Abstract
Background
Endoscopic drainage has become the preferred treatment for pancreatic fluid collections (PFCs). There is still a lack of reliable evidence to prove which metal stent is the best choice for endoscopic ultrasound (EUS)-guided drainage of PFCs. In this study, we aimed to evaluate the efficacy and safety of lumen-apposing metal stents (LAMS) compared to traditional self-expanding metal stents (SEMS) in meta-analysis.
Methods
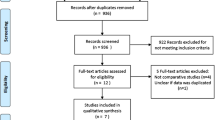
We systematically searched PubMed, Embase, Web of Science, and Cochrane Library up to July 15, 2023. Relevant publications that compared LAMS with traditional SEMS for drainage of patients’ PFCs under EUS-guidance were included. This meta-analysis assessed endpoints using Review Manager 5.3 and Stata 14.0 statistical software.
Result
Nine citations comprising 707 patients with PFCs were included. The clinical success rate of LAMS tended to be higher than that of SEMS (RR = 1.07, 95%CI [1.00, 1.15], P = 0.05). LAMS had a lower technical success rate (RR = 0.97, 95%CI [0.94, 0.99], P = 0.02) and faster procedure time (minutes) (MD = − 24.29, 95%CI [− 25.59, − 22.99], P < 0.00001) compared to SEMS. In addition, LAMS had fewer overall adverse events (RR = 0.64, 95%CI [0.48, 0.87], P = 0.004). For specific adverse events, LAMS had fewer migration (RR = 0.37, 95%CI [0.19, 0.72], P = 0.003), occlusion (RR = 0.43, 95%CI [0.22, 0.82], P = 0.01) and infection (RR = 0.38, 95%CI [0.20, 0.70], P = 0.002). There was no significant difference in bleeding and perforation between the two stents. For hospital stay (days), LAMS group was similar to SEMS group (MD = − 3.34, 95%CI [− 7.71, − 1.03], P = 0.13). Regarding recurrence, LAMS group was fewer than SEMS group (RR = 0.41, 95%CI [0.21, 0.78], P = 0.007).
Conclusion
Compared to traditional SEMS, LAMS has a higher clinical success rate, faster procedure time, fewer adverse events, similar hospital stay and lower recurrence rate in EUS-guided drainage of PFCs. LAMS is a good choice with a high technical success rate over 95%, and using a shorter length or “one-step” operation can further improve it. Richer placement experience is required for LAMS placement under EUS-guidance.






Similar content being viewed by others
References
Sarr MG (2013) 2012 revision of the Atlanta classification of acute pancreatitis. Pol Arch Med Wewn 123(3):118–124. https://doi.org/10.20452/pamw.1627
Molla NW, Alsergani AH, Alyamani AA et al (2022) Incidence of peripancreatic fluid collections in patients presenting with acute pancreatitis. Saudi Med J 43(12):1341–1346. https://doi.org/10.15537/smj.2022.43.12.20220508
Tsiotos GG, Sarr MG (1999) Management of fluid collections and necrosis in acute pancreatitis. Curr Gastroenterol Rep 1(2):139–144. https://doi.org/10.1007/s11894-996-0013-9
Baron TH, DiMaio CJ, Wang AY et al (2020) American gastroenterological association clinical practice update: management of pancreatic necrosis. Gastroenterology 158(1):67–75. https://doi.org/10.1053/j.gastro.2019.07.064
Chawla A, Afridi F, Prasath V et al (2023) Analysis of pancreatic pseudocyst drainage procedural outcomes: a population based study. Surg Endosc 37(1):156–164. https://doi.org/10.1007/s00464-022-09427-z
Mack S, Galasso D, Marx M et al (2023) Efficacy and safety of endoscopic ultrasound guided drainage of pseudocysts and walled-off necrosis after failure of percutaneous drainage. Surg Endosc 37(4):2626–2632. https://doi.org/10.1007/s00464-022-09741-6
Fogwe DT, AbiMansour JP, Truty MJ et al (2023) Endoscopic ultrasound-guided versus percutaneous drainage for the management of post-operative fluid collections after distal pancreatectomy. Surg Endosc. https://doi.org/10.1007/s00464-023-10188-6
Pereira F, Caldeira A, Leite S et al (2020) GRUPUGE perspective: endoscopic ultrasound-guided drainage of peripancreatic collections. GE Port J Gastroenterol 28(1):39–51. https://doi.org/10.1159/000509193
Wan J, Wu D, He W et al (2020) Comparison of percutaneous vs endoscopic drainage in the management of pancreatic fluid collections: a prospective cohort study. J Gastroenterol Hepatol 35(12):2170–2175. https://doi.org/10.1111/jgh.15121
