Abstract
Purpose
Taste changes and vulnerability are commonly co-occurring in oncology patients undergoing chemotherapy. However, few studies explored the association and the inter-individual variability of these two conditions. This study aimed to identify heterogeneous subtypes of vulnerability and taste changes in older cancer patients undergoing chemotherapy, and explore individuals' characteristics and risk factors.
Methods
In this cross-sectional study, the latent class analysis (LCA) was conducted to identify the heterogeneous subgroups of patients with distinct vulnerability and taste change profiles. Differences in sociodemographic and clinical characteristics among the subpopulation were evaluated using parametric and nonparametric tests. Multinomial logistic regression was performed to investigate predictors of taste change-vulnerability subgroup classification.
Results
Three subgroups of those older cancer survivors were identified from the LCA: Class 1 (27.5%)-“Moderate taste change and low vulnerability”, Class 2 (29.0%)-“Low taste change and moderate vulnerability”, Class 3 (43.5%)-“High taste change and high vulnerability”. 98.9% of Class 3 reported taste changes and 54.0% reported vulnerability. Results from multinomial logistic regression indicated that patients in Class 3 were more likely to report experiencing mouth dryness and high blood pressure, and have received more than 3 cycles of chemotherapy.
Conclusion
The findings could provide new insights into the association between taste changes and vulnerability in older cancer adults receiving chemotherapy. Identifying different latent classes of taste changes and vulnerability would be helpful for developing interventions tailored to the heterogeneous survivors.

Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Pallis AG, Wedding U, Lacombe D, Soubeyran P, Wildiers H (2010) Questionnaires and instruments for a multidimensional assessment of the older cancer patient: what clinicians need to know? Eur J Cancer 46:1019–1025
Lin Y, Docherty SL, Porter LS, Bailey DE Jr (2020) Symptom experience and self-management for multiple co-occurring symptoms in patients with gastric cancer: A qualitative study. Eur J Oncol Nurs 49:101860
Joseph PV, Nolden A, Kober KM, Paul SM, Cooper BA, Conley YP, Hammer MJ, Wright F, Levine JD, Miaskowski C (2021) Fatigue, stress, and functional status are associated with taste changes in oncology patients receiving chemotherapy. J Pain Symptom Manage 62:373-382.e372
Ness KK, Wogksch MD (2020) Frailty and aging in cancer survivors. Transl Res 221:65–82
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-156
Mohile SG, Xian Y, Dale W, Fisher SG, Rodin M, Morrow GR, Neugut A, Hall W (2009) Association of a cancer diagnosis with vulnerability and frailty in older Medicare beneficiaries. J Natl Cancer Inst 101:1206–1215
Mohile SG, Bylow K, Dale W, Dignam J, Martin K, Petrylak DP, Stadler WM, Rodin M (2007) A pilot study of the vulnerable elders survey-13 compared with the comprehensive geriatric assessment for identifying disability in older patients with prostate cancer who receive androgen ablation. Cancer 109:802–810
Veronese N, Custodero C, Cella A, Demurtas J, Zora S, Maggi S, Barbagallo M, Sabba C, Ferrucci L, Pilotto A (2021) Prevalence of multidimensional frailty and pre-frailty in older people in different settings: A systematic review and meta-analysis. Ageing Res Rev 72:101498
Gilmore N, Kehoe L, Bauer J, Xu H, Hall B, Wells M, Lei L, Culakova E, Flannery M, Grossman VA, Sardari RA, Subramanya H, Kadambi S, Belcher E, Kettinger J, O’Rourke MA, Dib EG, Vogelzang NJ, Dale W, Mohile S (2021) The relationship between frailty and emotional health in older patients with advanced cancer. Oncologist 26:e2181–e2191
