed by others
References
Schulte-Uentrop L, Goepfert MS. Anaesthesia or sedation for MRI in children. Curr Opin Anaesthesiol. 2010;23(4):513–7.
Ahmad R, Hu HH, Krishnamurthy R, Krishnamurthy R. Reducing sedation for pediatric body MRI using accelerated and abbreviated imaging protocols. Pediatr Radiol. 2018;48(1):37–49.
Hallowell LM, Stewart SE, de Amorim ESCT, Ditchfield MR. Reviewing the process of preparing children for MRI. Pediatr Radiol. 2008;38(3):271–9.
Arthurs OJ, Sury M. Anaesthesia or sedation for paediatric MRI: advantages and disadvantages. Curr Opin Anaesthesiol. 2013;26(4):489–94.
Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90(3):699–705.
Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008;4(5):619–27.
Arain SR, Ebert TJ. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesthesia and Analgesia. 2002;95(2):461–6, table of contents.
Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans II hemodynamic changes. Anesthesiology. 1992;77(6):1134–42.
Zhou Q, Shen L, Zhang X, Li J, Tang Y. Dexmedetomidine versus propofol on the sedation of pediatric patients during magnetic resonance imaging (MRI) scanning: a meta-analysis of current studies. Oncotarget. 2017;8(60):102468–73.
Fang H, Yang L, Wang X, Zhu H. Clinical efficacy of dexmedetomidine versus propofol in children undergoing magnetic resonance imaging: a meta-analysis. Int J Clin Exp Med. 2015;8(8):11881–9.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. http://handbook.cochrane.org.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60.
Yang Z, Song G, Hu W, Dang X, Haijuan G, Yu J. Pharmacological analysis of dexmedetomidine hydrochloride in pediatric anesthesia during magnetic resonance imaging. Pakistan J Pharmac Sci. 2018;31(5(Special)):2209–14.
Kamal K, Asthana U, Bansal T, Dureja J, Ahlawat G, Kapoor S. Evaluation of efficacy of dexmedetomidine versus propofol for sedation in children undergoing magnetic resonance imaging. Saudi J Anaesth. 2017;11(2):163–8.
Eldeek AM, Elfawal SM, Allam MG. Sedation in children undergoing magnetic resonance imaging comparative study between dexmedetomidine and ketamine. Egyptian Journal of Anaesthesia. 2016;32(3):263–8.
Wu J, Mahmoud M, Schmitt M, Hossain M, Kurth D. Comparison of propofol and dexmedetomedine techniques in children undergoing magnetic resonance imaging. Paediatr Anaesth. 2014;24(8):813–8.
Tammam TF. Comparison of the efficacy of dexmedetomidine, ketamine, and a mixture of both for pediatric MRI sedation. Egyptian Journal of Anaesthesia. 2013;29(3):241–6.
Koroglu A, Teksan H, Sagir O, Yucel A, Toprak HI, Ersoy OM. A comparison of the sedative, hemodynamic, and respiratory effects of dexmedetomidine and propofol in children undergoing magnetic resonance imaging. Anesthesia & Analgesia. 2006;103(1):63–7, table of contents.
Koroglu A, Demirbilek S, Teksan H, Sagir O, But AK, Ersoy MO. Sedative, haemodynamic and respiratory effects of dexmedetomidine in children undergoing magnetic resonance imaging examination: preliminary results. Br J Anaesth. 2005;94(6):821–4.
Campbell K, Torres L, Stayer S. Anesthesia and sedation outside the operating room. Anesthesiol Clin. 2014;32(1):25–43.
Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet (London, England). 2006;367(9512):766–80.
Roback MG, Carlson DW, Babl FE, Kennedy RM. Update on pharmacological management of procedural sedation for children. Curr Opin Anaesthesiol. 2016;29(Suppl 1):S21-35.
Mason KP, Zurakowski D, Zgleszewski SE, Robson CD, Carrier M, Hickey PR, Dinardo JA. High dose dexmedetomidine as the sole sedative for pediatric MRI. Paediatr Anaesth. 2008;18(5):403–11.
Mason KP, Lönnqvist PA. Bradycardia in perspective-not all reductions in heart rate need immediate intervention. Paediatr Anaesth. 2015;25(1):44–51.
Mason KP, Zgleszewski SE, Prescilla R, Fontaine PJ, Zurakowski D. Hemodynamic effects of dexmedetomidine sedation for CT imaging studies. Paediatr Anaesth. 2008;18(5):393–402.
Srinivasan M, Turmelle M, Depalma LM, Mao J, Carlson DW. Procedural sedation for diagnostic imaging in children by pediatric hospitalists using propofol: analysis of the nature, frequency, and predictors of adverse events and interventions. J Pediatr. 2012;160(5):801-6.e1.
Mallory MD, Baxter AL, Yanosky DJ, Cravero JP. Emergency physician-administered propofol sedation: a report on 25,433 sedations from the pediatric sedation research consortium. Ann Emerg Med. 2011;57(5):462-8.e1.
Cravero JP, Beach ML, Blike GT, Gallagher SM, Hertzog JH. The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium. Anesth Analg. 2009;108(3):795–804.
Aghajanian GK, VanderMaelen CP. Alpha 2-adrenoceptor-mediated hyperpolarization of locus coeruleus neurons: intracellular studies in vivo. Science (New York, NY). 1982;215(4538):1394–6.
Hsu YW, Cortinez LI, Robertson KM, Keifer JC, Sum-Ping ST, Moretti EW, Young CC, Wright DR, Macleod DB, Somma J. Dexmedetomidine pharmacodynamics: part I: crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004;101(5):1066–76.
Sriganesh K, Saini J, Theerth K, Venkataramaiah S. Airway dimensions in children with neurological disabilities during dexmedetomidine and propofol sedation for magnetic resonance imaging study. Turkish J Anaesthesiol Reanimat. 2018;46(3):214–21.
Mahmoud M, Mason KP. Dexmedetomidine: review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br J Anaesth. 2015;115(2):171–82.
Whittington RA, Virág L. Dexmedetomidine-induced decreases in accumbal dopamine in the rat are partly mediated via the locus coeruleus. Anesth Analg. 2006;102(2):448–55.
Jin S, Liang DD, Chen C, Zhang M, Wang J. Dexmedetomidine prevent postoperative nausea and vomiting on patients during general anesthesia: A PRISMA-compliant meta analysis of randomized controlled trials. Medicine. 2017;96(1):e5770.
Massad IM, Mohsen WA, Basha AS, Al-Zaben KR, Al-Mustafa MM, Alghanem SM. A balanced anesthesia with dexmedetomidine decreases postoperative nausea and vomiting after laparoscopic surgery. Saudi Med J. 2009;30(12):1537–41.
Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135(11):982–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was not supported by external funding and the authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kim, J.Y., Kim, K.N., Kim, D.W. et al. Effects of dexmedetomidine sedation for magnetic resonance imaging in children: a systematic review and meta-analysis. J Anesth 35, 525–535 (2021). https://doi.org/10.1007/s00540-021-02946-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02946-4