Li J, Yu Y, Li P et al (2020) Advancements in the endoscopic treatment of pancreatic fluid collections. Chronic Dis Transl Med 6(3):158–164. https://doi.org/10.1016/j.cdtm.2020.03.001
Saunders R, Ramesh J, Cicconi S et al (2019) A systematic review and meta-analysis of metal versus plastic stents for drainage of pancreatic fluid collections: metal stents are advantageous. Surg Endosc 33(5):1412–1425. https://doi.org/10.1007/s00464-018-6416-5
Panwar R, Singh PM (2017) Efficacy and safety of metallic stents in comparison to plastic stents for endoscopic drainage of peripancreatic fluid collections: a meta-analysis and trial sequential analysis. Clin J Gastroenterol 10(5):403–414. https://doi.org/10.1007/s12328-017-0763-y
Lyu Y, Li T, Wang B et al (2021) Comparison between lumen-apposing metal stents and plastic stents in endoscopic ultrasound-guided drainage of pancreatic fluid collection: a meta-analysis and systematic review. Pancreas 50(4):571–578. https://doi.org/10.1097/MPA.0000000000001798
Guzmán-Calderón E, Chacaltana A, Díaz R et al (2022) Head-to-head comparison between endoscopic ultrasound guided lumen apposing metal stent and plastic stents for the treatment of pancreatic fluid collections: a systematic review and meta-analysis. J Hepatobiliary Pancreat Sci 29(2):198–211. https://doi.org/10.1002/jhbp.1008
Chen YI, Yang J, Friedland S et al (2019) Lumen apposing metal stents are superior to plastic stents in pancreatic walled-off necrosis: a large international multicenter study. Endosc Int Open 7(3):E347–E354. https://doi.org/10.1055/a-0828-7630
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Luo D, Wan X, Liu J et al (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805. https://doi.org/10.1177/0962280216669183
Wan X, Wang W, Liu J et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Bekkali N, Nayar MK, Leeds JS et al (2017) A comparison of outcomes between a lumen-apposing metal stent with electrocautery-enhanced delivery system and a bi-flanged metal stent for drainage of walled-off pancreatic necrosis. Endosc Int Open 5(12):E1189–E1196. https://doi.org/10.1055/s-0043-120831
Siddiqui A, Naveed M, Basha J et al (2021) International, multicenter retrospective trial comparing the efficacy and safety of bi-flanged versus lumen-apposing metal stents for endoscopic drainage of walled-off pancreatic necrosis. Ann Gastroenterol 34(2):273–281. https://doi.org/10.20524/aog.2021.0570
Dos Santos ME, Matsubayashi CO, Guedes HG et al (2020) Su1313 Comparison of migration rate of lumen-apposing metal stent and standard covered self-expanding metal stent for endoscopic ultrasound-guided pancreatic fluid collection drainage: a randomized controlled trial. Gastrointest Endosc 91(6, Supplement):B326–B327. https://doi.org/10.1016/j.gie.2020.03.2159
Shah RJ, Shah JN, Waxman I et al (2015) Safety and efficacy of endoscopic ultrasound-guided drainage of pancreatic fluid collections with lumen-apposing covered self-expanding metal stents. Clin Gastroenterol Hepatol 13(4):747–752. https://doi.org/10.1016/j.cgh.2014.09.047
Musumba C, Tutticci N, Nanda K et al (2014) Endosonography-guided drainage of malignant fluid collections using lumen-apposing, fully covered self-expanding metal stents. Endoscopy 46(8):690–692. https://doi.org/10.1055/s-0034-1365424
Drepper M, Pérez-Cuadrado-Robles E, Deprez PH (2019) EUS-guided drainage of peripancreatic fluid collections by lumen-apposing metal stents versus self-expanding metal stents versus plastic stents: single center experience over 6 years. Endoscopy 51(4):S186. https://doi.org/10.1055/s-0039-1681720
Falk V, Kenshil S, Sandha S et al (2020) The Evolution of EUS-guided transluminal drainage for the treatment of pancreatic fluid collections: a comparison of clinical and cost outcomes with double-pigtail plastic stents, conventional metal stents and lumen-apposing metal stents. J Can Assoc Gastroenterol 3(1):26–35. https://doi.org/10.1093/jcag/gwy049
Garcia GDPA, Gonzalez MJ, Foruny OJ et al (2020) Lumen-apposing metal stents versus biliary fully-covered metal stents for EUS-guided drainage of pancreatic fluid collections: a case control study: meeting presentations: European Society of Gastrointestinal Endoscopy ESGE Days 2018. Endosc Int Open 8(1):E6–E12. https://doi.org/10.1055/a-1031-9295
