Abstract
Purpose
To determine the effectiveness of mobile health-based self-management interventions on medical/behavioral, role, and emotional management in breast cancer patients.
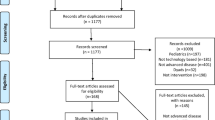
Methods
The Embase, MEDLINE, SINOMED, the Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), WanFang, and Weipu (VIP) databases were extensively searched from inception to November 30, 2020, to identify eligible clinical trials. Outcomes included medical/behavioral management (self-management behavior, functional exercise compliance, self-efficacy, complications, and symptoms), role management (role functioning), and emotional management (anxiety and depression), social support, and health-related quality of life.
Results
Twenty-four studies were included in this meta-analysis. The results of the meta-analysis indicated that mobile health-based self-management interventions could potentially improve breast cancer patients’ self-management behavior, functional exercise compliance (WMD = 15.80, 95% CI = 10.53 to 21.08, P < 0.001), self-efficacy (SMD = 1.22, 95% CI = 0.57 to 1.87, P < 0.001), and health-related quality of life (SMD = 0.78, 95% CI = 0.44 to 1.12, P < 0.001); reduce the incidence of lymphedema (RR = 0.20, 95% CI = 0.15 to 0.26, P < 0.001); and relieve the level of anxiety (SMD = − 0.67, 95% CI = − 0.99 to − 0.35, P < 0.001). However, patients assigned to the mobile health group and the conventional care group did not differ significantly in symptom relief (including pain and fatigue), role functioning, depression, or social support (all P ≥ 0.05).
Conclusion
Mobile health–based self-management interventions can potentially facilitate the self-management and health-related quality of life of breast cancer patients.




Similar content being viewed by others
Data availability
N/A.
Code availability
N/A.
References
The International Agency for Research on Cancer (IARC) (2020) Latest global cancer data: cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. https://www.iarc.fr/faq/latest-global-cancer-data-2020-qa/ Accessed 4 Jan 2021
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30. https://doi.org/10.3322/caac.21590
De Vrieze T, Nevelsteen I, Thomis S, De Groef A, Tjalma W, Gebruers N, Devoogdt N (2020) What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer 28:439–449. https://doi.org/10.1007/s00520-019-05101-8
Ho PJ, Gernaat S, Hartman M, Verkooijen HM (2018) Health-related quality of life in Asian patients with breast cancer: a systematic review. BMJ Open 8:e20512. https://doi.org/10.1136/bmjopen-2017-020512
Chou YH, Chia-Rong HV, Chen X, Huang TY, Shieh SH (2020) Unmet supportive care needs of survival patients with breast cancer in different cancer stages and treatment phases. Taiwan J Obstet Gynecol 59:231–236. https://doi.org/10.1016/j.tjog.2020.01.010
Gálvez-Hernández CL, Boyes A, Ortega-Mondragón A, Romo-González AG, Mohar A, Mesa-Chavez F, Oñate-Ocaña L, Villarreal-Garza C (2021) Unmet needs among breast cancer patients in a developing country and supportive care needs survey validation. Rev Invest Clin 73:245–250. https://doi.org/10.24875/RIC.21000068
Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26:1–7. https://doi.org/10.1207/S15324796ABM2601_01
Robert WJ (2002) Essential elements of self-management interventions. Center for the Advancement of Health, Washington, DC
Zhou K, Wang W, Zhao W, Li L, Zhang M, Guo P, Zhou C, Li M, An J, Li J, Li X (2020) Benefits of a WeChat-based multimodal nursing program on early rehabilitation in postoperative women with breast cancer: a clinical randomized controlled trial. Int J Nurs Stud 106:103–565. https://doi.org/10.1016/j.ijnurstu.2020.103565
Admiraal JM, van der Velden A, Geerling JI, Burgerhof J, Bouma G, Walenkamp A, de Vries E, Schröder CP, Reyners A (2017) Web-based tailored psychoeducation for breast cancer patients at the onset of the survivorship phase: a multicenter randomized controlled trial. J Pain Symptom Manage 54:466–475. https://doi.org/10.1016/j.jpainsymman.2017.07.009
