Abstract
Background
Morphology of the major duodenal papilla (MDP) influences the outcome of standard biliary cannulation. However, those data on advanced cannulation techniques are scarce. We aimed to study the impact of MDP morphology on the outcome of both standard and advanced cannulation methods.
Methods
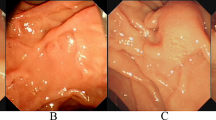
Images of naïve papilla were retrospectively reviewed and independently classified into 4 types (1: classic appearance, 2: small, 3: bulging, and 4: ridged papillae). All cannulation was started with guidewire cannulation. After failure, advanced cannulation including double guidewire (DG) and/or precut sphincterotomy (PS) was performed. Outcomes including success rate and complications were analyzed.
Results
A total 805 naïve papilla were included. The overall advanced cannulation rate was 23.2%. The MPD type 2 (OR 1.8, 95% CI 1.8–2.9) and type 4 (OR 2.1, 95% CI 1.1–3.8) required advanced cannulation technique at a higher rate than type 1. Type 3 significantly needed a higher proportion of PS when compared with type 1 (59.09% vs 27.03%, OR 3.90, 95% CI 1.51–10.06). Overall post-ERCP pancreatitis (PEP) was 8% and was not different among MDP types. PEP was significantly increased in difficult cannulation group (15.38% vs 5.71%, p-value < 0.001). Multivariate analysis demonstrated that DG independently increased risk of PEP (OR 3.6, 95% CI 2.0–6.6).
Conclusions
MDP type 2 and type 4 were related to difficult cannulation. Although DG and PS can be used as advanced cannulation in all types, DG carries risk of PEP and PS may be preferred over DG in MDP type 3.
Graphical abstract





Similar content being viewed by others
References
Peng C, Nietert PJ, Cotton PB, Lackland DT, Romagnuolo J (2013) Predicting native papilla biliary cannulation success using a multinational Endoscopic Retrograde Cholangiopancreatography (ERCP) Quality Network. BMC Gastroenterol 13:147
Bakman YG, Freeman ML (2013) Difficult biliary access at ERCP. Gastrointest Endosc Clin N Am 23:219–236
Haraldsson E, Lundell L, Swahn F, Enochsson L, Löhr JM, Arnelo U (2017) Endoscopic classification of the papilla of Vater. Results of an inter- and intraobserver agreement study. United Eur Gastroenterol J 5:504–510
Silvis SE, Vennes JA, Dreyer M (1983) Variations in the normal duodenal papilla. Gastrointest Endosc 29:132–133
Horiuchi A, Nakayama Y, Kajiyama M, Tanaka N (2007) Effect of precut sphincterotomy on biliary cannulation based on the characteristics of the major duodenal papilla. Clin Gastroenterol Hepatol 5:1113–1118
Haraldsson E, Kylänpää L, Grönroos J, Saarela A, Toth E, Qvigstad G, Hult M, Lindström O, Laine S, Karjula H, Hauge T, Sadik R, Arnelo U (2019) Macroscopic appearance of the major duodenal papilla influences bile duct cannulation: a prospective multicenter study by the Scandinavian Association for Digestive Endoscopy Study Group for ERCP. Gastrointest Endosc 90:957–963
Liao WC, Angsuwatcharakon P, Isayama H, Dhir V, Devereaux B, Khor CJ, Ponnudurai R, Lakhtakia S, Lee DK, Ratanachu-Ek T, Yasuda I, Dy FT, Ho SH, Makmun D, Liang HL, Draganov PV, Rerknimitr R, Wang HP (2017) International consensus recommendations for difficult biliary access. Gastrointest Endosc 85:295–304
Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Deviere J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ (2016) Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 48:657–683
Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP Jr, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW, Van Dam J, Hughes M, Carr-Locke DL (2002) Risk factors for complications after performance of ERCP. Gastrointest Endosc 56:652–656
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102:1781–1788
Elmunzer BJ (2017) Reducing the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis. Digest. Endosc 29:749–757
Halttunen J, Meisner S, Aabakken L, Arnelo U, Grönroos J, Hauge T, Kleveland PM, Nordblad Schmidt P, Saarela A, Swahn F, Toth E, Mustonen H, Löhr JM (2014) Difficult cannulation as defined by a prospective study of the Scandinavian Association for Digestive Endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol 49:752–758
Angsuwatcharakon P, Rerknimitr R, Ridtitid W, Ponauthai Y, Kullavanijaya P (2012) Success rate and cannulation time between precut sphincterotomy and double-guidewire technique in truly difficult biliary cannulation. J Gastroenterol Hepatol 27:356–361
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA (2006) Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutaneous Tech 16:208–211
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Tabak F, Wang HS, Li QP, Ge XX, Wang F, Ji GZ, Miao L (2020) Endoscopic retrograde cholangiopancreatography in elderly patients: Difficult cannulation and adverse events. World J Clin Cases 8:2988–2999
Zheng H, Yan S, Li D, Xue Y, Deng X (2021) Influence of periampullary diverticula on endoscopic retrograde cholangiopancreatography. Exp Ther Med 21:410–410
Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S (2008) Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointest Endosc 68:903–910
Tse F, Yuan Y, Moayyedi P, Leontiadis GI, Barkun AN (2017) Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 49:15–26
Acknowledgements
This project was funded by National Research Council of Thailand (NRCT): N42A640330 and support by Center of Excellence for Innovation and Endoscopy in Gastrointestinal Oncology.
Author information
Authors and Affiliations
Contributions
PA and CT were involved in study design, data analysis, and drafting of manuscript. PA, CT, WR, PP, SK, PK were involved in data collection. PA, CT, WR, PP, SK, PK, and RR were involved in editing and final approval of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Drs. Phonthep Angsuwatcharakon, Chompoonuch Thongsuwan, Wiriyaporn Ridtitid, Panida Piyachaturawat, Santi Kulpatcharapong, Pradermchai Kongkam, and Rungsun Rerknimitr have no conflicts of interest or financial ties to disclose. This work was presented in part at the Digestive Disease Week, May 21, 2021.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Angsuwatcharakon, P., Thongsuwan, C., Ridtitid, W. et al. Morphology of the major duodenal papilla for the selection of advanced cannulation techniques in difficult biliary cannulation. Surg Endosc 37, 5807–5815 (2023). https://doi.org/10.1007/s00464-023-10058-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10058-1