Abstract
Backgrounds
Esophageal gastrointestinal stromal tumors (E-GISTs) are extremely rare and surgical resection is the recommended approach. However, surgical resection usually causes severe trauma that may result in significant postoperative morbidity. Endoscopic resection (ER) has developed rapidly in recent years and has been widely used in gastrointestinal lesions. Nevertheless, the feasibility and efficacy of ER in the management of E-GISTs are unknown.
Methods
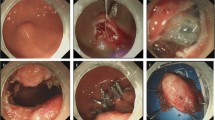
Retrospective data were collected from January 2011 to December 2020 in a large tertiary center of China. Twenty-eight patients with E-GISTs treated by ER were included in the study.
Results
Of the 28 patients, there were 21 males and 7 females, with a median age of 55 years (40–70 years). The median tumor size was 15 mm (5–80 mm). The technical success rate was 100% (28/28), while the en bloc resection rate was 96.4% (27/28). The median operation time was 35 min (10–410 min). Sixteen (57.2%) tumors were categorized into very low risk group, six (21.4%) into low risk group, and six (21.4%) into high risk group. Pathologists carefully examined margins of each lesion. There were 11 lesions (39.3%) determined as R0 resection and 17 lesions (60.7%) as R1 resection with positive margins. The median hospital stay was 2 days (range, 1–8 days). One patient suffered from hydrothorax and required drainage, leading to a major adverse event rate of 3.6% (1/28). There was no conversion to surgery, and no death occurred within 30 days after the procedure. Imatinib was given to two patients after ER under multidisciplinary team surveillance. During follow-up (median of 54 months, 9–122 months), no recurrences or metastasis were observed.
Conclusion
ER is safe and effective for E-GISTs and might become an optional choice in the future. Multicenter, prospective, large samples with long-term follow-up studies are still needed.




Similar content being viewed by others
Abbreviations
- GIST:
-
Gastrointestinal stromal tumor
- ESD:
-
Endoscopic submucosal dissection
- EFTR:
-
Endoscopic full-thickness resection
- HPF:
-
High power field
- GI:
-
Gastrointestinal
- NCCN:
-
National comprehensive cancer network
References
Corless CL, Barnett CM, Heinrich MC (2011) Gastrointestinal stromal tumours: origin and molecular oncology. Nat Rev Cancer 11:865–878. https://doi.org/10.1038/nrc3143
Fletcher CDM, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP, Shmookler B, Sobin LH, Weiss SW (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol 10:81–89. https://doi.org/10.1177/106689690201000201
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PWT, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN task force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. https://doi.org/10.6004/jnccn.2010.0116
Monges G, Bisot-Locard S, Blay J-Y, Bouvier A-M, Urbieta M, Coindre J-M, Scoazec J-Y (2010) The estimated incidence of gastrointestinal stromal tumors in France. Results of PROGIST study conducted among pathologists. Bull Cancer 97:E16-22. https://doi.org/10.1684/bdc.2010.1041
Lott S, Schmieder M, Mayer B, Henne-Bruns D, Knippschild U, Agaimy A, Schwab M, Kramer K (2015) Gastrointestinal stromal tumors of the esophagus: evaluation of a pooled case series regarding clinicopathological features and clinical outcome. Am J Cancer Res 5:333–343
Koo D-H, Ryu M-H, Kim K-M, Yang H-K, Sawaki A, Hirota S, Zheng J, Zhang B, Tzen C-Y, Yeh C-N, Nishida T, Shen L, Chen L-T, Kang Y-K (2016) Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat 48:1155–1166. https://doi.org/10.4143/crt.2016.187