Komici K, Bencivenga L, Navani N, D’Agnano V, Guerra G, Bianco A, Rengo G, Perrotta F (2022) Frailty in patients with lung cancer: a systematic review and meta-analysis. Chest 162:485–497
Wang S, Yang T, Qiang W, Shen A, Zhao Z, Yang H, Liu X (2022) The prevalence of frailty among breast cancer patients: a systematic review and meta-analysis. Support Care Cancer 30:2993–3006
Zhang Q, Zhang M, Hu S, Meng L, Xi J, Xu A, Zhang Y, Yu S (2022) Prevalence and risk factors of preoperative frailty in Chinese elderly inpatients with gastric and colorectal cancer undergoing surgery: a single-center cross-sectional study using the Groningen Frailty Indicator. Support Care Cancer 30:677–686
Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA (2017) Frailty and cancer: Implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 67:362–377
Chou WC, Chang PH, Chen PT, Wang HM, Yeh KY, Lu CH, Hung YS, Tung-Chieh Chang J, Tsang NM, Ho YW, Chen SY, Lee SH, Hung CY, Wang LJ, Liao KC, Lin CH, Tang WR, Lin YC (2020) Clinical significance of vulnerability assessment in patients with primary head and neck cancer undergoing definitive concurrent chemoradiation therapy. Int J Radiat Oncol Biol Phys 108:602–611
Bolukbas F, Kutluturkan S (2014) Symptoms and symptom clusters in non Hodgkin’s lymphoma patients in Turkey. Asian Pac J Cancer Prev 15:7153–7158
Nolden A, Joseph PV, Kober KM, Cooper BA, Paul SM, Hammer MJ, Dunn LB, Conley YP, Levine JD, Miaskowski C (2019) Co-occurring gastrointestinal symptoms are associated with taste changes in oncology patients receiving chemotherapy. J Pain Symptom Manage 58:756–765
Boltong A, Aranda S, Keast R, Wynne R, Francis PA, Chirgwin J, Gough K (2014) A prospective cohort study of the effects of adjuvant breast cancer chemotherapy on taste function, food liking, appetite and associated nutritional outcomes. PLoS ONE 9:e103512
Drareni K, Bensafi M, Giboreau A, Dougkas A (2021) Chemotherapy-induced taste and smell changes influence food perception in cancer patients. Support Care Cancer 29:2125–2132
Granström B, Holmlund T, Laurell G, Fransson P, TiblomEhrsson Y (2022) Addressing symptoms that affect patients’ eating according to the Head and Neck Patient Symptom Checklist©. Support Care Cancer 30:6163–6173
Marinho EDC, Custodio IDD, Ferreira IB, Crispim CA, Paiva CE, Maia YCP (2017) Impact of chemotherapy on perceptions related to food intake in women with breast cancer: A prospective study. PLoS ONE 12:e0187573
de Vries YC, Boesveldt S, Kelfkens CS, Posthuma EE, van den Berg M, de Kruif J, Haringhuizen A, Sommeijer DW, Buist N, Grosfeld S, de Graaf C, van Laarhoven HWM, Kampman E, Winkels RM (2018) Taste and smell perception and quality of life during and after systemic therapy for breast cancer. Breast Cancer Res Treat 170:27–34
Kiss N, Symons K, Hewitt J, Davis H, Ting C, Lee A, Boltong A, Tucker RM, Tan SY (2021) Taste function in adults undergoing cancer radiotherapy or chemotherapy, and implications for nutrition management: a systematic review. J Acad Nutr Diet 121:278–304
Chen SI, Chiang CL, Chao CT, Chiang CK, Huang JW (2021) Gustatory dysfunction is closely associated with frailty in patients with chronic kidney disease. J Ren Nutr 31:49–56
Bernstein IA, Roxbury CR, Lin SY, Rowan NR (2021) The association of frailty with olfactory and gustatory dysfunction in older adults: a nationally representative sample. Int Forum Allergy Rhinol 11:866–876
Feczko E, Miranda-Dominguez O, Marr M, Graham AM, Nigg JT, Fair DA (2019) The heterogeneity problem: approaches to identify psychiatric subtypes. Trends Cogn Sci 23:584–601
Wallström S, Sutherland JM, Kopec JA, Anis AH, Sawatzky R (2022) Distinguishing symptom patterns in adults newly diagnosed with cancer: a latent class analysis. J Pain Symptom Manage 64:146–155
Singh K, Pituch K, Zhu Q, Gu H, Ernst B, Tofthagen C, Brewer M, Kober KM, Cooper BA, Paul SM, Conley YP, Hammer M, Levine JD, Miaskowski C (2023) Distinct nausea profiles are associated with gastrointestinal symptoms in oncology patients receiving chemotherapy. Cancer Nurs 46:92–102
