Abstract
Background and aims
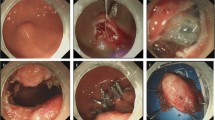
Sessile serrated lesions (SSLs) are more prone to incomplete resection than conventional adenomas. This study evaluated whether circumferential submucosal incision prior to endoscopic mucosal resection (CSI-EMR) can increase the rate of complete and en bloc resections of colorectal lesions with endoscopic features of SSL.
Methods
Retrospective analyses and propensity score matching were performed for the resection of colorectal lesions ≥ 10 mm with endoscopic features of SSL.
Results
After 1:1 ratio matching, 127 lesions in the CSI-EMR group and 127 in the EMR group were selected for analysis. The median size of the lesions was 15 mm (IQR 12–16) in both groups. There was no significant difference in either the complete resection rate or en bloc resection rate between CSI-EMR and EMR groups (96.9% vs. 92.9%, P = 0.155; 92.1% vs. 89.0%, P = 0.391). By contrast, the R0 resection rate was significantly higher in the CSI-EMR group than in the EMR group (89.8% vs. 59.8%, P < 0.001). The median procedure time was significantly longer in the CSI-EMR group than in the EMR group (6.28 min vs. 2.55 min, P < 0.001), whereas there was no significant difference between the two groups in the incidence of adverse events or recurrence rate. Multivariate analysis showed that CSI-EMR was the only factor significantly associated with R0 resection (P < 0.001).
Conclusions
For colorectal lesions with endoscopic features of SSL, CSI-EMR does not increase the complete or en bloc resection rate, but does increase the R0 resection rate. The procedure time is longer for CSI-EMR than EMR. The association of CSI-EMR with R0 resection and non-recurrence should be further evaluated.



Similar content being viewed by others
Abbreviations
- SSL:
-
Sessile serrated lesion
- CSI-EMR:
-
Circumferential submucosal incision prior to endoscopic mucosal resection
- EMR:
-
Endoscopic mucosal resection
- HPs:
-
Hyperplastic polyps
- IQR:
-
Interquartile range
- SMD:
-
Standardized mean difference
- OR:
-
Odd ratios
- CI:
-
Confidence interval
References
Zauber AG, Winawer SJ, O’Brien MJ et al (2012) Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 366:687–696
Moss A, Bourke MJ, Tran K et al (2010) Lesion isolation by circumferential submucosal incision prior to endoscopic mucosal resection (CSI-EMR) substantially improves en bloc resection rates for 40-mm colonic lesions. Endoscopy 42:400–404
Singh S, Singh PP, Murad MH et al (2014) Prevalence, risk factors, and outcomes of interval colorectal cancers: a systematic review and meta-analysis. Am J Gastroenterol 109:1375–1389
Ma MX, Bourke MJ (2017) Sessile serrated adenomas: how to detect, characterize and resect. Gut Liver 11:747–760
Sawhney MS, Farrar WD, Gudiseva S et al (2006) Microsatellite instability in interval colon cancers. Gastroenterology 131:1700–1705
Arain MA, Sawhney M, Sheikh S et al (2010) CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol 105:1189–1195
Rex DK, Ahnen DJ, Baron JA et al (2012) Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol 107:1315–1329; quiz 1314, 1330
Bouwens MW, van Herwaarden YJ, Winkens B et al (2014) Endoscopic characterization of sessile serrated adenomas/polyps with and without dysplasia. Endoscopy 46:225–235
Burgess NG, Tutticci NJ, Pellise M et al (2014) Sessile serrated adenomas/polyps with cytologic dysplasia: a triple threat for interval cancer. Gastrointest Endosc 80:307–310
Pohl H, Srivastava A, Bensen SP et al (2013) Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology 144(74–80):e71
Chandrasekar VT, Aziz M, Patel HK et al (2019) Efficacy and safety of endoscopic resection of sessile serrated polyps 10 mm or larger: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2019.11.041
Lee SH, Shin SJ, Park DI et al (2012) Korean guideline for colonoscopic polypectomy. Clin Endosc 45:11–24
Horiuchi A, Makino T, Kajiyama M et al (2016) Comparison between endoscopic mucosal resection and hot snare resection of large nonpedunculated colorectal polyps: a randomized trial. Endoscopy 48:646–651
Rao AK, Soetikno R, Raju GS et al (2016) Large sessile serrated polyps can be safely and effectively removed by endoscopic mucosal resection. Clin Gastroenterol Hepatol 14:568–574
Pellise M, Burgess NG, Tutticci N et al (2017) Endoscopic mucosal resection for large serrated lesions in comparison with adenomas: a prospective multicentre study of 2000 lesions. Gut 66:644–653
Agarwal A, Garimall S, Scott FI et al (2018) En bloc endoscopic mucosal resection is equally effective for sessile serrated polyps and conventional adenomas. Surg Endosc 32:1871–1878
Cheung DY, Choi SK, Kim HK et al (2015) Circumferential submucosal incision prior to endoscopic mucosal resection provides comparable clinical outcomes to submucosal dissection for well-differentiated neuroendocrine tumors of the rectum. Surg Endosc 29:1500–1505
Sakamoto T, Matsuda T, Nakajima T et al (2012) Efficacy of endoscopic mucosal resection with circumferential incision for patients with large colorectal tumors. Clin Gastroenterol Hepatol 10:22–26
IJspeert JEG, Bastiaansen BA, van Leerdam ME et al (2016) Development and validation of the WASP classification system for optical diagnosis of adenomas, hyperplastic polyps and sessile serrated adenomas/polyps. Gut 65:963–970
Lambert R. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003; 58: S3-S43.
