Abstract
Background
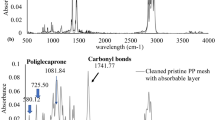
When using a prosthetic material in hernia repair, the behaviour of the mesh at the peritoneal interface is especially important for implant success. Biomaterials developed for their intraperitoneal placement are known as composites and are made up of two different-structure materials, one is responsible for good integration within host tissue and the other is responsible to make contact with the viscera. This study examines the behaviour at the peritoneal level of two composites, the fully degradable Phasix-ST® and the partially degradable Symbotex®. A polypropylene mesh (Optilene®) served as control.
Methods
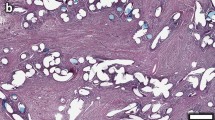
Sequential laparoscopy from 3 to 90 days, in a preclinical model in the New Zealand white rabbit, allowed monitoring adhesion formation. Morphological studies were performed to analyse the neoperitoneum formed in the repair process. Total macrophages were identified by immunohistochemical labelling. To identify the different macrophage phenotypes, complementary DNAs were amplified by qRT-PCR using specific primers for M1 (TNF-α/CXCL9) and M2 (MRC1/IL-10) macrophages.
Results
The percentage of firm and integrated adhesions remained very high in the control group over time. Both composites showed a significant decrease in adhesions at all study times and in qualitative terms were mainly loose. Significant differences were also observed from 7 days onwards between the two composites, increasing the values in Phasix over time. Neoperitoneum thickness for Phasix was significantly greater than those of the other meshes, showing mature and organized neoformed connective tissue.
Immunohistochemically, a significantly higher percentage of macrophages was observed in Symbotex. mRNA expression levels for the M2 repair-type macrophages were highest for Phasix but significant differences only emerged for IL-10.
Conclusions
Fewer adhesions formed to the Symbotex than Phasix implants. Ninety days after implant, total macrophage counts were significantly higher for Symbotex, yet Phasix showed the greater expression of M2 markers related to the tissue repair process.







Similar content being viewed by others
References
Klinge U, Park JK, Klosterhalfen B (2013) The ideal mesh? Pathobiology 80:169–175
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89(5):534–545
Pascual G, Rodriguez M, Gomez-Gil V, García-Honduvilla N, Buján J, Bellón JM (2008) Early tissue incorporation and collagen deposition in lightweight polypropylene meshes: bioassay in an experimental model of ventral hernia. Surgery 144(3):427–435
Yilmaz I, Karakas DO, Sucullu I, Ozdemir Y, Yucel E (2013) A rare cause of mechanical bowel obstruction: mesh migration. Hernia 17(2):267–269
Aziz F, Zaeem M (2014) Chronic abdominal pain secondary to mesh erosion into ceacum following incisional hernia repair: a case report and literature review. J Clin Med Res 6(2):153–155
Ott V, Groebli Y, Schneider R (2005) Late intestinal fistula formation after incisional hernia using intraperitoneal mesh. Hernia 9(1):103–104
Moussi A, Daldoul S, Bourguiba B, Othmani D, Zaouche A (2012) Gas gangrene of the abdominal wall due to late-onset enteric fistula after polyester mesh repair of an incisional hernia. Hernia 16(2):215–217
Arnold MR, Kao AM, Otero J, Marx JE, Augenstein VA, Sing RF, Colavita PD, Kercher K, Henniford BT (2020) Mesh fistula after ventral hernia repair: what is the optimal management? Surgery 167(3):590–597
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1:5–8
Deeken CR, Faucher KM, Matthews BD (2012) A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc 26(2):566–575