Thong MSY, Mols F, van de Poll-Franse LV, Sprangers MAG, van der Rijt CCD, Barsevick AM, Knoop H, Husson O (2018) Identifying the subtypes of cancer-related fatigue: results from the population-based PROFILES registry. J Cancer Surviv 12:38–46
Hammer MJ, Cooper B, Paul SM, Kober KM, Cartwright F, Conley YP, Wright F, Levine JD, Miaskowski C (2022) Identification of distinct symptom profiles in cancer patients using a pre-specified symptom cluster. J Pain Symptom Manage 64:17–27
Kano T, Kanda K (2013) Development and validation of a chemotherapy-induced taste alteration scale. Oncol Nurs Forum 40:E79-85
Saliba D, Elliott M, Rubenstein LZ, Solomon DH, Young RT, Kamberg CJ, Roth C, MacLean CH, Shekelle PG, Sloss EM, Wenger NS (2001) The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc 49:1691–1699
Rodin MB, Mohile SG (2007) A practical approach to geriatric assessment in oncology. J Clin Oncol 25:1936–1944
Griffith KA, Zhu S, Johantgen M, Kessler MD, Renn C, Beutler AS, Kanwar R, Ambulos N, Cavaletti G, Bruna J, Briani C, Argyriou AA, Kalofonos HP, Yerges-Armstrong LM, Dorsey SG (2017) Oxaliplatin-induced peripheral neuropathy and identification of unique severity groups in colorectal cancer. J Pain Symptom Manage 54:701–706
Spotten LE, Corish CA, Lorton CM, Ui DPM, O’Donoghue NC, O’Connor B, Walsh TD (2017) Subjective and objective taste and smell changes in cancer. Ann Oncol 28:969–984
Handforth C, Clegg A, Young C, Simpkins S, Seymour MT, Selby PJ, Young J (2015) The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol 26:1091–1101
de Vries J, Bras L, Sidorenkov G, Festen S, Steenbakkers R, Langendijk JA, Witjes MJH, van der Laan B, de Bock GH, Halmos GB (2020) Frailty is associated with decline in health-related quality of life of patients treated for head and neck cancer. Oral Oncol 111:105020
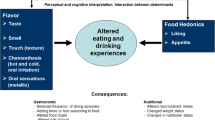
Epstein JB, Smutzer G, Doty RL (2016) Understanding the impact of taste changes in oncology care. Support Care Cancer 24:1917–1931
Shaw JF, Budiansky D, Sharif F, McIsaac DI (2022) The association of frailty with outcomes after cancer surgery: a systematic review and metaanalysis. Ann Surg Oncol 29:4690–4704
Sozeri E, Kutluturkan S (2015) Taste alteration in patients receiving chemotherapy. J Breast Health 11:81–87
Ferrat E, Audureau E, Paillaud E, Liuu E, Tournigand C, Lagrange JL, Canoui-Poitrine F, Caillet P, Bastuji-Garin S (2016) Four distinct health profiles in older patients with cancer: latent class analysis of the prospective ELCAPA cohort. J Gerontol A Biol Sci Med Sci 71:1653–1660
Looman WM, Fabbricotti IN, Blom JW, Jansen APD, Lutomski JE, Metzelthin SF, Huijsman R (2018) The frail older person does not exist: development of frailty profiles with latent class analysis. BMC Geriatr 18:84
Murtaza B, Hichami A, Khan AS, Ghiringhelli F, Khan NA (2017) Alteration in taste perception in cancer: causes and strategies of treatment. Front Physiol 8:134
Lesser GJ, Irby MB, Taylor RC, Snavely A, Case D, Wang A, Dietrich A, Duncan S (2022) Lactoferrin supplementation for taste and smell abnormalities among patients receiving cancer chemotherapy. Support Care Cancer 30:2017–2025
von Grundherr J, Koch B, Grimm D, Salchow J, Valentini L, Hummel T, Bokemeyer C, Stein A, Mann J (2019) Impact of taste and smell training on taste disorders during chemotherapy - TASTE trial. Cancer Manag Res 11:4493–4504
Kinjo T, Kanda K, Fujimoto K (2021) Effects of a self-monitoring intervention in breast cancer patients suffering from taste alterations induced by chemotherapy: A randomized, parallel-group controlled trial. Eur J Oncol Nurs 52:101956