Casali PG, Abecassis N, Aro HT, Bauer S, Biagini R, Bielack S, Bonvalot S, Boukovinas I, Bovee JVMG, Brodowicz T, Broto JM, Buonadonna A, De Álava E, Dei Tos AP, Del Muro XG, Dileo P, Eriksson M, Fedenko A, Ferraresi V, Ferrari A, Ferrari S, Frezza AM, Gasperoni S, Gelderblom H, Gil T, Grignani G, Gronchi A, Haas RL, Hassan B, Hohenberger P, Issels R, Joensuu H, Jones RL, Judson I, Jutte P, Kaal S, Kasper B, Kopeckova K, Krákorová DA, Le Cesne A, Lugowska I, Merimsky O, Montemurro M, Pantaleo MA, Piana R, Picci P, Piperno-Neumann S, Pousa AL, Reichardt P, Robinson MH, Rutkowski P, Safwat AA, Schöffski P, Sleijfer S, Stacchiotti S, Sundby Hall K, Unk M, Van Coevorden F, van der Graaf WTA, Whelan J, Wardelmann E, Zaikova O, Blay JY, Guidelines Committee ESMO, EURACAN, (2018) Gastrointestinal stromal tumours: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 29:iv68–iv78. https://doi.org/10.1093/annonc/mdy095
von Mehren M, Randall RL, Benjamin RS, Boles S, Bui MM, Ganjoo KN, George S, Gonzalez RJ, Heslin MJ, Kane JM, Keedy V, Kim E, Koon H, Mayerson J, McCarter M, McGarry SV, Meyer C, Morris ZS, O’Donnell RJ, Pappo AS, Paz IB, Petersen IA, Pfeifer JD, Riedel RF, Ruo B, Schuetze S, Tap WD, Wayne JD, Bergman MA, Scavone JL (2018) Soft tissue sarcoma, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 16:536–563. https://doi.org/10.6004/jnccn.2018.0025
An W, Sun P-B, Gao J, Jiang F, Liu F, Chen J, Wang D, Li Z-S, Shi X-G (2017) Endoscopic submucosal dissection for gastric gastrointestinal stromal tumors: a retrospective cohort study. Surg Endosc 31:4522–4531. https://doi.org/10.1007/s00464-017-5511-3
Andalib I, Yeoun D, Reddy R, Xie S, Iqbal S (2018) Endoscopic resection of gastric gastrointestinal stromal tumors originating from the muscularis propria layer in North America: methods and feasibility data. Surg Endosc 32:1787–1792. https://doi.org/10.1007/s00464-017-5862-9
Huang J, Xian X-S, Huang L-Y, Zhang B, Wu C-R (1992) Cui J (2018) Endoscopic full-thickness resection for gastric gastrointestinal stromal tumor originating from the muscularis propria. Rev Assoc Med Bras 64:1002–1006. https://doi.org/10.1590/1806-9282.64.11.1002
Shichijo S, Uedo N, Yanagimoto Y, Yamamoto K, Kono M, Fukuda H, Shimamoto Y, Nakagawa K, Ohmori M, Arao M, Iwatsubo T, Iwagami H, Inoue S, Matsuno K, Matsuura N, Nakahira H, Maekawa A, Kanesaka T, Takeuchi Y, Higashino K, Ohmori T, Ishihara R (2019) Endoscopic full-thickness resection of gastric gastrointestinal stromal tumor: a Japanese case series. Ann Gastroenterol 32:593–599. https://doi.org/10.20524/aog.2019.0413
Tian X, Shi B, Chen W-Q (2020) Modified endoscopic full-thickness resection of gastric stromal tumor originating from the muscularis propria layer. J Gastrointest Oncol 11:461–466. https://doi.org/10.21037/jgo.2020.03.12
Zhou Y, Zheng S, Sun M, Li Q (2020) Diagnosis and endoscopic treatment of gastrointestinal stromal tumors arising from esophagus. J Laparoendosc Adv Surg Tech A 30:759–763. https://doi.org/10.1089/lap.2019.0792
Xu M-D, Cai M-Y, Zhou P-H, Qin X-Y, Zhong Y-S, Chen W-F, Hu J-W, Zhang Y-Q, Ma L-L, Qin W-Z, Yao L-Q (2012) Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc 75:195–199. https://doi.org/10.1016/j.gie.2011.08.018
Shi Q, Zhong Y-S, Yao L, Zhou P, Xu M, Wang P (2011) Endoscopic submucosal dissection for treatment of esophageal submucosal tumors originating from the muscularis propria layer. Gastrointest Endosc 74:1194–1200. https://doi.org/10.1016/j.gie.2011.07.039
