Abstract
Background
Choledocholithiasis is a common complication of cholelithiasis, occurring in up to 18% of patients. Multiple treatments are often performed during the course of the management of choledocholithiasis, sometimes without success. Our study was performed identify the factors predictive of the success of treatment with retrograde endoscopic cholangiopancreatography (ERCP).
Methods
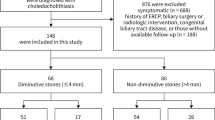
This was a retrospective, case–control study that used data from a biliary disease database at Hospital de Clínicas de Porto Alegre (HCPA). Demographic, clinical, radiological and procedure-related variables were compared between patients with successful biliary clearance after one ERCP procedure (Group 1) and those with unsuccessful biliary clearance after one ERCP procedure (Group 2).
Results
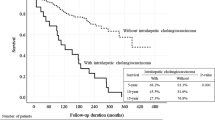
Three hundred twenty patients were included in Group 1, while 254 were included in Group 2. Multivariate analysis showed that older age, previous biliary exploration, elevated serum total bilirubin, choledocholithiasis above the level of the confluence of the hepatic ducts, stones retained in the cystic duct or Mirizzi syndrome, dilatation of the bile duct diagnosed during ERCP, and the need for suprapapillary opening were independently associated with the failure of the first ERCP to achieve bile duct clearance. The performance of imaging at the same institution prior to the procedure and the retention of stones in the duodenal papilla were associated with the success of endoscopic treatment.
Conclusions
The variables identified in this study, when considered in conjunction with the results of previously published studies, can be used to guide the choice of therapeutic methods for patients with choledocholithiasis in the future, given the significant difference in outcomes between the two groups. In the future, a prospective study should be performed to determine whether the same factors are predictive of the success of other methods of treatment (surgical or percutaneous).

Similar content being viewed by others
References
Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE (2019) Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 51:472–491
Ko CW, Lee SP (2002) Epidemiology and natural history of common bile duct stones and prediction of disease. Gastrointest Endosc 56:S165–S169
Möller M, Gustafsson U, Rasmussen F, Persson G, Thorell A (2014) Natural course vs interventions to clear common bile duct stones: data from the Swedish Registry for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). JAMA Surg 149:1008–1013
Copelan A, Kapoor BS (2015) Choledocholithiasis: diagnosis and management. Tech Vasc Interv Radiol 18:244–255
Molvar C, Glaenzer B (2016) Choledocholithiasis: evaluation, treatment, and outcomes. Semin Interv Radiol 33:268–276
European Association for the Study of the Liver (EASL) (2016) EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181
Gao YC, Chen J, Qin Q, Chen H, Wang W, Zhao J, Miao F, Shi X (2017) Efficacy and safety of laparoscopic bile duct exploration versus endoscopic sphincterotomy for concomitant gallstones and common bile duct stones: a meta-analysis of randomized controlled trials. Medicine (Baltim) 96:e7925
Perissat J, Huibregtse K, Keane FBV, Russell RCG, Neoptolemos JP (1994) Management of bile duct stones in the era of laparoscopic cholecystectomy. Br J Surg 81:799–810
Podda M, Polignano FM, Luhmann A, Wilson MS, Kulli C, Tait IS (2016) Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surg Endosc 30:845–861
Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66:765–782
Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Strohmeyer L, Dominitz JA (2010) The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc 71:1–9
Schacher FC, Giongo SM, Teixeira FJP, Mattos ÂZ (2019) Endoscopic retrograde cholangiopancreatography versus surgery for choledocholithiasis—a meta-analysis. Ann Hepatol 18:595–600
Ricci C, Pagano N, Taffurelli G, Pacilio CA, Migliori M, Bazzoli F, Casadei R, Minni F (2018) Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct Calculi: a systematic review and network meta-analysis. JAMA Surg 153:e181167
Poulose BK, Arbogast PG, Holzman MD (2006) National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc 20:186–190
Enochsson L, Sharp N, Gimberg K, Sandblom G (2020) The location of bile duct stones may affect intra- and postoperative cholecystectomy outcome: a population-based registry study. Am J Surg 220:1038–1043
