Abstract
Background and aims
With the development of endoscopic technology, endoscopic treatment has been widely used in Gastrointestinal stromal tumors (GISTs). However, population-based studies comparing the long-term results of patients who received endoscopic treatment vs. Surgery are lacking. We used the Surveillance, Epidemiology, and End Results (SEER) database to analyze the long-term survival of colorectal or gastric GISTs who underwent primary tumor resection (endoscopic therapy or surgery) in the USA.
Methods
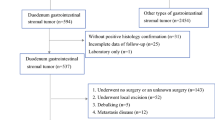
Patients with colorectal or gastric GISTs were selected from the SEER database between 2010 and 2015. Kaplan–Meier analyses and log-rank tests were used to evaluate the difference in the long-term survival between the endoscopic therapy group and the surgery group. We examined the association between different treatments and survival after using the multivariate cox proportional hazards model to adjust the relevant covariates. Besides, we used Propensity score matching (PSM) to overcome the different distributions of covariates between the two groups and then further compare the survival difference.
Results
In total, 2355 patients were enrolled in our study, of which 1999 (84.9%) received surgical treatment and 356 (15.1%) received endoscopic treatment. There was no significant difference in overall survival (OS) between the two groups before PSM. The median OS (73.5 months vs. 72.2 months) and 5-year OS rate (85.7% vs. 81.5%) of endoscopic therapy were similar to surgical patients (P = 0.34). The median Cancer-specific survival (CSS) and 5-year CSS rate in the endoscopic treatment group were higher than the surgical group before PSM, with 81.3 months, 97.1% versus 78.8 months, 92.7% (P = 0.011). After adjusting for other clinical factors and PSM, the long-term OS and CSS did not significantly differ between those treated surgically and treated endoscopically.
Conclusion
Based on the American population, we preliminarily found that the long-term OS and CSS did not differ between patients undergoing endoscopic therapy and surgery.




Similar content being viewed by others
Data availability
All data used in this paper may be accessed via the SEER*Stat web program following the submission of a request for access to the data at https://seer.cancer.gov/seertrack/data/request/.
References
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN task force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8(Suppl 2):S1-41
Blay JY, Kang YK, Nishida T, von Mehren M (2021) Gastrointestinal stromal tumours. Nat Rev Dis Primers 7:22
Joensuu H, Hohenberger P, Corless CL (2013) Gastrointestinal stromal tumour. Lancet 382:973–983
Etherington MS, DeMatteo RP (2019) Tailored management of primary gastrointestinal stromal tumors. Cancer 125:2164–2171
Lei T, Tan F, Liu H, Ouyang M, Zhou H, Liu P, Zhao X, Li B (2020) Endoscopic or surgical resection for patients with 2–5cm gastric gastrointestinal stromal tumors: a single-center 12-year experience from China. Cancer Manage Res 12:7659–7670
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58
Pourmousavi MK, Wang R, Kerdsirichairat T, Kamal A, Akshintala VS, Hajiyeva G, Lopimpisuth C, Hanada Y, Kumbhari V, Singh VK, Khashab MA, Brewer OG, Shin EJ, Canto MI, Lennon AM, Ngamruengphong S (2020) Comparable cancer-specific mortality of patients with early gastric cancer treated with endoscopic therapy vs surgical resection. Clin Gastroenterol Hepatol 18:2824-2832.e2821
Frühmorgen P, Rufle W, Kobras S, Seeliger H, Herrmann G (2003) Endoscopic therapy of early colorectal cancer (pT1) - a prospective study. Z Gastroenterol 41:703–710
Malik S, Sharma G, Sanaka MR, Thota PN (2018) Role of endoscopic therapy in early esophageal cancer. World J Gastroenterol 24:3965–3973
Balde AI, Chen T, Hu Y, Redondo NJ, Liu H, Gong W, Yu J, Zhen L, Li G (2017) Safety analysis of laparoscopic endoscopic cooperative surgery versus endoscopic submucosal dissection for selected gastric gastrointestinal stromal tumors: a propensity score-matched study. Surg Endosc 31:843–851
Wu CR, Huang LY, Guo J, Zhang B, Cui J, Sun CM, Jiang LX, Wang ZH, Ju AH (2015) Clinical control study of endoscopic full-thickness resection and laparoscopic surgery in the treatment of gastric tumors arising from the muscularis propria. Chin Med J (England) 128:1455–1459
Du C, Linghu E (2017) Submucosal tunneling endoscopic resection for the treatment of gastrointestinal submucosal tumors originating from the muscularis propria layer. J Gastrointest Surg 21:2100–2109
Jones RL, Serrano C, von Mehren M, George S, Heinrich MC, Kang YK, Schöffski P, Cassier PA, Mir O, Chawla SP, Eskens F, Rutkowski P, Tap WD, Zhou T, Roche M, Bauer S (2021) Avapritinib in unresectable or metastatic PDGFRA D842V-mutant gastrointestinal stromal tumours: long-term efficacy and safety data from the NAVIGATOR phase I trial. Eur J Cancer 145:132–142