Zhou P-H, Yao L-Q, Qin X-Y, Cai M-Y, Xu M-D, Zhong Y-S, Chen W-F, Zhang Y-Q, Qin W-Z, Hu J-W, Liu J-Z (2011) Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surg Endosc 25:2926–2931. https://doi.org/10.1007/s00464-011-1644-y
Zhang Y, Yao L, Xu M, Berzin TM, Li Q, Chen W, Hu J, Wang Y, Cai M, Qin W, Xu J, Huang Y, Zhou P (2017) Treatment of leakage via metallic stents placements after endoscopic full-thickness resection for esophageal and gastroesophageal junction submucosal tumors. Scand J Gastroenterol 52:76–80. https://doi.org/10.1080/00365521.2016.1228121
Joensuu H (2008) Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol 39:1411–1419. https://doi.org/10.1016/j.humpath.2008.06.025
Robb WB, Bruyere E, Amielh D, Vinatier E, Mabrut JY, Perniceni T, Piessen G, Mariette C, FREGAT Working Group-FRENCH (2015) Esophageal gastrointestinal stromal tumor: is tumoral enucleation a viable therapeutic option? Ann Surg 261:117–124. https://doi.org/10.1097/SLA.0000000000000505
Huang C-S, Hsu W-H, Wu Y-C, Chau G-Y, Tsay S-H, Huang M-H (2006) Enucleation of an advanced esophageal gastrointestinal stromal tumor with liver metastasis. J Gastroenterol Hepatol 21:482–483. https://doi.org/10.1111/j.1440-1746.2006.04106.x
Yamada H, Shinohara T, Yokoyama K, Takasu K, Fujimori Y, Yamagishi K (2011) Thoracoscopic enucleation of esophageal gastrointestinal stromal tumor using prone positioning in a patient with severe chronic obstructive lung disease. J Laparoendosc Adv Surg Tech A 21:635–639. https://doi.org/10.1089/lap.2011.0264
Liu S, Zhou X, Yao Y, Shi K, Yu M, Ji F (2020) Resection of the gastric submucosal tumor (G-SMT) originating from the muscularis propria layer: comparison of efficacy, patients’ tolerability, and clinical outcomes between endoscopic full-thickness resection and surgical resection. Surg Endosc 34:4053–4064. https://doi.org/10.1007/s00464-019-07311-x
Zhang F-B, Shi H-C, Shu Y-S, Shi W-P, Lu S-C, Zhang X-Y, Tu S-S (2015) Diagnosis and surgical treatment of esophageal gastrointestinal stromal tumors. World J Gastroenterol 21:5630–5634. https://doi.org/10.3748/wjg.v21.i18.5630
Briel JW, Tamhankar AP, Hagen JA, DeMeester SR, Johansson J, Choustoulakis E, Peters JH, Bremner CG, DeMeester TR (2004) Prevalence and risk factors for ischemia, leak, and stricture of esophageal anastomosis: gastric pull-up versus colon interposition. J Am Coll Surg 198:536–541. https://doi.org/10.1016/j.jamcollsurg.2003.11.026
Law S, Fok M, Chu KM, Wong J (1997) Comparison of hand-sewn and stapled esophagogastric anastomosis after esophageal resection for cancer: a prospective randomized controlled trial. Ann Surg 226:169–173. https://doi.org/10.1097/00000658-199708000-00008
Martínek J, Juhas S, Dolezel R, Walterová B, Juhasova J, Klima J, Rabekova Z, Vacková Z (2018) Prevention of esophageal strictures after circumferential endoscopic submucosal dissection. Minerva Chir 73:394–409. https://doi.org/10.23736/S0026-4733.18.07751-9
Pence K, Correa AM, Chan E, Khaitan P, Hofstetter W, Kim MP (2017) Management of esophageal gastrointestinal stromal tumor: review of one hundred seven patients. Dis Esophagus 30:1–5. https://doi.org/10.1093/dote/dox064
Chen T-Y, Xu J-X, Chen W-F, Li Q-L, Cai M-Y, Hu J-W, Qin W-Z, Ji Y, Xu X-Y, Zhang Y-Q, Zhou P-H (2022) Long-term prognosis of small gastric gastrointestinal stromal tumors with high histological grade: a longitudinal nested cohort study. Surg Endosc 36:4042–4049. https://doi.org/10.1007/s00464-021-08725-2
