Abstract
Background
Sleep disturbance is the most common and distressing cancer symptom that negatively affects the quality of life (QoL). The main objective of this study is to determine the prevalence of sleep disturbance among Arabic women with breast cancer, post-treatment, and assess their sleep disturbance in relation to health-related QoL, demographics and treatment characteristics.
Methods
In this study, cross-sectional data were collected using the Pittsburgh Sleep Quality Index (PSQI: 19-items) and the Functional Assessment of Cancer Therapy-General (FACT-G: 27 items). Demographic information and treatment characteristics were also collected.
Results
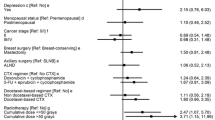
A total of 133 women who had been diagnosed with breast cancer agreed to participate in the study. Approximately three-quarters (73.7%; n = 98) of the participants was reported as poor sleepers (PSQI ˃ 5). The worse mean score of the PSQI component was the sleep latency with the highest score (M = 1.71, SD = 0.93). There were significant relationships between poor sleep and treatment (patients receiving both chemotherapy and radiotherapy) and with comorbidities (asthma, anaemia, hypertension/heart failure, diabetes/heart diseases) (P < 0.05). Those experiencing poor sleep had the lowest QoL among the cancer patients.
Conclusion
Sleep disturbance is a significant problem for Arabic patients diagnosed with breast cancer. The result suggests that sleep disturbance should be routinely assessed in clinical settings. Further research should develop an intervention for management to reduce sleep disturbance and improve sleep quality in cancer patients.

Similar content being viewed by others
Data Availability
The corresponding author has full control of all primary data. Primary data is available on request.
References
Berger AM (2009) Update on the state of the science: sleep-wake disturbances in adult patients with cancer. Oncol Nurs Forum 36:E165–E177. https://doi.org/10.1188/09.ONF.E165-E177
Otte JL, Carpenter JS, Russell KM, Bigatti S, Champion VL (2010) Prevalence, severity, and correlates of sleep-wake disturbances in long-term breast cancer survivors. J Pain Symptom Manag 39:535–547. https://doi.org/10.1016/j.jpainsymman.2009.07.004
Berger AM, Parker KP, Young-McCaughan S, Mallory GA, Barsevick AM, Beck SL, Carpenter JS, Carter PA, Farr LA, Hinds PS, Lee KA, Miaskowski C, Mock V, Payne JK, Hall M (2005) Sleep wake disturbances in people with cancer and their caregivers: state of the science. Oncol Nurs Forum 32:E98–E126. https://doi.org/10.1188/05.ONF.E98-E126
Clark J, Cunningham M, McMillan S, Vena C, Parker K (2004) Sleep-wake disturbances in people with cancer part II: evaluating the evidence for clinical decision making. Oncol Nurs Forum 31:747–771. https://doi.org/10.1188/04.ONF.747-771
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318. https://doi.org/10.1016/S2213-2600(15)00043-0
Lowery-Allison AE, Passik SD, Cribbet MR, Reinsel RA, O'Sullivan B, Norton L, Kirsh KL, Kavey NB (2018) Sleep problems in breast cancer survivors 1–10 years posttreatment. Palliat Support Care 16:325–334. https://doi.org/10.1017/S1478951517000311
Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D (2013) Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum 40:35–42. https://doi.org/10.1188/13.ONF.35-42
National Institutes of Health (2011) National institutes of health sleep disorders research plan. National Institutes of Health, Maryland
Berger AM, Matthews EE, Aloia MS (2018) Sleep and cancer. In: Olver I (ed) The MASCC textbook of cancer supportive care and survivorship. Springer International Publishing, Cham, pp 53–65
Otte JL, Davis L, Carpenter JS, Krier C, Skaar TC, Rand KL, Weaver M, Landis C, Chernyak Y, Manchanda S (2016) Sleep disorders in breast cancer survivors. Support Care Cancer 24:4197–4205. https://doi.org/10.1007/s00520-016-3247-6
Sateia MJ (2014) International classification of sleep disorders. Chest 146:1387–1394
American Academy of Sleep Medicine (ed) (2014) International classification of sleep disorders–third edition (ICSD-3), 3rd edn. American Academy of Sleep Medicine, Darien
Horesh U, Cotter WM (2016) Current research on linguistic variation in the Arabic-speaking world. Lang Ling Compass 10:370–381
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Al Maqbali M, Hughes C, Gracey J et al (2020) Validation of the Pittsburgh Sleep Quality Index (PSQI) with Arabic cancer patients. Sleep Biol Rhythms 0:1–7. https://doi.org/10.1007/s41105-020-00258-w
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579. https://doi.org/10.1200/JCO.1993.11.3.570
Webster K, Cella D, Yost K (2003) The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes 1:1–7. https://doi.org/10.1186/1477-7525-1-79
