Abstract
Background
In the treatment of small gastric subepithelial tumors originating from muscularis propria (SET-MPs), endoscopic full-thickness resection (EFTR) has been an effective procedure and ligation-assisted EFTR (EFTR-L) seems a feasible and promising operation. We aimed to compare the therapeutic outcomes of EFTR-L and EFTR to evaluate effect and safety of either method in the treatment of small (≤ 1.5 cm) gastric SET-MPs.
Methods
Between January 2018 to May 2022, we retrospectively enrolled a total of 119 patients with gastric SET-MPs treated by EFTR-L (79 patients) or EFTR (40 patients) at Xiangya Hospital Central South University. Clinical characteristics, operation efficacy, adverse events (AEs), and operation cost were compared between the 2 groups. Univariate and multiple logistic and linear regressions were applied to analyze the therapeutic outcomes of the procedure, and covariates were adjusted in the multiple analysis.
Results
The operation time of EFTR-L group (16.34 ± 5.75 min) was significantly shorter than EFTR group (51.23 ± 21.21 min, P < 0.001), and the difference remained significant after adjusting the covariates (adjusted mean difference, 30.56; 95% confidence interval, 25.65–35.47; P < 0.001). The operation cost of EFTR-L group was lower than EFTR group (1268.52 ± 457.22 vs 1643.18 ± 295.08 $; P < 0.001). The complete resection rate of the EFTR-L group was 98.72% and of the EFTR group 100%. The incidence of abdominal pain in the EFTR-L group (5.06%) was lower than in the EFTR group (27.50%, P = 0.008). A patient in the EFTR group underwent severe pneumoperitoneum and received abdominocentesis during operation. One case of peritonitis occurred in the EFTR-L group but recovered from intensified antibiotic therapy. No delayed blood or perforation occurred.
Conclusions
Compared to EFTR, EFTR-L might be a feasible procedure for small (≤ 1.5 cm) gastric SET-MPs due to the acceptable efficacy, shorter operation time, and lower cost.
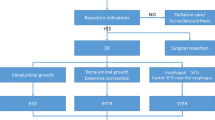
Graphical abstract




Similar content being viewed by others
References
Kim GH (2012) Endoscopic resection of subepithelial tumors. Clin Endosc 45:240–244. https://doi.org/10.5946/ce.2012.45.3.240
Zhang D, Lin Q, Shi R (2018) Ligation-assisted endoscopic submucosal resection with apical mucosal incision to treat gastric subepithelial tumors originating from the muscularis propria. Endoscopy 50:1180–1185. https://doi.org/10.1055/a-0625-6326
Faulx A, Kothari S, Acosta RD (2017) The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc 85:1117–1132. https://doi.org/10.1016/j.gie.2017.02.022
Deprez PH, Moons LMG, OʼToole D, et al (2022) Endoscopic management of subepithelial lesions including neuroendocrine neoplasms: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 54:412–429. https://doi.org/10.1055/a-1751-5742
Cai MY, Zhou PH, Yao LQ (2012) Current status of endoscopic resection in China. Dig Endosc 24:166–171. https://doi.org/10.1111/j.1443-1661.2012.01268.x
Cai MY, Martin Carreras-Presas F, Zhou PH (2018) Endoscopic full-thickness resection for gastrointestinal submucosal tumors. Dig Endosc 30:17–24. https://doi.org/10.1111/den.13003
Hajifathalian K, Ichkhanian Y, Dawod Q et al (2020) Full-thickness resection device (FTRD) for treatment of upper gastrointestinal tract lesions: the first international experience. Endosc Int Open 8:E1291-1301. https://doi.org/10.1055/a-1216-1439
Meier B, Schmidt A, Glaser N et al (2020) Endoscopic full-thickness resection of gastric subepithelial tumors with the gFTRD-system: a prospective pilot study (RESET trial). Surg Endosc 34:853–860. https://doi.org/10.1007/s00464-019-06839-2
Granata A, Martino A, Ligresti D (2022) Exposed endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors: A systematic review and pooled analysis. Dig Liver Dis 54:729–736. https://doi.org/10.1016/j.dld.2021.09.014
Wang C, Gao Z, Shen K et al (2020) Safety and efficiency of endoscopic re-section versus laparoscopic resection in gastric gastrointestinal stromal tumours: a systematic review and meta-analysis. Eur J Surg Oncol 46:667–674. https://doi.org/10.1016/j.ejso.2019.10.030
Casali PG, Abecassis N, Aro HT et al (2018) Gastrointestinal stromal tumors: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. https://doi.org/10.1093/annonc/mdy095
von Mehren M, Kane JM, Bui MM et al (2020) NCCN guidelines insights: Softtissue sarcoma, version 1.2021. J Natl Compr Canc Netw 18:1604–1612. https://doi.org/10.6004/jnccn.2020.0058
Li L, Cristofaro S, Zhou X, Xu L et al (2017) Endoscopic submucosal resection: a novel technique for resection of a small gastric stromal tumor from the muscularis propria. Am J Gastroenterol 112:679. https://doi.org/10.1038/ajg.2016.590