Chee W, Lee Y, Im E, Chee E, Tsai H, Nishigaki M, Yeo SA, Schapira MM, Mao JJ (2017) A culturally tailored Internet cancer support group for Asian American breast cancer survivors: a randomized controlled pilot intervention study. J Telemed Telecare 23:618–626. https://doi.org/10.1177/1357633X16658369
Kim HJ, Kim HS (2020) Effects of a web-based expert support self-management program (WEST) for women with breast cancer: a randomized controlled trial. J Telemed Telecare 26:433–442. https://doi.org/10.1177/1357633X19850386
Kim HJ, Kim SM, Shin H, Jang JS, Kim YI, Han DH (2018) A mobile game for patients with breast cancer for chemotherapy self-management and quality-of-life improvement: randomized controlled trial. J Med Internet Res 20:e273. https://doi.org/10.2196/jmir.9559
Zhang Y (2019). Construction and empirical study of self-management intervention program based on mobile health application for breast cancer patients. the PLA Naval Medical University
Zhu J, Ebert L, Liu X, Wei D, Chan SW (2018) Mobile breast cancer e-support program for chinese women with breast cancer undergoing chemotherapy (Part 2): Multicenter Randomized Controlled Trial. JMIR MHEALTH AND UHEALTH 6:e104. https://doi.org/10.2196/mhealth.9438
Zhou H, Wang J, Li S (2019) Effect of WeChat supported hospital-family collaborative transitional care on postoperative functional recovery in breast cancer patients. J Nurs Sci 34:63–66
Pope ZC, Zeng N, Zhang R, Lee H Y, Gao Z (2018). Effectiveness of combined smartwatch and social media intervention on breast cancer survivor health outcomes: a 10-week pilot randomized trial. J Clin Med 7:140. https://doi.org/10.3390/jcm7060140
Kapoor A, Nambisan P, Baker E (2020). Mobile applications for breast cancer survivorship and self-management: A systematic review. Health Informatics J 26: 2892–2905. https://doi.org/10.1177/1460458220950853
Liao Y, Wang B, Han L (2017) An application effect study on the self-management of breast cancer patients by the establishment of the “fans” club informatization. Chinese Journal of Practical Nursing 33:241–244
Lu Y (2019). Construction and research of cloud platform of targeted drug therapy based on self-management model for breast cancer patients. Nanjing University of Traditional Chinese Medicine
Wu Q, Kue J, Zhu X, Yin X, Jiang J, Chen J, Yang L, Zeng L, Sun X, Liu X, Duan X, Shi Y (2020) Effects of Nurse-Led Support Via WeChat, a smartphone application, for breast cancer patients after surgery: a quasi-experimental study. Telemedicine and E-Health 26:226–234. https://doi.org/10.1089/tmj.2018.0293
Lee MK, Yun YH, Park HA, Lee ES, Jung KH, Noh DY (2014) A Web-based self-management exercise and diet intervention for breast cancer survivors: pilot randomized controlled trial. Int J Nurs Stud 51:1557–1567. https://doi.org/10.1016/j.ijnurstu.2014.04.012
Huang J, Han Y, Wei J, Liu X, Du Y, Yang L, Li Y, Yao W, Wang R (2020) The effectiveness of the Internet-based self-management program for cancer-related fatigue patients: a systematic review and meta-analysis. Clin Rehabil 34:287–298. https://doi.org/10.1177/0269215519889394
Xu A, Wang Y, Wu X (2019) Effectiveness of e-health based self-management to improve cancer-related fatigue, self-efficacy and quality of life in cancer patients: Systematic review and meta-analysis. J Adv Nurs 75:3434–3447. https://doi.org/10.1111/jan.14197
Kim AR, Park HA (2015) Web-based self-management support interventions for cancer survivors: a systematic review and meta-analyses. Stud Health Technol Inform 216:142–147
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151:W65–W94. https://doi.org/10.7326/0003-4819-151-4-200908180-00136
Versel N (2020). Mobile takes its place on health IT scene. https://www.himss.org/mhealth. Accessed 21 Oct 2020
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Hong Z, Zhen W (2011) Calculation of standardized mean difference effect size in Meta analysis. Chinese Journal of Tissue Engineering Research 15:737–740
Noble D, Lagisz M, O’Dea RE, Nakagawa S (2017) Nonindependence and sensitivity analyses in ecological and evolutionary meta-analyses. Mol Ecol 26:2410–2425. https://doi.org/10.1111/mec.14031
