Abstract
Background
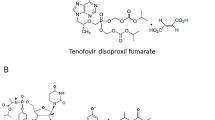
Entecavir and tenofovir–disoproxil–fumarate are first-line nucleos(t)ide analogs (NA) for treatment of hepatitis B virus (HBV) infections; however, their long-term administration can impact extrahepatic organs. Herein, we sought to examine the effect of NA on lipid metabolism while also characterizing the associated mechanism.
Methods
A retrospective study was performed on HBV patients administered entecavir or tenofovir–disoproxil–fumarate. Patient clinical information, as well as their preserved serum samples obtained at baseline and 6–12 months after treatment initiation, were analyzed. A 1:1 propensity score matching was applied to the assignment of tenofovir–disoproxil–fumarate or entecavir treatment. Changes in serum cholesterol, including oxidized-LDL, were analyzed. Subsequently, in vitro analysis elucidated the mechanism associated with the effect of NAs on lipid metabolism.
Results
Administration of tenofovir–disoproxil–fumarate, not entecavir, to chronic HBV patients, decreased serum cholesterol levels, including non-HDL and oxidized-LDL, which are strongly associated with arteriosclerosis. In vitro analysis revealed that tenofovir–disoproxil–fumarate reduced supernatant cholesterol, and upregulated the scavenger receptor, CD36, in hepatocytes. Meanwhile, silencing of hepatic CD36 increased supernatant cholesterol and negated the cholesterol-reducing effect of tenofovir–disoproxil–fumarate in HepG2-cells. Reporter, microarray, and RT-PCR analyses further revealed that tenofovir–disoproxil–fumarate treatment activates PPAR-α-mediated signaling, and upregulates PPAR-α target genes, including CPT1 and CD36. Alternatively, silencing of PPAR-α reversed the effects of tenofovir–disoproxil–fumarate on CD36.
Conclusions
Tenofovir–disoproxil–fumarate modulates lipid metabolism by upregulating hepatic CD36 via PPAR-α activation. Since dyslipidemia could be associated with arteriosclerosis and hepatocarcinogenesis, these discoveries provide novel insights into anti-HBV therapies, as well as the associated extrahepatic effects of NA.



Similar content being viewed by others
References
Trepo C, Chan HL, Lok A. Hepatitis B virus infection. Lancet. 2014;384:2053–63.
Lee WM. Hepatitis B virus infection. N Engl J Med. 1997;337:1733–45.
Walter SR, Thein HH, Gidding HF, et al. Risk factors for hepatocellular carcinoma in a cohort infected with hepatitis B or C. J Gastroenterol Hepatol. 2011;26:1757–64.
Mahoney FJ. Update on diagnosis, management, and prevention of hepatitis B virus infection. Clin Microbiol Rev. 1999;12:351–66.
Drafting Committee for Hepatitis Management G. the Japan Society of H.JSH Guidelines for the Management of Hepatitis B Virus Infection. Hepatol Res. 2014;44(Suppl S1):1–58.
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L.EASL. Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;2017(67):370–98.
Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–99.
Drafting Committee for Hepatitis Management Guidelines tJSoH.Japan Society of Hepatology Guidelines for the Management of Hepatitis B Virus Infection. update. Hepatol Res. 2019;2020(50):892–923.
Murata K, Asano M, Matsumoto A, et al. Induction of IFN-lambda3 as an additional effect of nucleotide, not nucleoside, analogues: a new potential target for HBV infection. Gut. 2018;67:362–71.
Wong GL, Chan HL, Tse YK, et al. Chronic kidney disease progression in patients with chronic hepatitis B on tenofovir, entecavir, or no treatment. Aliment Pharmacol Ther. 2018;48:984–92.
Suzuki K, Suda G, Yamamoto Y, et al. Entecavir treatment of hepatitis B virus-infected patients with severe renal impairment and those on hemodialysis. Hepatol Res. 2019;49:1294–304.
Charlton MR, Alam A, Shukla A, et al. An expert review on the use of tenofovir alafenamide for the treatment of chronic hepatitis B virus infection in Asia. J Gastroenterol. 2020;55:811–23.
Shaheen AA, AlMattooq M, Yazdanfar S, et al. Tenofovir disoproxil fumarate significantly decreases serum lipoprotein levels compared with entecavir nucleos(t)ide analogue therapy in chronic hepatitis B carriers. Aliment Pharmacol Ther. 2017;46:599–604.
Santos JR, Saumoy M, Curran A, et al. The lipid-lowering effect of tenofovir/emtricitabine: a randomized, crossover, double-blind, placebo-controlled trial. Clin Infect Dis. 2015;61:403–8.
Assmann G, Gotto AM. HDL cholesterol and protective factors in atherosclerosis. Circulation. 2004;109:III8-14.
Choi J, Kim HJ, Lee J, et al. Risk of hepatocellular carcinoma in patients treated with entecavir vs tenofovir for chronic hepatitis B: a Korean Nationwide Cohort Study. JAMA Oncol. 2019;5:30–6.