Wada Y, Nishi M, Yoshikawa K, Takasu C, Tokunaga T, Nakao T, Kashihara H, Yoshimoto T, Shimada M (2022) Preoperative nutrition and exercise intervention in frailty patients with gastric cancer undergoing gastrectomy. Int J Clin Oncol 27:1421–1427
Huang SM, Tseng LM, Chien LY, Tai CJ, Chen PH, Hung CT, Hsiung Y (2016) Effects of non-sporting and sporting qigong on frailty and quality of life among breast cancer patients receiving chemotherapy. Eur J Oncol Nurs 21:257–265
Johal J, Han CY, Joseph R, Munn Z, Agbejule OA, Crawford-Williams F, Wallen MP, Chan RJ, Hart NH (2022) Dietary supplements in people with metastatic cancer who are experiencing malnutrition, cachexia, sarcopenia, and frailty: a scoping review. Nutrients 14:2642
Murphy BA, Deng J (2015) Advances in supportive care for late effects of head and neck cancer. J Clin Oncol 33:3314–3321
Amezaga J, Alfaro B, Rios Y, Larraioz A, Ugartemendia G, Urruticoechea A, Tueros I (2018) Assessing taste and smell alterations in cancer patients undergoing chemotherapy according to treatment. Support Care Cancer 26:4077–4086
Wang Y, Lu Q, Zhang L, Zhuang B, Zhang T, Jin S, Sun Y, Xiao S, Zheng B, Fang Y, Gong L, Wang Y, Cao Y, Wang W (2021) Nutrition impact symptom clusters in patients with head and neck cancer receiving concurrent chemoradiotherapy. J Pain Symptom Manage 62:277–285
Malta CEN, de Lima MJO, Carlos A, Freitas MO, Magalhaes IA, de Vasconcelos HCA, de Lima S-FIJ, de Barros SPG (2022) Risk factors for dysgeusia during chemotherapy for solid tumors: a retrospective cross-sectional study. Support Care Cancer 30:313–325
Ishikawa M, Shibata T, Iwata T, Nishio S, Takada T, Suzuki S, Horie K, Kudaka W, Kagabu M, Tanikawa M, Kitagawa R, Takekuma M, Kobayashi H, Yaegashi N (2021) A randomized phase II/III trial of conventional paclitaxel and carboplatin with or without bevacizumab versus dose-dense paclitaxel and carboplatin with or without bevacizumab, in stage IVB, recurrent, or persistent cervical carcinoma (JCOG1311): Primary analysis. Gynecol Oncol 162:292–298
Aprahamian I, Sassaki E, Dos Santos MF, Izbicki R, Pulgrossi RC, Biella MM, Borges AC, Sassaki MM, Torres LM, Fernandez ÍS, Pião OA (2018) Hypertension and frailty in older adults. J Clin Hypertens 20:186–192
Duan L, Cui H, Zhang W, Wu S (2022) Symptoms and experiences of frailty in lung cancer patients with chemotherapy: A mixed-method approach. Front Oncol 12:1019006
Koll TT, Semin JN, Brodsky R, Keehn D, Fisher AL, High R, Beadle JN (2021) Health-related and sociodemographic factors associated with physical frailty among older cancer survivors. J Geriatr Oncol 12:96–101
Saracino RM, Cham H, RosenfeldNelson BJC (2020) Latent profile analyses of depressive symptoms in younger and older oncology patients. Assessment 27:1383–1398
Funding
This study was supported by National Natural Science Foundation of China (No. 82172583), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (BJ 2020041), Key Speciality of Precision Medicine from Wuxi Health and Family Planning Commission (J 201807).
Author information
Authors and Affiliations
Contributions
MZ, TW, JS, ZZ and DW were responsible for patient recruitment and data collection. LT guided MZ and TW with the data analysis. MZ, TW and LT contributed to writing the paper. All authors reviewed the findings, agreed with the interpretation, and read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Jiangnan University (approval no. JNU20210918IRB04).
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent to publish All of the authors read the final version of the paper and approved its submission for publication.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, M., Wang, T., Sun, J. et al. Heterogeneity of vulnerability and taste changes in older cancer patients undergoing chemotherapy: a latent class analysis. Support Care Cancer 31, 392 (2023). https://doi.org/10.1007/s00520-023-07862-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07862-9