Chen T-H, Hsu C-M, Chu Y-Y, Wu C-H, Chen T-C, Hsu J-T, Yeh T-S, Lin C-J, Chiu C-T (2016) Association of endoscopic ultrasonographic parameters and gastrointestinal stromal tumors (GISTs): can endoscopic ultrasonography be used to screen gastric GISTs for potential malignancy? Scand J Gastroenterol 51:374–377. https://doi.org/10.3109/00365521.2015.1095350
Swinnen J, Eisendrath P, Rigaux J, Kahegeshe L, Lemmers A, Le Moine O, Devière J (2011) Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc 73:890–899. https://doi.org/10.1016/j.gie.2010.12.019
Inbar R, Santo E, Subchi AE-A, Korianski J, Halperin Z, Greenberg R, Avital S (2011) Insertion of removable self-expanding metal stents as a treatment for postoperative leaks and perforations of the esophagus and stomach. Isr Med Assoc J 13:230–233
Babor R, Talbot M, Tyndal A (2009) Treatment of upper gastrointestinal leaks with a removable, covered, self-expanding metallic stent. Surg Laparosc Endosc Percutan Tech 19:e1-4. https://doi.org/10.1097/SLE.0b013e318196c706
McCarter MD, Antonescu CR, Ballman KV, Maki RG, Pisters PWT, Demetri GD, Blanke CD, von Mehren M, Brennan MF, McCall L, Ota DM, DeMatteo RP, American College of Surgeons Oncology Group (ACOSOG) Intergroup Adjuvant Gist Study Team (2012) Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg 215:53–59. https://doi.org/10.1016/j.jamcollsurg.2012.05.008
Zhu Y, Xu M-D, Xu C, Zhang X-C, Chen S-Y, Zhong Y-S, Zhang Y-Q, Chen W-F, Chen T-Y, Xu J-X, Yao L-Q, Li Q-L, Zhou P-H (2020) Microscopic positive tumor margin does not increase the rate of recurrence in endoscopic resected gastric mesenchymal tumors compared to negative tumor margin. Surg Endosc 34:159–169. https://doi.org/10.1007/s00464-019-06744-8
Hou Y-Y, Lu S-H, Zhou Y, Qi W-D, Shi Y, Tan Y-S, Zhu X-Z (2009) Stage and histological grade of gastrointestinal stromal tumors based on a new approach are strongly associated with clinical behaviors. Mod Pathol 22:556–569. https://doi.org/10.1038/modpathol.2009.11
Hou Y-Y, Lu S-H, Zhou Y, Xu J-F, Ji Y, Hou J, Qi W-D, Shi Y, Tan Y-S, Zhu X-Z (2009) Predictive values of clinical and pathological parameters for malignancy of gastrointestinal stromal tumors. Histol Histopathol 24:737–747. https://doi.org/10.14670/HH-24.737
Funding
This study was supported by grants from National Natural Science Foundation of China (82172787), Shanghai Science and Technology Commission (19ZR1409600), Youth fund of Shanghai Municipal Science and Technology Committee (20194Y0138), and Special fund for clinical research of Zhongshan Hospital (2020ZXLC33).
Author information
Authors and Affiliations
Contributions
J-XX: writing–original draft. T-YC: writing–original draft. Y-BL: methodology. X-YX: resources. W-FC: resources. Q-LL: resources. J-WH: resources. W-ZQ: resources. M-YC: resources. Y-QZ: conceptualization; supervision; writing–review & editing. P-HZ: writing–review & editing.
Corresponding authors
Ethics declarations
Disclosures
Jia-Xin Xu, Tian-Yin Chen, Yan-Bo Liu, Xiao-Yue Xu, Wei-Feng Chen, Quan-Lin Li, Jian-Wei Hu, Wen-Zheng Qin, Ming-Yan Cai, Yi-Qun Zhang, and Ping-Hong Zhou have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, JX., Chen, TY., Liu, YB. et al. Clinical outcomes of endoscopic resection for the treatment of esophageal gastrointestinal stromal tumors: a ten-year experience from a large tertiary center in China. Surg Endosc 37, 5883–5893 (2023). https://doi.org/10.1007/s00464-023-10032-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10032-x