Abstract
Background
Our study aimed to determine the prevalence of acute kidney injury (AKI) in pediatric non-traumatic rhabdomyolysis, and to identify factors associated with its development.
Methods
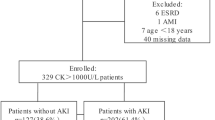
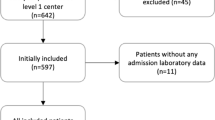
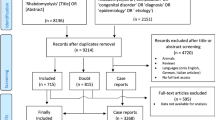
Clinical information and laboratory tests of children with rhabdomyolysis who were admitted between 2009 and 2018 were reviewed retrospectively. Rhabdomyolysis was defined by a peak serum creatine kinase (CK) level > 1000 IU/L within the first 72 h of admission. The primary outcome was the occurrence of AKI within the first 7 days of admission, which was determined by the KDIGO criteria.
Results
A total of 54 patients with a median age of 7.8 years old were included. Ten (18.5%) patients developed AKI. AKI was relatively rare in children with viral myositis (2.6%), whereas all patients with rhabdomyolysis related to seizure or irritability/dystonia developed AKI. Patients with AKI had higher white cell count (10.6 vs. 4.5 × 109/L) and lower serum bicarbonate (19.4 vs. 25.5 mmol/L) on admission, with higher peak serum CK (23,086.0 vs. 3959.5 IU/L). The AKI group was more likely to present with positive urine results (myoglobinuria, dipstick heme or protein ≥ 2+). Peak serum CK had a good discriminatory power for stage 2–3 AKI (AUC 0.930, p = 0.005), with an optimal cut-off of 15,000 IU/L identified from the ROC analysis.
Conclusions
The overall prevalence of AKI in pediatric non-traumatic rhabdomyolysis was 18.5%. Positive urine tests (myoglobinuria, dipstick heme or protein ≥ 2+), high white cell count, lower serum bicarbonate on admission, and high peak serum CK were associated with development of AKI.
Graphical abstract




Similar content being viewed by others
References
Chavez LO, Leon M, Einav S, Varon J (2016) Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Crit Care 20:135
Yang J, Zhou J, Wang X, Wang S, Tang Y, Yang L (2020) Risk factors for severe acute kidney injury among patients with rhabdomyolysis. BMC Nephrol 21:498
Rodríguez E, Soler MJ, Rap O, Barrios C, Orfila MA, Pascual J (2013) Risk factors for acute kidney injury in severe rhabdomyolysis. PLoS One 8:e82992
Wu CT, Huang JL, Lin JJ, Hsia SH (2009) Factors associated with nontraumatic rhabdomyolysis and acute renal failure of children in Taiwan population. Pediatr Emerg Care 25:657–660
Watanabe T (2001) Rhabdomyolysis and acute renal failure in children. Pediatr Nephrol 16:1072–1075
Zepeda-Orozco D, Ault BH, Jones DP (2008) Factors associated with acute renal failure in children with rhabdomyolysis. Pediatr Nephrol 23:2281–2284
Chen CY, Lin YR, Zhao LL, Yang WC, Chang YJ, Wu KH, Wu HP (2013) Clinical spectrum of rhabdomyolysis presented to pediatric emergency department. BMC Pediatr 13:134
Lim YS, Cho H, Lee ST, Lee Y (2018) Acute kidney injury in pediatric patients with rhabdomyolysis. Korean J Pediatr 61:95–100
Cervellin G, Comelli I, Benatti M, Sanchis-Gomar F, Bassi A, Lippi G (2017) Non-traumatic rhabdomyolysis: background, laboratory features, and acute clinical management. Clin Biochem 50:656–662
Acute Kidney Injury Work Group (2012) Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2:1–138
Piepsz A, Tondeur M, Ham H (2006) Revisiting normal (51)Cr-ethylenediaminetetraacetic acid clearance values in children. Eur J Nucl Med Mol Imaging 33:1477–1482
Hessey E, Ali R, Dorais M, Morissette G, Pizzi M, Rink N, Jouvet P, Lacroix J, Phan V, Zappitelli M (2017) Evaluation of height-dependent and height-independent methods of estimating baseline serum creatinine in critically ill children. Pediatr Nephrol 32:1953–1962
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Hoste L, Dubourg L, Selistre L, De Souza VC, Ranchin B, Hadj-Aïssa A, Cochat P, Martens F, Pottel H (2014) A new equation to estimate the glomerular filtration rate in children, adolescents and young adults. Nephrol Dial Transplant 29:1082–1091
Bosch X, Poch E, Grau JM (2009) Rhabdomyolysis and acute kidney injury. N Engl J Med 361:62–72
Mannix R, Tan ML, Wright R, Baskin M (2006) Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics 118:2119–2125
You J, Lee J, Park Y, Lee J (2017) Virus-associated rhabdomyolysis in children. Child Kidney Dis 21:89–93
Wu CT, Hsia SH, Huang JL (2010) Influenza B-associated rhabdomyolysis in Taiwanese children. Acta Paediatr 99:1701–1704
Goebel J, Harter HR, Boineau FG, El-Dahr SS (1997) Acute renal failure from rhabdomyolysis following influenza A in a child. Clin Pediatr (Phila) 36:479–481
Ishiwada N, Takada N, Okunushi T, Hishiki H, Katano H, Nakajima N, Kohno Y (2012) Rhabdomyolysis associated with influenza A/H1N1 2009 infection in a pediatric patient. Pediatr Int 54:703–705
Hui WF, Chan WK, Miu TY (2013) Acute kidney injury in the paediatric intensive care unit: identification by modified RIFLE criteria. Hong Kong Med J 19:13–19
Goldstein SL, Jaber BL, Faubel S, Chawla LS (2013) AKI transition of care: a potential opportunity to detect and prevent CKD. Clin J Am Soc Nephrol 8:476–483
Gelbart B, DeMarco R, David Hussey A, Namachivayam SP, McRae R, Quinlan C, Duke T (2018) Rhabdomyolysis in a tertiary PICU: a 10-year study. Pediatr Crit Care Med 19:e51–e57
Riley LK, Rupert J (2015) Evaluation of patients with leukocytosis. Am Fam Physician 92:1004–1011
Aydogan M, Aydogan A, Kara B, Basim B, Erdogan S (2007) Transient peripheral leukocytosis in children with afebrile seizures. J Child Neurol 22:77–79
Celkan T, Koç B (2015) Approach to the patient with neutropenia in childhood. Turk Pediatri Ars 50:136–144
Candela N, Silva S, Georges B, Cartery C, Robert T, Moussi-Frances J, Rondeau E, Rebibou JM, Lavayssiere L, Belliere J, Krummel T, Lebas C, Cointault O, Sallee M, Faguer S (2020) Short- and long-term renal outcomes following severe rhabdomyolysis: a French multicenter retrospective study of 387 patients. Ann Intensive Care 10:27
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Research Ethics Committee (Kowloon Central/Kowloon East Cluster), Hospital Authority, Hong Kong (Reference: KC/KE-19-0035/ER-3).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuok, C.I., Chan, W.K.Y. Acute kidney injury in pediatric non-traumatic rhabdomyolysis. Pediatr Nephrol 36, 3251–3257 (2021). https://doi.org/10.1007/s00467-021-05057-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05057-0