World Health Organisation (2019) Classification of tumours of the digestive tract. IARC Press, Lyon
Kawamura T, Takeuchi Y, Asai S et al (2018) A comparison of the resection rate for cold and hot snare polypectomy for 4–9 mm colorectal polyps: a multicentre randomised controlled trial (CRESCENT study). Gut 67:1950–1957
Zhang Q, Gao P, Han B et al (2018) Polypectomy for complete endoscopic resection of small colorectal polyps. Gastrointest Endosc 87:733–740
Robertson DJ, Lieberman DA, Winawer SJ et al (2014) Colorectal cancers soon after colonoscopy: a pooled multicohort analysis. Gut 63:949–956
Saito Y, Uraoka T, Matsuda T et al (2007) Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video). Gastrointest Endosc 66:966–973
Iishi H, Tatsuta M, Iseki K et al (2000) Endoscopic piecemeal resection with submucosal saline injection of large sessile colorectal polyps. Gastrointest Endosc 51:697–700
Saito Y, Fukuzawa M, Matsuda T et al (2010) Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24:343–352
Yoshida N, Inoue K, Dohi O et al (2019) Efficacy of precutting endoscopic mucosal resection with full or partial circumferential incision using a snare tip for difficult colorectal lesions. Endoscopy 51:871–876
Makazu M, Sakamoto T, So E et al (2015) Relationship between indeterminate or positive lateral margin and local recurrence after endoscopic resection of colorectal polyps. Endosc Int Open 3:E252-257
Arimoto J, Higurashi T, Chiba H et al (2019) Investigation of the local recurrence rate after colorectal endoscopic mucosal resection: is incomplete polyp resection really a clinically important problem? Analysis of the rationale for the “Resect and Discard” strategy. Can J Gastroenterol Hepatol 2019:7243515
Crockett SD, Nagtegaal ID (2019) Terminology, molecular features, epidemiology, and management of serrated colorectal neoplasia. Gastroenterology 157(949–966):e944
Kim SW, Cha JM, Lee JI et al (2010) A significant number of sessile serrated adenomas might not be accurately diagnosed in daily practice. Gut Liver 4:498–502
Tinmouth J, Henry P, Hsieh E et al (2014) Sessile serrated polyps at screening colonoscopy: have they been under diagnosed? Am J Gastroenterol 109:1698–1704
Spring KJ, Zhao ZZ, Karamatic R et al (2006) High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology 131:1400–1407
Atkinson NS, East JE (2015) Optical biopsy and sessile serrated polyps: is DISCARD dead? Long live DISCARD-lite! Gastrointest Endosc 82:118–121
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Dr. Bo-In Lee was consultant to Taejoon Pharm, Pentax. Co., Olympus Co., Abbvie Co., and Medtronics Co. Drs. Chang Kyo Oh, Sung Hak Lee, Seung-Jun Kim, Han Hee Lee, Chul-Hyun Lim, Jin Su Kim, Yu Kyung Cho, Jae Myung Park, Young-Seok Cho, In Seok Lee, and Myung-Gyu Choi have no conflicts of interest or financial ties to disclose.
Ethical approval
The study protocol was approved by the Institutional Review Board of the Catholic Medical Center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oh, C., Lee, BI., Lee, S. et al. Circumferential submucosal incision prior to endoscopic mucosal resection versus conventional endoscopic mucosal resection for colorectal lesions with endoscopic features of sessile serrated lesions. Surg Endosc 36, 2087–2095 (2022). https://doi.org/10.1007/s00464-021-08495-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08495-x