Abstract
Background
Despite the increasing utilization of transanal total mesorectal excision as a promising approach for low rectal cancer, the feasibility and safety of transperineal minimally invasive abdominoperineal resection (tp-APR) remain unclear.
Methods
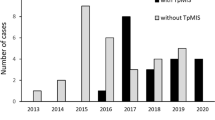
In total, 25 patients who underwent tp-APR between April 2017 and May 2020 (tp-APR group) and 27 patients who underwent conventional laparoscopic APR between May 2009 and September 2016 (lap-APR group) for low rectal cancer were enrolled in this retrospective study. Clinical outcomes were compared between the groups before and after propensity score matching. The primary outcome was the incidence of the overall postoperative complications with Clavien–Dindo grade II or above. Standardized technique of tp-APR was also demonstrated.
Results
On comparison, operative time, intraoperative blood loss, and overall postoperative complications with Clavien–Dindo grade II or above were significantly less in the tp-APR group both before and after propensity score matching. The rates of urinary disturbance and perineal wound infection were significantly less in the tp-APR group after matching. Further, postoperative hospital stay was significantly shorter in the tp-APR group both before and after matching. However, pathological outcomes did not differ between the groups before and after matching. There has been no local recurrence in the tp-APR group with a median follow-up period of 18 months.
Conclusion
Standardized tp-APR for low rectal cancer is feasible and seems superior to conventional laparoscopic APR in terms of short-term outcomes. Further larger-scale studies with a longer follow-up period are required to evaluate oncological outcomes.




Similar content being viewed by others
Change history
02 September 2021
This article was updated to correct the formatting of Table 3.
02 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00464-021-08709-2
References
Breukink SO, van der Zaag-Loonen HJ, Bouma EM, Pierie JP, Hoff C, Wiggers T, Meijerink WJ (2007) Prospective evaluation of quality of life and sexual functioning after laparoscopic total mesorectal excision. Dis Colon Rectum 50:147–155
Fields AC, Scully RE, Saadat LV, Lu P, Davids JS, Bleday R, Goldberg JE, Melnitchouk N (2019) Oncologic outcomes for low rectal adenocarcinoma following low anterior resection with coloanal anastomosis versus abdominoperineal resection: a National Cancer Database propensity matched analysis. Int J Colorectal Dis 34:843–848
van Leersum N, Martijnse I, den Dulk M, Kolfschoten N, Le Cessie S, van de Velde C, Tollenaar R, Wouters M, Rutten HJ (2014) Differences in circumferential resection margin involvement after abdominoperineal excision and low anterior resection no longer significant. Ann Surg 259:1150–1155
Wibe A, Syse A, Andersen E, Tretli S, Myrvold HE, Søreide O (2004) Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum 47:48–58
Han JG, Wang ZJ, Gao ZG, Wei GH, Yang Y, Zhai ZW, Zhao BC, Yi BQ (2019) Perineal wound complications after extralevator abdominoperineal excision for low rectal cancer. Dis Colon Rectum 62:1477–1484
Welten VM, Fields AC, Lu P, Goldberg JE, Irani J, Bleday R, Melnitchouk N (2019) Omental flaps in patients undergoing abdominoperineal resection for rectal cancer. Int J Colorectal Dis 34:1227–1232
Yan X, Su H, Zhang S, Zhou L, Lu J, Yang X, Li J, Xue P, He Z, Wang M, Lu A, Ma J, Zang L, Cai Z, Sun J, Hong H, Zheng M, Feng B (2020) Pelvic peritoneum closure reduces postoperative complications of laparoscopic abdominoperineal resection: 6-year experience in single center. Surg Endosc. https://doi.org/10.1007/s00464-020-07414-w
Lehtonen T, Räsänen M, Carpelan-Holmström M, Lepistö A (2019) Oncological outcomes before and after the extralevator abdominoperineal excision era in rectal cancer patients treated with abdominoperineal excision in a single centre, high volume unit. Colorectal Dis 21:183–190
Seshadri RA, West NP, Sundersingh S (2017) A pilot randomized study comparing extralevator with conventional abdominoperineal excision for low rectal cancer after neoadjuvant chemoradiation. Colorectal Dis 19:O253-o262
West NP, Anderin C, Smith KJ, Holm T, Quirke P (2010) Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg 97:588–599
Zhang Y, Wang D, Zhu L, Wang B, Ma X, Shi B, Yan Y, Zhou C (2017) Standard versus extralevator abdominoperineal excision and oncologic outcomes for patients with distal rectal cancer: a meta-analysis. Medicine 96:e9150
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24:1205–1210
Fernández-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, Díaz del Gobbo G, DeLacy B, Balust J, Lacy AM (2015) Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg 261:221–227