Jang S, Stevens T, Chahal P et al (2018) Comparative efficacy of lumen apposing metal stent versus fully covered self-expandable metallic stent in the managemnt of pancreatic fluid collection. Gastrointest Endosc 87(6):B394–B395
Kayal A, Taghizadeh N, Ishikawa T et al (2021) Endosonography-guided transmural drainage of pancreatic fluid collections: comparative outcomes by stent type. Surg Endosc 35(6):2698–2708. https://doi.org/10.1007/s00464-020-07699-x
Law ST, De La SernaHiguera C, Simón PG et al (2018) Comparison of clinical efficacies and safeties of lumen-apposing metal stent and conventional-type metal stent-assisted EUS-guided pancreatic wall-off necrosis drainage: a real-life experience in a tertiary hospital. Surg Endosc 32(5):2448–2453. https://doi.org/10.1007/s00464-017-5946-6
Lera DSM, Proença IM, de Moura D et al (2023) Self-expandable metal stent (SEMS) versus lumen-apposing metal stent (LAMS) for drainage of pancreatic fluid collections: a randomized clinical trial. Cureus 15(4):e37731. https://doi.org/10.7759/cureus.37731
Siddiqui AA, Kowalski TE, Loren DE et al (2017) Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: clinical outcomes and success. Gastrointest Endosc 85(4):758–765. https://doi.org/10.1016/j.gie.2016.08.014
Wang Z, Zhao S, Meng Q et al (2019) Comparison of three different stents for endoscopic ultrasound-guided drainage of pancreatic fluid collection: a large retrospective study. J Gastroenterol Hepatol 34(4):791–798. https://doi.org/10.1111/jgh.14557
Pfau PR, Pleskow DK, Banerjee S et al (2013) Pancreatic and biliary stents. Gastrointest Endosc 77(3):319–327. https://doi.org/10.1016/j.gie.2012.09.026
Chen Y, Barkun AN, Adam V et al (2018) Cost-effectiveness analysis comparing lumen-apposing metal stents with plastic stents in the management of pancreatic walled-off necrosis. Gastrointest Endosc 88(2):267–276. https://doi.org/10.1016/j.gie.2018.03.021
Mangiavillano B, Pagano N, Baron TH et al (2016) Biliary and pancreatic stenting: devices and insertion techniques in therapeutic endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography. World J Gastrointest Endosc 8(3):143–156. https://doi.org/10.4253/wjge.v8.i3.143
Yeoh KG, Zimmerman MJ, Cunningham JT et al (1999) Comparative costs of metal versus plastic biliary stent strategies for malignant obstructive jaundice by decision analysis. Gastrointest Endosc 49(4 Pt 1):466–471. https://doi.org/10.1016/s0016-5107(99)70044-1
Han S, Obando JV, Bhatt A et al (2023) Biliary and pancreatic stents. iGIE 2(2):240–253. https://doi.org/10.1016/j.gie.2023.03.016
Vaishnavi C, Samanta J, Kochhar R (2018) Characterization of biofilms in biliary stents and potential factors involved in occlusion. World J Gastroenterol 24(1):112–123. https://doi.org/10.3748/wjg.v24.i1.112
Sung JJ (1995) Bacterial biofilm and clogging of biliary stents. J Ind Microbiol 15(3):152–155. https://doi.org/10.1007/BF01569819
Neuhaus H, Hagenmüller F, Classen M (1989) Self-expanding biliary stents: preliminary clinical experience. Endoscopy 21(5):225–228. https://doi.org/10.1055/s-2007-1012954
Irving JD, Adam A, Dick R et al (1989) Gianturco expandable metallic biliary stents: results of a European clinical trial. Radiology 172(2):321–326. https://doi.org/10.1148/radiology.172.2.2664861
Lam R, Muniraj T (2021) Fully covered metal biliary stents: a review of the literature. World J Gastroenterol 27(38):6357–6373. https://doi.org/10.3748/wjg.v27.i38.6357
Bang JY, Varadarajulu S (2019) Lumen-apposing metal stents for endoscopic ultrasonography-guided interventions. Dig Endosc 31(6):619–626. https://doi.org/10.1111/den.13428
Mussetto A, Fugazza A, Fuccio L et al (2018) Current uses and outcomes of lumen-apposing metal stents. Ann Gastroenterol 31(5):535–540. https://doi.org/10.20524/aog.2018.0287
Saumoy M, Yarber C, Kahaleh M (2018) Novel uses of lumen-apposing metal stents. Gastrointest Endosc Clin N Am 28(2):197–205. https://doi.org/10.1016/j.giec.2017.11.007