Li LY, Li BW, Mekaroonkamol P et al (2020) Mucosectomy device-assisted endoscopic resection of gastric subepithelial lesions. J Dig Dis 21:215–221. https://doi.org/10.1111/1751-2980.12856
Li QL, Yao LQ, Zhou PH et al (2012) Submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a large study of endoscopic submucosal dissection (with video). Gastrointest Endosc 75:1153–1158. https://doi.org/10.1016/j.gie.2012.01.037
Ye LP, Zhang Y, Luo DH et al (2016) Safety of endoscopic resection for upper gastrointestinal subepithelial tumors originating from the muscularis propria layer: an analysis of 733 tumors. Am J Gastroenterol 111:788–796. https://doi.org/10.1038/ajg.2015.426
Joo MK, Park JJ, Kim H et al (2016) Endoscopic versus surgical resection of GI stromal tumors in the upper GI tract. Gastrointest Endosc 83:318–326. https://doi.org/10.1016/j.gie.2015.07.034
Chen H, Li B, Li L et al (2019) Current status of endoscopic resection of gastric subepithelial tumors. Am J Gastroenterol 114:718–725. https://doi.org/10.14309/ajg.0000000000000196
Xiu H, Zhao C, Liu FG et al (2019) Comparing about three types of endsoscopic therapy methods for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. Scand J Gastroenterol 54:1481–1486. https://doi.org/10.1080/00365521.2019.1692064
Blaisdell PC (1958) Office ligation of internal hemorrhoids. Am J Surg 96:401–404. https://doi.org/10.1016/0002-9610(58)90933-4
Ji JS, Cho YS (2013) Endoscopic band ligation: beyond prevention and management of gastroesophageal varices. World J Gastroenterol 19:4271–4276. https://doi.org/10.3748/wjg.v19.i27.4271
Li S, Liang X, Zhang B et al (2021) Novel endoscopic management for small gastric submucosal tumors: a single-center experience (with video). Dig Liver Dis 53:895–899. https://doi.org/10.1016/j.dld.2021.02.014
Guo J, Liu Z, Sun S et al (2013) Ligation-assisted endoscopic enucleation for the diagnosis and resection of small gastrointestinal tumors originating from the muscularis propria: a preliminary study. BMC Gastroenterol 13:88. https://doi.org/10.1186/1471-230X-13-88
Zheng Z, Jiao G, Wang T et al (2016) Ligation-assisted endoscopic enucleation for the resection of gastrointestinal tumors originating from the muscularis propria: analysis of efficacy and facility. Dig Surg 33:488–494. https://doi.org/10.1159/000445957
Ge N, Hu JL, Yang F et al (2019) Endoscopic full-thickness resection for treating small tumors originating from the muscularis propria in the gastric fundus: An improvement in technique over 15 years. World J Gastrointest Oncol 11:1054–1064. https://doi.org/10.4251/wjgo.v11.i11.1054
Ahmed I, Shibukawa G, Groce R et al (2007) Study of full-thickness endoluminal segmental resection of colon in a porcine colon model (with videos). Gastrointest Endosc 65:696–702. https://doi.org/10.1016/j.gie.2006.10.051
Yang J, Ni M, Jiang J et al (2022) Comparison of endoscopic full-thickness resection and cap-assisted endoscopic full-thickness resection in the treatment of small (≤1.5 cm) gastric GI stromal tumors. Gastrointest Endosc 95:660-670.e2. https://doi.org/10.1016/j.gie.2021.10.026
Meier B, Stritzke B, Kuellmer A et al (2020) Efficacy and safety of endoscopic full-thickness resection in the colorectum: results from the German colonic FTRD registry. Am J Gastroenterol 115:1998–2006. https://doi.org/10.14309/ajg.0000000000000795
Acknowledgements
This project was supported by Appropriate Technology Promotion Project of National Clinical Research Center for Geriatric Disorders (Xiangya Hospital) (XYYYJSTG-11). No other funding organization played a role in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript. We thank Ms. Menglin Gu (Department of Visual Communication, College of Art and Design, Hunan First Normal University) for drawing schematic diagram.
Funding
This work was supported by grant funded by National Research Center of Geriatric Diseases (Xiangya Hospital of Central South University) (XYYYJSTG-11). No other funding organization played a role in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
LG, YW, and XL: designed the study; LG and YW: collected data of patients and performed follow-up visit; LG: analyzed data and wrote the manuscript; MO and JY revised the manuscript; YW and XL: modified the manuscript critically. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Disclosures
Authors Lei Gu, Yu Wu, Jun Yi, Miao Ouyang, and Xiaowei Liu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gu, L., Wu, Y., Yi, J. et al. Comparison of endoscopic full-thickness resection and ligation-assisted endoscopic full-thickness resection for small (≤ 1.5 cm) gastric subepithelial tumors originating from muscularis propria. Surg Endosc 37, 3796–3806 (2023). https://doi.org/10.1007/s00464-023-09881-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09881-3