Bellón JM, García-Honduvilla N, López R, Corrales C, Jurado F, Buján J (2003) In vitro mesothelialization of prosthetic materials designed for the repair of abdominal wall defects. J Mater Sci Mater Med 14(4):359–364
Klopfleisch R (2016) Macrophage reaction against biomaterials in the mouse model—phenotypes, functions and markers. Acta Biomater 43:3–13
Cohen HB, Mosser DM (2013) Extrinsic and intrinsic control of macrophage inflammatory responses. J Leukoc Biol 94(5):913–919
Roszer T (2015) Understanding the mysterious M2 macrophage through activation markers and effector mechanisms. Mediators Inflamm. https://doi.org/10.1155/2015/816460
Badylak SF, Valentin JE, Ravindra AK, McCabe GP, Stewart-Akers AM (2008) Macrophage phenotype as a determinant of biologic scaffold remodelling. Tissue Eng A 14(11):1835–1842
Brown BN, Sicari BM, Badylak SF (2014) Rethinking regenerative medicine: a macrophage-centered approach. Front Immunol 5:510
Bellon JM, Contreras LA, Bujan J, Jurado F (1996) Effect of phosphatidylcholine on the process of peritoneal adhesion following implantation of a polypropylene mesh prosthesis. Biomaterials 17(14):1369–1372
Walker AP, Henderson J, Condon RE (1993) Double-layer prostheses for repair of abdominal wall defects in a rabbit model. J Surg Res 55(1):32–37
Amid PK, Shulman AG, Lichtenstein IL, Sostrin S, Young J, Hakakha M (1994) Experimental evaluation of a new composite mesh with the selective property of incorporation to the abdominal wall without adhering to the intestines. J Biomed Mater Res 28(3):373–375
Baptista ML, Bonsack ME, Delaney JP (2000) Seprafilm reduces adhesions to polypropylene mesh. Surgery 128(1):86–92
Szabo A, Haj M, Waxsman I, Eitan A (2000) Evaluation of seprafilm and amniotic membrane as adhesion prophylaxis in mesh repair of abdominal wall hernia in rats. Eur Surg Res 32(2):125–128
Greenawalt KE, Butler TJ, Rowe EA, Finneral AC, Garlick DS, Burns JW (2000) Evaluation of sepramesh biosurgical composite in a rabbit hernia repair model. J Surg Res 94(2):92–98
Shapiro L, Holste JL, Muench T, diZerega G (2015) Rapid reperitonealization and wound healing in a preclinical model of abdominal trauma repair with a composite mesh. Int J Surg 22:86–91
Ar’Rajab A, Ahrén B, Rozga J, Bengmark S (1991) Phosphatidylcholine prevents postoperative peritoneal adhesions: an experimental study in the rat. J Surg Res 50(3):212–215
Holmdahl L, Risberg B, Beck DE, Burns JW, Chegini N, Di Zerega GS, Ellis H (1997) Adhesions: pathogenesis and prevention. Eur J Surg Suppl 577:56–62
Felemovicius I, Bonsack ME, Hegerman G, Delaney JP (2004) Prevention of adhesions to polypropylene mesh. J Am Coll Surg 198(4):543–548
Brochhausen C, Schmitt VH, Rajab TK, Planck CN, Krämer B, Tapprich C, Wallwiener M, Hierlemann H, Planck H, Kirkpatrick CJ (2012) Mesothelial morphology and organisation after peritoneal treatment with solid and liquid adhesion barriers—a scanning electron microscopical study. J Mater Sci Mater Med 23(8):1931–1939
Arnaud JP, Hennekinne-Mucci S, Pessaux P, Tuech JJ, Aube C (2003) Ultrasound detection of visceral adhesions after intraperitoneal ventral hernia treatment: a comparative study of protected versus unprotected meshes. Hernia 7(2):85–88
Balique JG, Benchetrit S, Bouillot JL, Flament JB, Gouillat C, Jarsaillon P, Lepère M, Mantion G, Arnaud JP, Magne E, Brunetti F (2005) Intraperitoneal treatment of incisional and umbilical hernias using an innovative composite mesh: four-year results of a prospective multicenter clinical trial. Hernia 9(1):68–74
