Abstract
Purpose
The needs and experiences of palliative home care for patients with advanced cancer have received little research attention. We aimed to explore the needs and experiences of palliative home care among patients with advanced cancer in China.
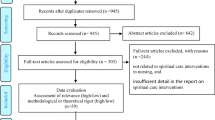
Methods
This qualitative study was conducted using semi-structured interviews with patients with advanced cancer. Participants (n = 15) were recruited from an oncology palliative care unit and a hospice outpatient unit, and were selected using purposive sampling from October 2019 to March 2020. Interviews were audio-recorded, transcribed verbatim, and subjected to thematic analysis. Two researchers coded the interviews independently in NVivo 12 and developed major themes and subthemes by inductive and constant comparison.
Results
Five themes were identified: (1) physical need; (2) psychological experience; (3) spiritual need; (4) social need; and (5) information need. Patients need to manage their symptoms (especially cancer pain), prolong life as long as possible, reconstruct their attitudes to adapt to their roles, be socially supported, be respected, maintain spiritual peace, and obtain more information about illness and home care.
Conclusions
The current palliative home care services are imperfect, and patients face substantial challenges, including physical symptoms, psychological/spiritual distress, and inadequate social support and information. Our findings may provide evidence and a reference for the development of palliative home care in China.
Similar content being viewed by others
References
Yan Y, Zhang H, Gao W, Liu D, Endo M, Deshpande GA, Uehara Y, Watanabe D, Yoshikawa S, Mizushima A (2020) Current awareness of palliative care in China. Lancet Glob Health 8(3):e333–e335. https://doi.org/10.1016/S2214-109X(20)30006-1
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Feng RM, Zong YN, Cao SM, Xu RH (2019) Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics? Cancer Commun (Lond) 39(1):22. https://doi.org/10.1186/s40880-019-0368-6
Yin Z, Li J, Ma K, Ning X, Chen H, Fu H, Zhang H, Wang C, Bruera E, Hui D (2017) Development of palliative care in China: a tale of three cities. Oncologist 22(11):1362–1367. https://doi.org/10.1634/theoncologist.2017-0128
Gomes B, Calanzani N, Gysels M, Hall S, Higginson IJ (2013) Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care 12:7. https://doi.org/10.1186/1472-684X-12-7
Ventura AD, Burney S, Brooker J, Fletcher J, Ricciardelli L (2014) Home-based palliative care: a systematic literature review of the self-reported unmet needs of patients and carers. Palliat Med 28(5):391–402. https://doi.org/10.1177/0269216313511141
Cai J, Zhao H, Coyte PC (2017) Socioeconomic differences and trends in the place of death among elderly people in China. Int J Environ Res Public Health 14(10). https://doi.org/10.3390/ijerph14101210
Li Ka Shing Foundation. “Heart of Gold” national hospice service program. Available at www.Hospice.com.cn. Accessed 07 July 2020
Shepperd S, Goncalves-Bradley DC, Straus SE, Wee B (2016) Hospital at home: home-based end-of-life care. Cochrane Database Syst Rev 2:CD009231. https://doi.org/10.1002/14651858.CD009231.pub2
Kerr CW, Donohue KA, Tangeman JC, Serehali AM, Knodel SM, Grant PC, Luczkiewicz DL, Mylotte K, Marien MJ (2014) Cost savings and enhanced hospice enrollment with a home-based palliative care program implemented as a hospice-private payer partnership. J Palliat Med 17(12):1328–1335. https://doi.org/10.1089/jpm.2014.0184
Chapman M, Johnston N, Lovell C, Forbat L, Liu WM (2018) Avoiding costly hospitalisation at end of life: findings from a specialist palliative care pilot in residential care for older adults. BMJ Support Palliat Care 8(1):102–109. https://doi.org/10.1136/bmjspcare-2015-001071
