Abstract
Background and aim
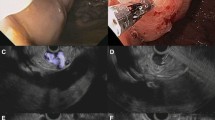
First, it has been demonstrated that endoscopic ultrasonography (EUS)-guided cyanoacrylate (CYA) injection (EUS-CYA) has greater efficacy than direct endoscopic injection of cyanoacrylate (DEI-CYA) for treating type 1-isolated gastric varices. However, it is necessary to conduct further studies to determine whether EUS has any advantage over the current guidelines for treating gastroesophageal varices type 1 (GOV1). Second, liver function is an important prognostic factor in patients with liver cirrhosis. Therefore, we evaluated the liver function of patients treated with EUS-CYA.
Methods
In a single-center study, a prospective cohort from February 2021 to September 2022 involving 89 patients with cirrhosis with GOV1 were assigned to undergo EUS-CYA (n = 45) or DEI-CYA (n = 44). The success rate of CYA injection, the rate of overall rebleeding, the rate of reintervention, the complications during the follow-up period, and the liver function were compared.
Results
In both groups, 100% of the operations were successful. The follow-up time of the two groups was 290 (153–398) days and 267 (177–416) days, respectively. In the EUS group, the perforating veins had an average diameter of 7.0 ± 2.7 mm, and they had a 100% occlusion rate. A statistically significant difference was found between the two groups regarding the number of sessions needed to eradicate GV (p = 0.005, pairwise comparisons were conducted using the Bonferroni correction method.), the late rebleeding rate after EUS-CYA [n = 3 (6.7%) vs n = 10 (22.7%); p = 0.032], and the incidence of postinjection ulcers [n = 4 (8.9%) vs n = 12 (27.3); p = 0.023)]. Following EUS or DEI-CYA treatment, the patient’s liver function did not show any significant deterioration or decline.
Conclusion
EUS-CYA has a higher eradication success rate and fewer complications, recurrences, and rebleeding episodes than DEI-CYA used for GOV1 treatment. In addition, EUS-CYA did not impair liver function.





Similar content being viewed by others
References
Franco MC (2014) Efficacy and safety of endoscopic prophylactic treatment with undiluted cyanoacrylate for gastric varices. World J Gastrointest Endosc 6(6):254
De Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C, Abraldes JG, Albillos A, Baiges A, Bajaj J, Bañares R, Barrufet M (2022) Baveno VII—renewing consensus in portal hypertension. J Hepatol 76(4):959–974
Thiruvengadam SS, Sedarat A (2021) The role of endoscopic ultrasound (EUS) in the management of gastric varices. Curr Gastroenterol Rep. https://doi.org/10.1007/s11894-020-00801-2
McCarty TR, Bazarbashi AN, Hathorn KE (2020) Combination therapy versus monotherapy for EUS-guided management of gastric varices: a systematic review and meta-analysis. Endosc Ultrasound 9(1):6–15
Baig M, Ramchandani M, Puli SR (2022) Safety and efficacy of endoscopic ultrasound-guided combination therapy for treatment of gastric varices: a systematic review and meta-analysis. Clin J Gastroenterol 15(2):310–319
Bick BL et al (2019) EUS-guided fine needle injection is superior to direct endoscopic injection of 2-octyl cyanoacrylate for the treatment of gastric variceal bleeding. Surg Endosc 33(6):1837–1845
Bertroli JA, Abadia MA, Peracaula MM (2011) Preliminary experience with EUS-guided treatment of acute gastric varices bleeding using a forward-viewing echoendoscope. Gastrointest Endosc 73:179
Mohan BP et al (2020) Efficacy and safety of endoscopic ultrasound-guided therapy versus direct endoscopic glue injection therapy for gastric varices: systematic review and meta-analysis. Endoscopy 52(4):259–267
Tamaki N, Kurosaki M, Matsuda S (2014) Non-invasive prediction of hepatocellular carcinoma development using serum fibrosis marker in chronic hepatitis C patients. J Gastroenterol 49(11):1495–1503
Hayashi T et al (2021) Endoscopic injection sclerotherapy improves liver function compared with endoscopic variceal ligation. Sci Rep 11(1):20479
Sarin SK et al (1992) Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology 16(6):1343–1349
Lee YT et al (2000) EUS-guided injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc 52(2):168–174
Soehendra N, Nam VC, Grimm H (1986) Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy 18(1):25–26
de Franchis R (2015) Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 63:743–752
Castellanos ER, Seron P, Gisbert JP (2015) Endoscopic injection of cyanoacrylate glue versus other endoscopic procedures for acute bleeding gastric varices in people with portal hypertension. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010180.pub2
Qiao W, Ren Y, Bai Y (2015) Cyanoacrylate injection versus band ligation in the endoscopic management of acute gastric variceal bleeding. Medicine (Baltimore) 94(41):e1725
Romero-Castro R et al (2007) EUS-guided injection of cyanoacrylate in perforating feeding veins in gastric varices: results in 5 cases. Gastrointest Endosc 66(2):402–407
Bazarbashi AN et al (2020) Endoscopic ultrasound-guided coil embolization with absorbable gelatin sponge appears superior to traditional cyanoacrylate injection for the treatment of gastric varices. Clin Transl Gastroenterol 11(5):e00175
Ma L et al (2019) Risk stratification for secondary prophylaxis of gastric varices due to portal hypertension. Dig Liver Dis 51(12):1678–1684
Lôbo MRDA et al (2019) Safety and efficacy of EUS-guided coil plus cyanoacrylate versus conventional cyanoacrylate technique in the treatment of gastric varices: a randomized controlled trial. Arquivos Gastroenterol 56(1):99–105
Boustière C et al (1993) Endoscopic ultrasonography classification of gastric varices in patients with cirrhosis. Comparison with endoscopic findings. J Hepatol 19(2):268
Iwase H, Suga S, Morise K (1995) Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc 41(2):150–154
Kobayashi M, Suzuki M, Ikeda H (2009) Assessment of hepatic steatosis and hepatic tissue blood flow by xenon computed tomography in nonalcoholic steatohepatitis. Hepatol Res 39(1):31–39
Acknowledgements
The author thanks Jiangrui Cheng for his contribution in the statistical portion of this paper and appreciates Xianfu Lu’s contribution in the field of anesthesia.
Funding
The sixth batch of health and appropriate technology promotion projects in Anhui Province, new technology of comprehensive diagnosis and treatment of esophagogastric varices under endoscopy (SYJS202103); NSF Project, MAIT Cells induce neutrophil aging through gut microbiota. A novel mechanism for the progression of alcoholic liver disease (82270623).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Zhihong Wang, Zhuang Zeng, Lihong Chen, Chen Shi, Jing Jin, Fumin Zhang, Qianqian Zhang, Xuecan Mei, and Derun Kong have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Zeng, Z., Chen, L. et al. Endoscopic ultrasonography-guided injection of cyanoacrylate in the treatment of gastroesophageal varices type 1: a single-center randomized study. Surg Endosc 37, 8277–8284 (2023). https://doi.org/10.1007/s00464-023-10342-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10342-0