Moreno-Egea A, Bustos JAC, Girela E, Aguayo-Albasini JL (2010) Long-term results of laparoscopic repair of incisional hernias using an intraperitoneal composite mesh. Surg Endosc 24(2):359–365
Chelala E, Debardemaeker Y, Elias B, Charara F, Dessily M, Alle JL (2010) Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: adhesion and recurrence analysis. Hernia 14(2):123–129
Celdrán A, García-Ureña MA, Bazire P, Marijuan JL (1996) The use of omentum in mesh repair of ventral hernias. Am Surg 62(6):443–445
Sorour MA (2014) Interposition of the omentum and/or the peritoneum in the emergency repair of large ventral hernias with polypropylene mesh. Int J Surg 12(6):578–586
Hasbahceci M, Basak F (2014) Interposition of the hernia sac as a protective layer in repair of giant incisional hernia with polypropylene mesh. Surg Today 44(2):227–232
D´Amore L, Ceci F, Mattia S, Fabbi M, Negro P, Gossetti F (2017) Adhesion prevention in ventral hernia repair: an experimental study comparing three lightweight porous meshes recommended for intraperitoneal use. Hernia 21(1):115–123
Boersema GS, Grotenhuis N, Bayon Y, Lange JF, Bastiaansen-Jenniskens YM (2016) The effect of biomaterials used for tissue regeneration purposes on polarization of macrophages. Biores Open Access 5(1):6–14
Brown BN, Badylak SF (2013) Expanded applications, shifting paradigms and an improved understanding of host-biomaterial interactions. Acta Biomater 9(2):4948–4955
Sridharan R, Cavanagh B, Cameron AR, Kelly DJ, O’Brien FJ (2019) Material stiffness influences the polarization state, function and migration mode of macrophages. Acta Biomater 89:47–59
Grotenhuis N, Vd Toom HF, Kops N, Bayon Y, Deerenberg EB, Mulder IM, van Osch GJ, Lange JF, Bastiaansen-Jenniskens YM (2014) In vitro model to study the biomaterial-dependent reaction of macrophages in an inflammatory environment. BJS 101(8):983–992
Deeken CR, Matthews BD (2013) Characterization of the mechanical strength, resorption properties, and histologic characteristics of a fully absorbable material (poly-4-hydroxybutyrate-PHASIX Mesh) in a Porcine Model of hernia repair. ISRN Surg. https://doi.org/10.1155/2013/238067
Martin DP, Badhwar A, Shah DV, Rizk S, Eldridge SN, Gagne DH, Ganatra A, Darois RE, Williams SF, Tai HC, Scott JR (2013) Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J Surg Res 184(2):766–773
Scott JR, Deeken CR, Martindale RG, Rosen MJ (2016) Evaluation of a fully absorbable poly-4-hydroxybutyrate/absorbable barrier composite mesh in a porcine model of ventral hernia repair. Surg Endosc 30(9):3691–3701
Wolf MT, Dearth CL, Ranallo CA, LoPresti ST, Carey LE, Daly KA, Brown BN, Badylak SF (2014) Macrophage polarization in response to ECM coated polypropylene mesh. Biomaterials 35(25):6838–6849
Hong GS, Schwandt T, Stein K, Schneiker B, Kummer MP, Heneka MT, Kitamura K, Kalff JC, Wehner S (2015) Effects of macrophage-dependent peroxisome proliferator-activated receptor γ signalling on adhesion formation after abdominal surgery in an experimental model. Br J Surg 102(12):1506–1516
Funding
The study was supported by Grant “SAF2017-89481-P” from the Spanish Ministry of Economy and Competitiveness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Gemma Pascual, Selma Benito-Martínez, Marta Rodríguez, Bárbara Pérez-Köhler, Francisca García-Moreno and Juan M. Bellón have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pascual, G., Benito-Martínez, S., Rodríguez, M. et al. Behaviour at the peritoneal interface of next-generation prosthetic materials for hernia repair. Surg Endosc 36, 579–590 (2022). https://doi.org/10.1007/s00464-021-08320-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08320-5