Al Maqbali M, Hughes C, Gracey J et al (2020) Psychometric properties of the Arabic version of the Functional Assessment of Chronic Illnesses Therapy–Fatigue in Arabic cancer patients. J Pain Symptom Manag 59:130–138.e2. https://doi.org/10.1016/j.jpainsymman.2019.10.008
Mansano-Schlosser TC, Ceolim MF, Valerio TD (2016) Sleep quality in women with breast cancer: an integrative review. Int Arch Med 9:1–17. https://doi.org/10.3823/2230
Abrahams HJG, Gielissen MFM, Verhagen CAHHVM, Knoop H (2018) The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: a systematic review. Clin Psychol Rev 63:1–11. https://doi.org/10.1016/j.cpr.2018.05.004
Klyushnenkova EN, Sorkin JD, Gallicchio L (2015) Association of obesity and sleep problems among breast cancer survivors: results from a registry-based survey study. Support Care Cancer 23:3437–3445. https://doi.org/10.1007/s00520-015-2692-y
Otte JL, Payne JK, Carpenter JS (2011) Nighttime variability in wrist actigraphy. J Nurs Meas 19:105–114
Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL (2017) Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 13:307–349. https://doi.org/10.5664/jcsm.6470
Schreier AM, Johnson LA, Vohra NA, Muzaffar M, Kyle B (2019) Post-treatment symptoms of pain, anxiety, sleep disturbance, and fatigue in breast cancer survivors. Pain Manag Nurs 20:146–151. https://doi.org/10.1016/j.pmn.2018.09.005
Savard J, Ivers H, Savard M-H, Morin CM (2015) Cancer treatments and their side effects are associated with aggravation of insomnia: results of a longitudinal study. Cancer 121:1703–1711. https://doi.org/10.1002/cncr.29244
Garland SN, Xie SX, Li Q, Seluzicki C, Basal C, Mao JJ (2017) Comparative effectiveness of electro-acupuncture versus gabapentin for sleep disturbances in breast cancer survivors with hot flashes: a randomized trial. Menopause N Y N 24:517–523. https://doi.org/10.1097/GME.0000000000000779
Ancoli-Israel S (2015) Sleep disturbances in cancer: a review. Sleep Med Res 6:45–49. https://doi.org/10.17241/smr.2015.6.2.45
Budhrani PH, Lengacher CA, Kip K, Tofthagen C, Jim H (2015) An integrative review of subjective and objective measures of sleep disturbances in breast cancer survivors. Clin J Oncol Nurs 19:185–191. https://doi.org/10.1188/15.CJON.185-191
Costa AR, Fontes F, Pereira S, Gonçalves M, Azevedo A, Lunet N (2014) Impact of breast cancer treatments on sleep disturbances - a systematic review. Breast Edinb Scotl 23:697–709. https://doi.org/10.1016/j.breast.2014.09.003
Aricò D, Raggi A, Ferri R (2016) Cognitive behavioral therapy for insomnia in breast cancer survivors: a review of the literature. Front Psychol 7. https://doi.org/10.3389/fpsyg.2016.01162
Banthia R, Malcarne VL, Ko CM, Varni JW, Sadler GR (2009) Fatigued breast cancer survivors: the role of sleep quality, depressed mood, stage, and age. Psychol Health 24:965–980. https://doi.org/10.1080/08870440802110831
Ziner KW, Sledge GW, Bell CJ, Johns S, Miller KD, Champion VL (2012) Predicting fear of breast cancer recurrence and self-efficacy in survivors by age at diagnosis. Oncol Nurs Forum 39:287–295. https://doi.org/10.1188/12.ONF.287-295
Henneghan AM, Carter P, Stuifbergan A, Parmelee B, Kesler S (2018) Relationships between self-reported sleep quality components and cognitive functioning in breast cancer survivors up to 10 years following chemotherapy. Psychooncology 27:1937–1943. https://doi.org/10.1002/pon.4745
Schmidt ME, Wiskemann J, Steindorf K (2018) Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual Life Res 27:2077–2086. https://doi.org/10.1007/s11136-018-1866-8
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80:40–52. https://doi.org/10.1016/j.biopsych.2015.05.014
Hopko DR, Lejuez CW, Ryba MM, Shorter RL, Bell JL (2016) Support for the efficacy of behavioural activation in treating anxiety in breast cancer patients. Clin Psychol 20:17–26. https://doi.org/10.1111/cp.12083
Peoples AR, Roscoe JA, Block RC, Heckler CE, Ryan JL, Mustian KM, Janelsins MC, Peppone LJ, Moore DF Jr, Coles C, Hoelzer KL, Morrow GR, Dozier AM (2017) Nausea and disturbed sleep as predictors of cancer-related fatigue in breast cancer patients: a multicenter NCORP study. Support Care Cancer 25:1271–1278. https://doi.org/10.1007/s00520-016-3520-8
Code availability
N/A.
Funding
Graduate Research Grants (GRG), Ministry of Higher Education, Research and Innovation, Oman.
Author information
Authors and Affiliations
Contributions
A.M. completed the data collection, statistical support, and provided analysis and conceptualization and design and the manuscript preparation.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local ethics committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al Maqbali, M. Sleep disturbance among Arabic breast cancer survivors. Support Care Cancer 29, 5179–5186 (2021). https://doi.org/10.1007/s00520-021-06088-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06088-x