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH, Tetzlaff J, Deeks JJ, Peters J, Macaskill P, Schwarzer G, Duval S, Altman DG, Moher D, Higgins JP (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. https://doi.org/10.1136/bmj.d4002
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Kong H, Zhou L, Hong L, Zhang Y, Ji F, Sun L (2018) The effect of continuous nursing based on WeChat platform on quality of life and psychological quality of postoperative breast cancer patients. Journal of Nursing and Rehabilitation 17:19–23
Qin Q (2018) Application of WeChat platform in postoperative extended care of breast cancer. Modern Diagnosis and Treatment 29:2319–2321
Zha G (2020) Effects of WeChat continuous nursing on psychological stress, self-care ability and quality of life of breast cancer patients undergoing chemotherapy after radical mastectomy. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease 28:148–150
Zhou L, Kong H (2019) Effects of WeChat platform continuing nursing intervention on mental resilience and stigma of postoperative breast cancer patients. Chinese Journal of General Practice 17:1773–1776
Shi S (2018) Application and effect analysis of WeChat platform in postoperative nursing of breast cancer patients. Hospital Management Forum 35:44–46
Wei S, Yang X (2019) Effects of WeChat-based continuous care on quality of life and functional exercise compliance of breast cancer patients. Health Medicine Research and Practice 16:66–68
Omidi Z, Kheirkhah M, Abolghasemi J, Haghighat S (2020) Effect of lymphedema self-management group-based education compared with social network-based education on quality of life and fear of cancer recurrence in women with breast cancer: a randomized controlled clinical trial. Qual Life Res 29:1789–1800. https://doi.org/10.1007/s11136-020-02455-z
Dong X, Yi X, Gao D, Gao Z, Huang S, Chao M, Chen W, Ding M (2019) The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients:a randomized controlled trial. Health Qual Life Outcomes 17:109. https://doi.org/10.1186/s12955-019-1183-0
van den Berg SW, Gielissen MF, Custers JA, van der Graaf WT, Ottevanger PB, Prins JB (2015) BREATH: web-based self-management for psychological adjustment after primary breast cancer—results of a multicenter randomized controlled trial. J Clin Oncol 33:2763–2771. https://doi.org/10.1200/JCO.2013.54.9386
Zhang L, Fan A, Yan J, He Y, Zhang H, Zhang H, Zhong Q, Liu F, Luo Q, Zhang L, Tang H, Xin M (2016) Combining manual lymph drainage with physical exercise after modified radical mastectomy effectively prevents upper limb lymphedema. Lymphat Res Biol 14:104–108. https://doi.org/10.1089/lrb.2015.0036
Li Y, Li L, Liu A, Zhang X (2019). Application of case management mode based on mobile phone APP in functional exercise of patients after breast cancer operation. Chinese Journal of Modern Nursing 12: 1518–1522
Uhm KE, Yoo JS, Chung SH, Lee JD, Lee I, Kim JI, Lee SK, Nam SJ, Park YH, Lee JY, Hwang JH (2017) Effects of exercise intervention in breast cancer patients: is mobile health (mHealth) with pedometer more effective than conventional program using brochure? Breast Cancer Res Treat 161:443–452. https://doi.org/10.1007/s10549-016-4065-8
Glanz K, Bishop DB (2010) The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 31:399–418. https://doi.org/10.1146/annurev.publhealth.012809.103604
Kim SH, Kim K, Mayer DK (2017) Self-Management Intervention for Adult Cancer Survivors After Treatment: A Systematic Review and Meta-Analysis. Oncol Nurs Forum 44:719–728. https://doi.org/10.1188/17.ONF.719-728
De Groef A, Van Kampen M, Dieltjens E, Christiaens MR, Neven P, Geraerts I, Devoogdt N (2015) Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: a systematic review. Arch Phys Med Rehabil 96:1140–1153. https://doi.org/10.1016/j.apmr.2015.01.006
Sai Z, Fan-Jie M (2013) Upper limb exercise and breast cancer related lymphedema. Int J Oncol 40:36–39. https://doi.org/10.3760/cma.j.issn.1673-422X.2013.01.011