Ye S, Sharipova D, Kozinova M, Klug L, D’Souza J, Belinsky MG, Johnson KJ, Einarson MB, Devarajan K, Zhou Y, Litwin S, Heinrich MC, DeMatteo R, von Mehren M, Duncan JS, Rink L (2021) Identification of Wee1 as a target in combination with avapritinib for gastrointestinal stromal tumor treatment. JCI Insight. https://doi.org/10.1172/jci.insight.143474
He B, Yan S, Li R, Qiu H, Tu J (2018) A comparative study of treatment of gastrointestinal stromal tumors with laparoscopic surgery: a retrospective study. J Buon 23:820–825
Wang C, Gao Z, Shen K, Cao J, Shen Z, Jiang K, Wang S, Ye Y (2020) Safety and efficiency of endoscopic resection versus laparoscopic resection in gastric gastrointestinal stromal tumours: a systematic review and meta-analysis. Eur J Surg Oncol 46:667–674
Huang LY, Cui J, Wu CR, Zhang B, Jiang LX, Xian XS, Lin SJ, Xu N, Cao XL, Wang ZH (2014) Endoscopic full-thickness resection and laparoscopic surgery for treatment of gastric stromal tumors. World J Gastroenterol 20:8253–8259
Yin X, Yin Y, Chen H, Shen C, Tang S, Cai Z, Zhang B, Chen Z (2018) Comparison analysis of three different types of minimally invasive procedures for gastrointestinal stromal tumors ≤5 cm. J Laparoendosc Adv Surg Tech A 28:58–64
Dong HY, Wang YL, Jia XY, Li J, Li GD, Li YQ (2014) Modified laparoscopic intragastric surgery and endoscopic full-thickness resection for gastric stromal tumor originating from the muscularis propria. Surg Endosc 28:1447–1453
Dai WJ, Liu G, Wang M, Liu WJ, Song W, Yang XZ, Wang QL, Zhang XY, Fan ZN (2017) Endoscopic versus laparoscopic resection of gastric gastrointestinal stromal tumors: a multicenter study. Oncotarget 8:11259–11267
Liu S, Zhou X, Yao Y, Shi K, Yu M, Ji F (2020) Resection of the gastric submucosal tumor (G-SMT) originating from the muscularis propria layer: comparison of efficacy, patients’ tolerability, and clinical outcomes between endoscopic full-thickness resection and surgical resection. Surg Endosc 34:4053–4064
Zhu H, Zhao S, Jiao R, Zhou J, Zhang C, Miao L (2020) Comparison of endoscopic versus laparoscopic resection for gastric gastrointestinal stromal tumors: a preliminary meta-analysis. J Gastroenterol Hepatol 35:1858–1868
Wang H, Cao L, Zheng K, Zhao Y (2018) Laparoscopic endoscopic cooperative surgery for gastrointestinal stromal tumors. Surg Laparosc Endosc Percutan Tech 28:354–358
Tsujimoto H, Yaguchi Y, Kumano I, Takahata R, Ono S, Hase K (2012) Successful gastric submucosal tumor resection using laparoscopic and endoscopic cooperative surgery. World J Surg 36:327–330
Qiu WQ, Zhuang J, Wang M, Liu H, Shen ZY, Xue HB, Shen L, Ge ZZ, Cao H (2013) Minimally invasive treatment of laparoscopic and endoscopic cooperative surgery for patients with gastric gastrointestinal stromal tumors. J Dig Dis 14:469–473
Zhao Y, Pang T, Zhang B, Wang L, Lv Y, Ling T, Zhang X, Huang Q, Xu G, Zou X (2020) Retrospective comparison of endoscopic full-thickness versus laparoscopic or surgical resection of small (≤ 5 cm) gastric gastrointestinal stromal tumors. J Gastrointest Surg 24:2714–2721
Acknowledgements
We thank the Surveillance, Epidemiology, and End Results (SEER) database and our collaborators who helped with this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
LLY designed the study. JJW and RJZ performed data mining. LLY, KDC, and ZHJ analyzed the data. LLY and JJW drafted the initial manuscript. GZJ and XHZ contributed to the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Disclosures
Linlin Yin, Jingjing Wang, Rongjie Zhao, Kangdi Chen, Zuhong Ji, Xiuhua Zhang, and Guozhong Ji have declared that they have no conflicts of interest or financial ties to disclose.
Ethical approval
Institutional review board approval was not needed for this study as it utilized publically available data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
464_2021_8755_MOESM1_ESM.tif
Supplementary file1 The appropriate cutoff values of age and tumor size was assessed by X-tile analysis (A, B). The appropriate cutoff values of age were 66 and 75 years (C, D). The appropriate cutoff values of tumor size were 56 and 143 mm (TIF 8626 kb)
464_2021_8755_MOESM2_ESM.tif
Supplementary file2 Forest plots summarize the HR and 95% CI of overall survival according to treatment methods (TIF 4561 kb)
464_2021_8755_MOESM3_ESM.tif
Supplementary file3 Forest plots summarize the HR and 95% CI of cancer-specific survival according to treatment methods (TIF 4586 kb)
Rights and permissions
About this article
Cite this article
Yin, L., Wang, J., Zhao, R. et al. Comparable long-term survival of patients with colorectal or gastric gastrointestinal stromal tumors treated with endoscopic vs. surgical resection. Surg Endosc 36, 4215–4225 (2022). https://doi.org/10.1007/s00464-021-08755-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08755-w