Maetens A, Beernaert K, De Schreye R, Faes K, Annemans L, Pardon K, Deliens L, Cohen J (2019) Impact of palliative home care support on the quality and costs of care at the end of life: a population-level matched cohort study. BMJ Open 9(1):e025180. https://doi.org/10.1136/bmjopen-2018-025180
Hudson P, Trauer T, Kelly B, O’Connor M, Thomas K, Zordan R, Summers M (2015) Reducing the psychological distress of family caregivers of home based palliative care patients: longer term effects from a randomised controlled trial. Psychooncology 24(1):19–24. https://doi.org/10.1002/pon.3610
Ciemins EL, Brant J, Kersten D, Mullette E, Dickerson D (2015) A qualitative analysis of patient and family perspectives of palliative care. J Palliat Med 18(3):282–285. https://doi.org/10.1089/jpm.2014.0155
Green A, Jerzmanowska N, Green M, Lobb EA (2018) ‘Death is difficult in any language’: a qualitative study of palliative care professionals’ experiences when providing end-of-life care to patients from culturally and linguistically diverse backgrounds. Palliat Med 32(8):1419–1427. https://doi.org/10.1177/0269216318776850
Herbstsomer RA, Stahl ST (2020) Cross-cultural experiences of hospice and palliative care services: a thematic analysis. Omega (Westport):30222820904205. https://doi.org/10.1177/0030222820904205
Bosma H, Apland L, Kazanjian A (2010) Cultural conceptualizations of hospice palliative care: more similarities than differences. Palliat Med 24(5):510–522. https://doi.org/10.1177/0269216309351380
Evans N, Menaca A, Koffman J, Harding R, Higginson IJ, Pool R, Gysels M, Prisma (2012) Cultural competence in end-of-life care: terms, definitions, and conceptual models from the British literature. J Palliat Med 15(7):812–820. https://doi.org/10.1089/jpm.2011.0526
Lee HT, Melia KM, Yao CA, Lin CJ, Chiu TY, Hu WY (2014) Providing hospice home care to the terminally ill elderly people with cancer in Taiwan: family experiences and needs. Am J Hosp Palliat Care 31(6):628–635. https://doi.org/10.1177/1049909113499603
Lai XB, Chen LQ, Chen SH, Xia HO (2019) An examination of home-based end-of-life care for cancer patients: a qualitative study. BMC Palliat Care 18(1):115. https://doi.org/10.1186/s12904-019-0501-y
Ritchie CS, Leff B, Garrigues SK, Perissinotto C, Sheehan OC, Harrison KL (2018) A quality of care framework for home-based medical care. J Am Med Dir Assoc 19(10):818–823. https://doi.org/10.1016/j.jamda.2018.05.020
Temkin-Greener H, Ladwig S, Caprio T, Norton S, Quill T, Olsan T, Cai X, Mukamel DB (2015) Developing palliative care practice guidelines and standards for nursing home-based palliative care teams: a Delphi study. J Am Med Dir Assoc 16(1):86.e81–86.e87. https://doi.org/10.1016/j.jamda.2014.10.013
Palinkas L, Horwitz S, Green C, Wisdom J, Duan N, Hoagwood K (2015) Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Hlth 42(5):533–544. https://doi.org/10.1007/s10488-013-0528-y
Bowen GA (2008) Naturalistic inquiry and the saturation concept: a research note. Qual Res 8(1):137–152. https://doi.org/10.1177/1468794107085301 Method
Guest G, Bunce A, Johnson L (2006) How many interviews are enough? An experiment with data saturation and variability. Field Method 18(1):59–82. https://doi.org/10.1177/1525822X05279903
Vasileiou K, Barnett J, Thorpe S, Young T (2018) Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 18(1):148. https://doi.org/10.1186/s12874-018-0594-7
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual. Res. Psychol. 3:77–101
Corbin J, Strauss A, Strauss AL (2014) Basics of qualitative research. Thousand Oaks, SAGE
Creswell J (2013) Qualitative inquiry and research design: choosing among five traditions, 3rd edn. Thousand Oaks, SAGE
Thomas E, Magilvy JK (2011) Qualitative rigor or research validity in qualitative research. J Spec Pediatr Nurs 16(2):151–155. https://doi.org/10.1111/j.1744-6155.2011.00283.x