Chen YY, Guan BS, Li ZK, Li XY (2018) Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J Telemed Telecare 24:157–167. https://doi.org/10.1177/1357633X16686777
Paterson C, Robertson A, Nabi G (2015) Exploring prostate cancer survivors’ self-management behaviours and examining the mechanism effect that links coping and social support to health-related quality of life, anxiety and depression: a prospective longitudinal study. Eur J Oncol Nurs 19:120–128. https://doi.org/10.1016/j.ejon.2014.10.008
Maughan KL, Lutterbie MA, Ham PS (2010) Treatment of breast cancer. Am Fam Physician 81:1339–1346
Gottrup H, Andersen J, Arendt-Nielsen L, Jensen TS (2000) Psychophysical examination in patients with post-mastectomy pain. Pain 87:275–284. https://doi.org/10.1016/S0304-3959(00)00291-8
Pieretti S, Di Giannuario A, Di Giovannandrea R, Marzoli F, Piccaro G, Minosi P, Aloisi AM (2016) Gender differences in pain and its relief. Ann Ist Super Sanita 52:184–189. https://doi.org/10.4415/ANN_16_02_09
Singer S, Kuhnt S, Zwerenz R, Eckert K, Hofmeister D, Dietz A, Giesinger J, Hauss J, Papsdorf K, Briest S, Brown A (2011) Age- and sex-standardised prevalence rates of fatigue in a large hospital-based sample of cancer patients. Br J Cancer 105:445–451. https://doi.org/10.1038/bjc.2011.251
Gamper EM, Petersen MA, Aaronson N, Costantini A, Giesinger JM, Holzner B, Kemmler G, Oberguggenberger A, Singer S, Young T, Groenvold M (2016) Development of an item bank for the EORTC Role Functioning Computer Adaptive Test (EORTC RF-CAT). Health Qual Life Outcomes 14:72. https://doi.org/10.1186/s12955-016-0475-x
Li Q, Lin Y, Qiu Y, Gao B, Xu Y (2014) The assessment of health-related quality of life and related factors in Chinese elderly patients undergoing chemotherapy for advanced cancer: a cross-sectional study. Eur J Oncol Nurs 18:425–435. https://doi.org/10.1016/j.ejon.2014.03.005
Goodman SH, Sewell DR, Cooley EL, Leavitt N (1993) Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment Health J 29:119–131. https://doi.org/10.1007/BF00756338
Lu Q, Man J, You J, Leroy AS (2015) The link between ambivalence over emotional expression and depressive symptoms among Chinese breast cancer survivors. J Psychosom Res 79:153–158. https://doi.org/10.1016/j.jpsychores.2015.01.007
Kim E, Han JY, Moon TJ, Shaw B, Shah DV, Mctavish FM, Gustafson DH (2012) The process and effect of supportive message expression and reception in online breast cancer support groups. Psychooncology 21:531–540. https://doi.org/10.1002/pon.1942
Pingree S, Hawkins R, Baker T, Dubenske L, Roberts LJ, Gustafson DH (2010) The value of theory for enhancing and understanding e-health interventions. Am J Prev Med 38:103–109. https://doi.org/10.1016/j.amepre.2009.09.035
Ventura F, Ohlén J, Koinberg I (2013) An integrative review of supportive e-health programs in cancer care. Eur J Oncol Nurs 17:498–507. https://doi.org/10.1016/j.ejon.2012.10.007
Funding
This work was supported by China’s National Natural Science Foundation (no. 71974217).
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to conception and design, or acquisition of data, or analysis and interpretation of data. All authors contributed in drafting the article or revising it critically for important intellectual content. All authors approved the version to be published.
Conceptualization: Jun Yan
Acquisition of data: Xia Luo and Yuzhen Chen
Analysis and/or interpretation of data: Xia Luo and Jing Chen
Drafting the manuscript: Xia Luo and Yuzhen Chen
Revising the manuscript critically for important intellectual content: Jun Yan and Yue Zhang, and Jing Chen
Data validation: Jun Yan, Mingfang Li, Chenxia Xiong, and Jing Chen
Supervision: Jun Yan
Corresponding author
Ethics declarations
Ethics approval
N/A
Consent to participate
N/A
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Luo, X., Chen, Y., Chen, J. et al. Effectiveness of mobile health-based self-management interventions in breast cancer patients: a meta-analysis. Support Care Cancer 30, 2853–2876 (2022). https://doi.org/10.1007/s00520-021-06568-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06568-0