Yip TC, Wong VW, Chan HL, et al. Tenofovir is associated with lower risk of hepatocellular carcinoma than entecavir in patients with chronic HBV infection in China. Gastroenterology. 2020;158(215–25):e6.
Papatheodoridis GV, Sypsa V, Dalekos GN, et al. Hepatocellular carcinoma prediction beyond year 5 of oral therapy in a large cohort of Caucasian patients with chronic hepatitis B. J Hepatol. 2020;72:1088–96.
Su F, Berry K, Ioannou GN. (2020) No difference in hepatocellular carcinoma risk between chronic hepatitis B patients treated with entecavir versus tenofovir. Gut.
Dave S, Park S, Murad MH, et al. Comparative effectiveness of entecavir vs tenofovir for preventing hepatocellular carcinoma in patients with chronic hepatitis B: a systematic review and meta-analysis. Hepatology. 2020. https://doi.org/10.1002/hep.31267.
Yu MW, Lin CL, Liu CJ, et al. Influence of metabolic risk factors on risk of hepatocellular carcinoma and liver-related death in men with chronic hepatitis B: a large cohort study. Gastroenterology. 2017;153(1006–17):e5.
Ishigaki Y, Katagiri H, Gao J, et al. Impact of plasma oxidized low-density lipoprotein removal on atherosclerosis. Circulation. 2008;118:75–83.
Que X, Hung MY, Yeang C, et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018;558:301–6.
Suda G, Ogawa K, Yamamoto Y, et al. Retreatment with sofosbuvir, ledipasvir, and add-on ribavirin for patients who failed daclatasvir and asunaprevir combination therapy. J Gastroenterol. 2017;52(10):1122–9.
Suda G, Kurosaki M, Itakura J, et al. Safety and efficacy of elbasvir and grazoprevir in Japanese hemodialysis patients with genotype 1b hepatitis C virus infection. J Gastroenterol. 2018;54(1):78–86.
Suda G, Kudo M, Nagasaka A, et al. Efficacy and safety of daclatasvir and asunaprevir combination therapy in chronic hemodialysis patients with chronic hepatitis C. J Gastroenterol. 2016;51(7):733–40.
Suda G, Furusyo N, Toyoda H, et al. Daclatasvir and asunaprevir in hemodialysis patients with hepatitis C virus infection: a nationwide retrospective study in Japan. J Gastroenterol. 2018;53:119–28.
Suda G, Nagasaka A, Yamamoto Y, et al. Safety and efficacy of daclatasvir and asunaprevir in hepatitis C virus-infected patients with renal impairment. Hepatol Res. 2017;47:1127–36.
Sho T, Suda G, Nagasaka A, et al. Safety and efficacy of sofosbuvir and ribavirin for genotype 2 hepatitis C Japanese patients with renal dysfunction. Hepatol Res. 2018;48:529–38.
Kawagishi N, Suda G, Onozawa M, et al. Hepatitis B virus reactivation during hepatitis C direct-acting antiviral therapy in patients with previous HBV infection. J Hepatol. 2017;67:1106–8.
Mueller H, Lopez A, Tropberger P, et al. PAPD5/7 are host factors that are required for hepatitis B virus RNA stabilization. Hepatology. 2019;69:1398–411.
Okazaki M, Usui S, Ishigami M, et al. Identification of unique lipoprotein subclasses for visceral obesity by component analysis of cholesterol profile in high-performance liquid chromatography. Arterioscler Thromb Vasc Biol. 2005;25:578–84.
Tsukuda Y, Suda G, Tsunematsu S, et al. Anti-adipogenic and antiviral effects of l-carnitine on hepatitis C virus infection. J Med Virol. 2017;89:857–66.
Tsunematsu S, Suda G, Yamasaki K, et al. Hepatitis B virus X protein impairs alpha-interferon signaling via up-regulation of suppressor of cytokine signaling 3 and protein phosphatase 2A. J Med Virol. 2017;89:267–75.
Suda G, Kimura M, Shigesawa T, et al. Effects of resistance-associated variants in genotype 2 hepatitis C virus on viral replication and susceptibility to antihepatitis C virus drugs. Hepatol Res. 2019;49:1275–85.
Brown MS, Goldstein JL. The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell. 1997;89:331–40.
Zhou J, Febbraio M, Wada T, et al. Hepatic fatty acid transporter Cd36 is a common target of LXR, PXR, and PPARgamma in promoting steatosis. Gastroenterology. 2008;134:556–67.
Rakhshandehroo M, Knoch B, Muller M, et al. Peroxisome proliferator-activated receptor alpha target genes. PPAR Res. 2010;2010:612089.
Kinoshita M, Yokote K, Arai H, et al. Japan atherosclerosis society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J Atheroscler Thromb. 2018;25:846–984.
Packard CJ, Saito Y. Non-HDL cholesterol as a measure of atherosclerotic risk. J Atheroscler Thromb. 2004;11:6–14.
Steinberg D, Parthasarathy S, Carew TE, et al. Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med. 1989;320:915–24.
Ishigaki Y, Oka Y, Katagiri H. Circulating oxidized LDL: a biomarker and a pathogenic factor. Curr Opin Lipidol. 2009;20:363–9.