Guo J, Saftoiu A, Vilmann P et al (2017) A multi-institutional consensus on how to perform endoscopic ultrasound-guided peri-pancreatic fluid collection drainage and endoscopic necrosectomy. Endosc Ultrasound 6(5):285–291. https://doi.org/10.4103/eus.eus_85_17
Itoi T, Binmoeller KF, Shah J et al (2012) Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc 75(4):870–876. https://doi.org/10.1016/j.gie.2011.10.020
Bang JY, Navaneethan U, Hasan MK et al (2019) Non-superiority of lumen-apposing metal stents over plastic stents for drainage of walled-off necrosis in a randomised trial. Gut 68(7):1200–1209. https://doi.org/10.1136/gutjnl-2017-315335
Park CH, Park SW, Nam E et al (2020) Comparative efficacy of stents in endoscopic ultrasonography-guided peripancreatic fluid collection drainage: a systematic review and network meta-analysis. J Gastroenterol Hepatol 35(6):941–952. https://doi.org/10.1111/jgh.14960
Han D, Inamdar S, Lee CW et al (2018) Lumen apposing metal stents (LAMSs) for drainage of pancreatic and gallbladder collections: a meta-analysis. J Clin Gastroenterol 52(9):835–844. https://doi.org/10.1097/MCG.0000000000000934
Yoo J, Yan L, Hasan R et al (2017) Feasibility, safety, and outcomes of a single-step endoscopic ultrasonography-guided drainage of pancreatic fluid collections without fluoroscopy using a novel electrocautery-enhanced lumen-apposing, self-expanding metal stent. Endosc Ultrasound 6(2):131–135. https://doi.org/10.4103/2303-9027.204814
Armellini E, Metelli F, Anderloni A et al (2023) Lumen-apposing-metal stent misdeployment in endoscopic ultrasound-guided drainages: a systematic review focusing on issues and rescue management. World J Gastroenterol 29(21):3341–3361. https://doi.org/10.3748/wjg.v29.i21.3341
Luthra AK, Garner Z, Krishna SG (2020) International multicenter comprehensive analysis of adverse events associated with lumen-apposing metal stent placement for pancreatic fluid collection drainage. Gastrointest Endosc 92(4):980. https://doi.org/10.1016/j.gie.2020.05.008
van Brunschot S, van Grinsven J, van Santvoort HC et al (2018) Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial. Lancet 391(10115):51–58. https://doi.org/10.1016/S0140-6736(17)32404-2
Arvanitakis M, Dumonceau JM, Albert J et al (2018) Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines. Endoscopy 50(5):524–546. https://doi.org/10.1055/a-0588-5365
Ramai D, Enofe I, Deliwala SS et al (2023) Early (<4 weeks) versus standard (≥4 weeks) endoscopic drainage of pancreatic walled-off fluid collections: a systematic review and meta-analysis. Gastrointest Endosc 97(3):415–421. https://doi.org/10.1016/j.gie.2022.11.003
Bang JY, Wilcox CM, Trevino J et al (2013) Factors impacting treatment outcomes in the endoscopic management of walled-off pancreatic necrosis. J Gastroenterol Hepatol 28(11):1725–1732. https://doi.org/10.1111/jgh.12328
Ross AS, Irani S, Gan SI et al (2014) Dual-modality drainage of infected and symptomatic walled-off pancreatic necrosis: long-term clinical outcomes. Gastrointest Endosc 79(6):929–935. https://doi.org/10.1016/j.gie.2013.10.014
Puli SR, Graumlich JF, Pamulaparthy SR et al (2014) Endoscopic transmural necrosectomy for walled-off pancreatic necrosis: a systematic review and meta-analysis. Can J Gastroenterol Hepatol 28(1):50–53. https://doi.org/10.1155/2014/539783
Funding
This research was funded by Sichuan Provincial Science and Technology Department, grant number 2021YJ0198, Sichuan Medical Association, Grant Number 2021XHNJ19, and XingLin Scholars Program of Chengdu University of TCM, Grant Number YYZX2020036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yong Tian, Changjie Yin, Yihan Ma, Guochuan Fu, Rui Liu, Hongmei Ran, Tao Pan, Yang Xiao, Xudong Wen have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was exempt from ethics review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tian, Y., Yin, C., Ma, Y. et al. Lumen-apposing metal stents versus traditional self-expanding metal stents for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a systematic review and meta-analysis. Surg Endosc 38, 586–596 (2024). https://doi.org/10.1007/s00464-023-10636-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10636-3