Dehghan R, Ramakrishnan J, Uddin-Ahmed N, Harding R (2012) They patiently heard what we had to say... this felt different to me’: the palliative care needs and care experiences of advanced cancer patients and their families in Bangladesh. BMJ Support Palliat Care 2(2):145–149. https://doi.org/10.1136/bmjspcare-2011-000143
Zhai J, Weller-Newton JM, Shimoinaba K, Chen H, Copnell B (2020) Emerging from the “Ku:” fluctuating in adjusting with breast cancer-a post-traumatic growth theory situated within Chinese culture. Qual Health Res 30(11):1674–1683. https://doi.org/10.1177/1049732320930195
Kwon JH (2014) Overcoming barriers in cancer pain management. J Clin Oncol 32(16):1727–1733. https://doi.org/10.1200/JCO.2013.52.4827
Brooks JV, Poague C, Formagini T, Roberts AW, Sinclair CT, Keirns CC (2020) Palliative care’s role managing cancer pain during the opioid crisis: a qualitative study of patients, caregivers, and clinicians. J Pain Symptom Manage. 60:1127–1135.e2. https://doi.org/10.1016/j.jpainsymman.2020.06.039
Heydari H, Hojjat-Assari S, Almasian M, Pirjani P (2019) Exploring health care providers’ perceptions about home-based palliative care in terminally ill cancer patients. BMC Palliat Care 18(1):66. https://doi.org/10.1186/s12904-019-0452-3
Uslu-Sahan F, Terzioglu F, Koc G (2019) Hopelessness, death anxiety, and social support of hospitalized patients with gynecologic cancer and their caregivers. Cancer Nurs 42(5):373–380. https://doi.org/10.1097/NCC.0000000000000622
Lam WW, Yeo W, Suen J, Ho WM, Tsang J, Soong I, Yau TK, Wong KY, Sze WK, Ng AW, Kwong A, Suen D, Fong D, Ho S, Fielding R (2016) Goal adjustment influence on psychological well-being following advanced breast cancer diagnosis. Psycho-oncology 25(1):58–65. https://doi.org/10.1002/pon.3871
Tang ST, Chou WC, Chang WC, Chen JS, Hsieh CH, Wen FH, Chung SC (2019) Courses of change in good emotional preparedness for death and accurate prognostic awareness and their associations with psychological distress and quality of life in terminally ill cancer patients’ last year of life. J Pain Symptom Manage 58(4):623–631 e621. https://doi.org/10.1016/j.jpainsymman.2019.06.022
Chen HC, Chan SW, Yeh TP, Huang YH, Chien IC, Ma WF (2019) The spiritual needs of community-dwelling older people living with early-stage dementia-a qualitative study. J Nurs Scholarsh 51(2):157–167. https://doi.org/10.1111/jnu.12454
Philipp R, Mehnert A, Lo C, Muller V, Reck M, Vehling S (2019) Characterizing death acceptance among patients with cancer. Psychooncology 28(4):854–862. https://doi.org/10.1002/pon.5030
Bradley N, Lloyd-Williams M, Dowrick C (2018) Effectiveness of palliative care interventions offering social support to people with life-limiting illness-a systematic review. Eur J Cancer Care (Engl) 27(3):e12837. https://doi.org/10.1111/ecc.12837
Chen SC, Huang BS, Hung TM, Lin CY, Chang YL (2019) Impact of a behavior change program and health education on social interactions in survivors of head and neck cancer: randomized controlled trial. Psychooncology 28(2):293–300. https://doi.org/10.1002/pon.4939
Li X, Deng Y, Tang W, Sun Q, Chen Y, Yang C, Yan B, Wang Y, Wang J, Wang S, Yang F, Ding Y, Zhao G, Cao G (2018) Urban-rural disparity in cancer incidence, mortality, and survivals in Shanghai, China, during 2002 and 2015. Front Oncol 8:579. https://doi.org/10.3389/fonc.2018.00579
Gardiner C, Taylor B, Robinson J, Gott M (2019) Comparison of financial support for family caregivers of people at the end of life across six countries: a descriptive study. Palliat Med 33(9):1189–1211. https://doi.org/10.1177/0269216319861925
Salmasi S, Lee KS, Ming LC, Neoh CF, Elrggal ME, Babar ZD, Khan TM, Hadi MA (2017) Pricing appraisal of anti-cancer drugs in the South East Asian, Western Pacific and East Mediterranean Region. BMC Cancer 17(1):903. https://doi.org/10.1186/s12885-017-3888-y