Hasegawa S, Yoshida Y, Morimoto M, Kojima D, Komono A, Aisu N, Taketomi H, Nagano H, Matsumoto Y, Munechika T, Kajitani R (2019) Transanal TME: new standard or fad? J Anus Rectum Colon 3:1–9
Hu D, Jin P, Hu L, Liu W, Zhang W, Guo T, Yang X (2018) The application of transanal total mesorectal excision for patients with middle and low rectal cancer: A systematic review and meta-analysis. Medicine 97:e11410
Jiang HP, Li YS, Wang B, Wang C, Liu F, Shen ZL, Ye YJ, Wang S (2018) Pathological outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a systematic review with meta-analysis. Surg Endosc 32:2632–2642
Al Furajii H, Kennedy N, Cahill RA (2017) Abdomino-endoscopic perineal excision of the rectum for benign and malignant pathology: technique considerations for true transperineal verus transanal total mesorectal excision endoscopic proctectomy. J Min Access Surg 13:7–12
Arolfo S, Bullano A, Allaix ME, Arezzo A, Morino M (2020) Transperineal minimally invasive abdomino-perineal resection: preliminary outcomes and future perspectives. Updates Surg 72:97–102
Han JG, Wang ZJ, Wei GH, Zhai ZW, Zhao BC (2020) Trans-perineal minimally invasive approach during extralevator abdominoperineal excision for advanced low rectal cancer: a retrospective cohort study. Asian J Surg. https://doi.org/10.1016/j.asjsur.2019.11.004
Yasukawa D, Hori T, Kadokawa Y, Kato S, Aisu Y, Hasegawa S (2019) Trans-perineal minimally invasive surgery during laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc 33:437–447
van Oostendorp SE, Roodbeen SX, Chen CC, Caycedo-Marulanda A, Joshi HM, Tanis PJ, Cunningham C, Tuynman JB, Hompes R (2020) Transperineal minimally invasive APE: preliminary outcomes in a multicenter cohort. Tech Coloproctol 24:823–831
Wasmuth HH, Faerden AE, Myklebust T, Pfeffer F, Norderval S, Riis R, Olsen OC, Lambrecht JR, Kørner H, Larsen SG, Forsmo HM, Baekkelund O, Lavik S, Knapp JC, Sjo O, Rashid G (2020) Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg 107:121–130
de Lacy AM, Rattner DW, Adelsdorfer C, Tasende MM, Fernández M, Delgado S, Sylla P, Martínez-Palli G (2013) Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME)–short-term outcomes in the first 20 cases. Surg Endosc 27:3165–3172
Matsuda T, Yamashita K, Hasegawa H, Arimoto A, Watanabe A, Yamamoto M, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2020) Reliable dissection technique during transanal total mesorectal excision using a lateral-first approach. Dis Colon Rectum 63:859
Matsuda T, Hasegawa H, Yamashita K, Tanaka T, Yamamoto M, Kanaji S, Oshikiri T, Nakamura T, Sumi Y, Suzuki S, Kakeji Y (2020) Laparoscopic lateral pelvic lymph node dissection for lower rectal cancer treated with preoperative chemoradiotherapy. Surg Endosc 34:1425–1431
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Matsuda T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2018) Outcomes and prognostic factors of selective lateral pelvic lymph node dissection with preoperative chemoradiotherapy for locally advanced rectal cancer. Int J Colorectal Dis 33:367–374
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Atallah S, Albert M, Monson JR (2016) Critical concepts and important anatomic landmarks encountered during transanal total mesorectal excision (taTME): toward the mastery of a new operation for rectal cancer surgery. Tech Coloproctol 20:483–494
Hüscher CG, Tierno SM, Romeo V, Lirici MM (2016) Technologies, technical steps, and early postoperative results of transanal TME. Minim Invasive Ther Allied Technol 25:247–256
Watanabe J, Ishibe A, Suwa Y, Suwa H, Momiyama M, Ota M, Endo I (2018) Surgical techniques for identification of the prostate gland using the autonomic nerve as a landmark during transanal total mesorectal excision: secure dissection of the male rectourethral muscle. Dis Colon Rectum 61:999–1000
Japanese Society for Cancer of the Colon and Rectum (2019) Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3rd English edition. J Anus Rectum Colon 3:175–195
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Takeru Matsuda, Kimihiro Yamashita, Hiroshi Hasegawa, Shingo Kanaji, Taro Oshikiri, Tetsu Nakamura, Satoshi Suzuki, and Yoshihiro Kakeji have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 30845 kb)
Supplementary file2 (MP4 28742 kb)
Supplementary file3 (MP4 29786 kb)
Rights and permissions
About this article
Cite this article
Matsuda, T., Yamashita, K., Hasegawa, H. et al. Transperineal minimally invasive abdominoperineal resection for low rectal cancer: standardized technique and clinical outcomes. Surg Endosc 35, 7236–7245 (2021). https://doi.org/10.1007/s00464-021-08633-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08633-5