Delaney JA, Scherzer R, Biggs ML, et al. Associations of antiretroviral drug use and HIV-specific risk factors with carotid intima-media thickness. AIDS. 2010;24:2201–9.
Chen R, Scherzer R, Hsue PY, et al. Association of Tenofovir Use With Risk of Incident Heart Failure in HIV-Infected Patients. J Am Heart Assoc. 2017;2017:6.
Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2:re3.
Koonen DP, Jacobs RL, Febbraio M, et al. Increased hepatic CD36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes. 2007;56:2863–71.
Luangrath V, Brodeur MR, Rhainds D, et al. Mouse CD36 has opposite effects on LDL and oxidized LDL metabolism in vivo. Arterioscler Thromb Vasc Biol. 2008;28:1290–5.
Brundert M, Heeren J, Merkel M, et al. Scavenger receptor CD36 mediates uptake of high density lipoproteins in mice and by cultured cells. J Lipid Res. 2011;52:745–58.
Garbacz WG, Lu P, Miller TM, et al. Hepatic overexpression of CD36 improves glycogen homeostasis and attenuates high-fat diet-induced hepatic steatosis and insulin resistance. Mol Cell Biol. 2016;36:2715–27.
Takei K, Han SI, Murayama Y, et al. Selective peroxisome proliferator-activated receptor-alpha modulator K-877 efficiently activates the peroxisome proliferator-activated receptor-alpha pathway and improves lipid metabolism in mice. J Diabetes Investig. 2017;8:446–52.
Honda Y, Kessoku T, Ogawa Y, et al. Pemafibrate, a novel selective peroxisome proliferator-activated receptor alpha modulator, improves the pathogenesis in a rodent model of nonalcoholic steatohepatitis. Sci Rep. 2017;7:42477.
Acknowledgements
The authors thank all patients and their families and the investigators and staff of the participating institutions, NORTE Study Group a. The principal investigators of the NORTE study sites are listed below: Tomofumi Takagi (JCHO Sapporo Hokushin Hospital), Atsushi Nagasaka (Sapporo City General Hospital), Akira Fuzinaga (Abashiri-Kosei General Hospital), Hideaki Kikuchi, (Obihiro-Kosei General Hospital), Ken Furuya (JCHO Hokkaido Hospital), Takashi katou (National Hospital Organization Hokkaido Medical Center), Takashi Meguro (Hokkaido Gastroenterology Hospital), Akiyoshi Saga (Kaisei Hospital), Munenori Okamoto (Aiiku Hospital), Masaki Katagiri (Sapporo Hokuyu Hospital), Takuto Miyagishima (Kushiro Rosai Hospital), Jun Konno (Hakodate Central General Hospital), Kenichi Kumagai (Mori city National Health Insurance Hospital), Manabu Onodera (NTT EAST Sapporo Hospital), Tomoe Kobayashi (Tomakomai City Hospital), Minoru Uebayashi (Japanese Red Cross Kitami Hospital), Kanji Katou (Iwamizawa Municipal General Hospital), Yasuyuki Kunieda (Wakkanai City Hospital), Miki Tateyama (Tomakomai Nissho Hospital), Atsuhiko Kawakami (Sapporo Century Hospital), Izumi Tsunematsu (Touei hospital), Keisuke Shinada (Keiwakai Ebetsu Hospital) and Yoshiya Yamamoto (Hakodate Municipal Hospital). We would also like to thank Dr. Koichi Watashi and Dr. Takaji Wakita for generously providing the Hep2.2.15 cells.
Funding
This study was supported in part by Grants from the Japan Agency for Medical Research and Development (AMED; Grant Numbers JP20fk0210072, JP20fk0210064, JP20fk0210056, JP20fk0310101, JP20fk0210047, JP20fk0210048, JP20fk0210058, JP20fk0210066, JP20fk0210067) and SPS KAKENHI (Grant No. 19K08458).
Author information
Authors and Affiliations
Consortia
Contributions
KS and GS contributed equally to this work. KS and GS designed this study, performed the statistical analyses, and wrote the manuscript. YY, KF, MB, AN HM, MK,TK, KY, AN MO, NK, MN, TS, MN, KM, KO, and SO, collected the data KS, GS, MK, KY, conducted in vitro experiments. AN, HK, MN, KM, KO, and NS provided hepatological advice and edited the manuscript. MN, SO and NS revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Professor Naoya Sakamoto received lecture fees from Bristol Myers Squibb and Pharmaceutical K.K, grants and endowments from MSD K.K and Chugai Pharmaceutical Co., Ltd, and a research grant from Gilead Sciences, Inc. Dr. Goki Suda received research grants from Bristol Myers Squibb, MSD K.K, and Gilead Sciences. The other authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Suzuki, K., Suda, G., Yamamoto, Y. et al. Tenofovir–disoproxil–fumarate modulates lipid metabolism via hepatic CD36/PPAR-alpha activation in hepatitis B virus infection. J Gastroenterol 56, 168–180 (2021). https://doi.org/10.1007/s00535-020-01750-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-020-01750-3