Meng Q, Fang H, Liu X, Yuan B, Xu J (2015) Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet 386(10002):1484–1492. https://doi.org/10.1016/S0140-6736(15)00342-6
Dou G, Wang Q, Ying X (2018) Reducing the medical economic burden of health insurance in China: achievements and challenges. Biosci Trends 12(3):215–219. https://doi.org/10.5582/bst.2018.01054
Chen C, Pan J (2019) The effect of the health poverty alleviation project on financial risk protection for rural residents: evidence from Chishui City, China. Int J Equity Health 18(1):79. https://doi.org/10.1186/s12939-019-0982-6
Liu Y, Yang J, Huo D, Fan H, Gao Y (2018) Disclosure of cancer diagnosis in China: the incidence, patients’ situation, and different preferences between patients and their family members and related influence factors. Cancer Manag Res 10:2173–2181. https://doi.org/10.2147/CMAR.S166437
Smith-Uffen MES, Johnson SB, Martin AJ, Tattersall MHN, Stockler MR, Bell ML, Detering K, Clayton JM, Silvester W, Clarke S, Vaccaro L, Beale P, Kiely BE (2020) Estimating survival in advanced cancer: a comparison of estimates made by oncologists and patients. Support Care Cancer 28(7):3399–3407. https://doi.org/10.1007/s00520-019-05158-5
Acknowledgements
The authors would like to acknowledge Dr. Changrong Yuan (Nursing School, Fudan University, Shanghai, China) for her kind support for this study. The authors also would like to give special thanks to all the participants who generously shared their needs and experiences.
Funding
This study was funded by Shantou University Medical College in Shantou, China (Grant Number: NU201902) and the Li Ka Shing Foundation Cross-Disciplinary Research Grant (Grant Number: 2020LKSFG10B).
Author information
Authors and Affiliations
Contributions
Ying WJ and Liu XCh conceived in this qualitative study, and Ying WJ secured funding. Liu ZHL and Zheng RH conducted a review of the literature. Liu XCh, Ying WJ, Liu ZhL, Cao WH, Li WY, and Zheng RH developed the interview guide. Zheng RH, Li WY, Rui N, and Cao WH recruited all the participants and were accountable for all aspects of the interview. Liu XCh conducted the qualitative interviews. The transcription was conducted by Liu XCh and checked by Li WY and Liu XCh. Liu XCh and Chen QD independently coded all interview transcripts. The data were mainly analyzed by Ying WJ, Liu XCh, Liu ZhL, and Chen QD. The results were reviewed and confirmed by all co-authors. Liu XCh and Liu ZhL prepared and drafted the first manuscript. Zheng RH, Li WY, and Ying WJ critically revised the first manuscript for important content. Liu ZhL, Zheng RH, and Li WY reviewed and revised the subsequent version of the manuscript. All co-authors read and approved the final manuscript. Ying WJ submitted the final manuscript.
Corresponding author
Ethics declarations
Ethical approval involving humans
Approval was obtained from the ethics committee of the First Affiliated Hospital of Shantou University Medical College (protocol number 2019088) and Shantou Longhu People’s Hospital (protocol number LHLL2020005). All procedures implemented in studies involving human participants were in compliance with the institutional and/or national research committees on ethical standards and with the 1964 Helsinki Declaration and its subsequent amendments or similar ethical standards. Written informed consent was acquired from all participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, X., Liu, Z., Zheng, R. et al. Exploring the needs and experiences of palliative home care from the perspectives of patients with advanced cancer in China: a qualitative study. Support Care Cancer 29, 4949–4956 (2021). https://doi.org/10.1007/s00520-021-06037-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06037-8