Singh AN, Kilambi R (2018) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc 32:3763–3776
Barr LL, Frame BC, Coulanjon A (1999) Proposed criteria for preoperative endoscopic retrograde cholangiography in candidates for laparoscopic cholecystectomy. Surg Endosc 13:778–781
Gillaspie DB, Davis KA, Schuster KM (2019) Total bilirubin trend as a predictor of common bile duct stones in acute cholecystitis and symptomatic cholelithiasis. Am J Surg 217:98–102
Easler JJ, Sherman S (2015) Endoscopic retrograde cholangiopancreatography for the management of common bile duct stones and gallstone pancreatitis. Gastrointest Endosc Clin N Am 25:657–675
Trieu J, Rogers H, Umar S, Samuel R, Abougergi M, Bazarbashi AN, Desai M, Peluso H, Kröner P, Khan A, Singh S, Bilal M, Berzin T (2020) Increased mortality and costs seen among patients requiring repeat ERCP within the first year. Gastrointest Endosc 91:AB356
Mori T, Sugiyama M, Atomi Y (2006) Gallstone disease: management of intrahepatic stones. Best Pract Res Clin Gastroenterol 20:1117–1137
Ilgit ET, Gürel K, Önal B (2002) Percutaneous management of bile duct stones. Eur J Radiol 43:237–245
Ozcan N, Kahriman G, Mavili E (2011) Percutaneous transhepatic removal of bile duct stones: results of 261 patients. Cardiovasc Interv Radiol 35:621–627
Ramchandani M, Pal P, Reddy DN (2017) Endoscopic management of acute cholangitis as a result of common bile duct stones. Dig Endosc 29(Suppl 2):78–87
Tranter SE, Thompson MH (2003) Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ann R Coll Surg Engl 85:174–177
Lefemine V, Morgan RJ (2011) Spontaneous passage of common bile duct stones in jaundiced patients. Hepatobiliary Pancreat Dis Int 10:209–213
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335:909–918
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102:1781–1788
Vezakis A, Fragulidis G, Polydorou A (2015) Endoscopic retrograde cholangiopancreatography-related perforations: diagnosis and management. World J Gastrointest Endosc 7:1135–1141
Mariani A, Segato S, Anderloni A, Cengia G, Parravicini M, Staiano T, Tontini GE, Lochis D, Cantù P, Manfredi G, Amato A, Bargiggia S, Bernasconi G, Lella F, Canani MB, Beretta P, Ferraris L, Signorelli S, Pantaleo G, Manes G, Testoni PA (2019) Prospective evaluation of ERCP performance in an Italian regional database study. Dig Liver Dis 51(7):978–984
de Araujo TB, Jotz GP, Zaki CH, Mantelli RA, Fernandes VF, Pretto GG, Volkweis BS, Corso CO, Cavazzola LT (2020) Intraoperative cholangiography with filling defects: comparative complication analysis of postoperative transcystic duct (TCD) catheter maintenance. Surg Endosc. https://doi.org/10.1007/s00464-020-08133-y
Almadi MA, Eltayeb M, Thaniah S, Alrashed F, Aljebreen MA, Alharbi OR, Azzam N, Aljebreen AM (2019) Predictors of failure of endoscopic retrograde cholangiography in clearing bile duct stone on the initial procedure. Saudi J Gastroenterol 25:132–138
Üsküdar O, Parlak E, Dışıbeyaz S, Köksal AS, Cıçek B, Kılıç ZM, Ödemiş B, Şaşmaz N (2013) Major predictors for difficult common bile duct stone. Turk J Gastroenterol 24:423–429
Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH (2007) Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc 66:1154–1160
Frazee R, Regner J, Truitt MS, Agrawal V, Swope M, Burlew CC, Dissanaike S, Vangipurum D, Bruns B, O’Meara L, Stivers J, Kwok A, Grover BT, Kothari SN, Cibari C, Dunn J, McIntyre RC Jr, Wright F, Scherer EP, Crane C, Schroeppel TJ, Callaghan E, Gordy S, Todd R (2019) The southwestern surgical congress multi-center trial on suspected common duct stones. Am J Surg 217:1006–1009
Kummerow KL, Shelton J, Phillips S, Holzman MD, Nealon W, Beck W, Sharp K, Poulose BK (2012) Predicting complicated choledocholithiasis. J Surg Res 177:70–74
McHenry L, Lehman G (2006) Difficult bile duct stones. Curr Treat Options Gastroenterol 9:123–132
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Luciano Paludo Marcelino, Stefano Thofehrn, Tatiana Falcão Eyff, Vivian Pierre Bersch and Alessandro Bersch Osvaldt have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marcelino, L.P., Thofehrn, S., Eyff, T.F. et al. Factors predictive of the successful treatment of choledocholithiasis. Surg Endosc 36, 1838–1846 (2022). https://doi.org/10.1007/s00464-021-08463-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08463-5