Abstract
Background
Double-balloon endoscopy (DBE) provides both diagnosis and treatment in overt obscure gastrointestinal bleeding (OGIB). The aim of this study was to evaluate the rebleeding rate after DBE.
Methods
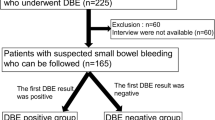
This retrospective review was conducted between January 2006 and July 2018, 166 patients with overt OGIB who underwent DBE were enrolled. Therapeutic intervention was defined as endoscopic treatment, embolization, or surgery. Primary outcome was rebleeding rate after DBE. The patients were divided into 3 groups based on their DBE; (1) positive DBE requiring therapeutic intervention (G1), (2) positive DBE without therapeutic intervention required (G2) and (3) negative DBE (G3). Cumulative incidence of rebleeding was estimated using the Kaplan–Meier method. Cox regression was used to assess the association of DBE with rebleeding risk. This study was approved by our Institutional Review Board.
Results
Sixty-eight patients (41%) were categorized in G1, 34 patients (20%) in G2 and 64 patients (39%) in G3. Overall rebleeding occurred in 24 patients (15%). The cumulative incidence of rebleeding for G1 was the lowest. The 1-year and 2-year cumulative probability of developing rebleeding after DBE in G1 were 3.5% and 3.5%, 8.2% and 14.0% in G2, and 18.2% and 20.6% in G3, respectively (p = 0.02). After adjusting for bleeding severity and comorbidities, patients with positive DBE requiring therapeutic intervention had a significantly lower rate of rebleeding when compared with patients who did not receive intervention (hazard ratio 0.17; 95% CI 0.03–0.90).
Conclusion
DBE-guided therapeutic intervention was associated with a lower risk of rebleeding when compared with those with negative and positive DBE without therapeutic intervention. One-fifth of patients with overt OGIB had false negative after DBE.

Similar content being viewed by others
References
ASGE Standards of Practice Committee, Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C, Fukami N, Harrison ME, Ikenberry SO, Jain R, Jue T, Khan K, Maple JT, Strohmeyer L, Sharaf R, Dominitz JA (2010) The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc 72:471–479
Gerson LB, Fidler JL, Cave DR, Leighton JA (2015) ACG Clinical guideline: diagnosis and management of small bowel bleeding. Am J Gastroenterol 110:1265–1287 (quiz 1288)
Shinozaki S, Yamamoto H, Yano T, Sunada K, Miyata T, Hayashi Y, Arashiro M, Sugano K (2010) Long-term outcome of patients with obscure gastrointestinal bleeding investigated by double-balloon endoscopy. Clin Gastroenterol Hepatol 8:151–158
Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, De Franchis R (2004) Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology 126:643–653
Gerson LB, Batenic MA, Newsom SL, Ross A, Semrad CE (2009) Long-term outcomes after double-balloon enteroscopy for obscure gastrointestinal bleeding. Clin Gastroenterol Hepatol 7:664–669
Aniwan S, Viriyautsahakul V, Rerknimitr R, Angsuwatcharakon P, Kongkam P, Treeprasertsuk S, Kullavanijaya P (2014) Urgent double balloon endoscopy provides higher yields than non-urgent double balloon endoscopy in overt obscure gastrointestinal bleeding. Endosc Int Open 2:E90–95
Fujimori S, Seo T, Gudis K, Tanaka S, Mitsui K, Kobayashi T, Ehara A, Yonezawa M, Tatsuguchi A, Sakamoto C (2007) Diagnosis and treatment of obscure gastrointestinal bleeding using combined capsule endoscopy and double balloon endoscopy: 1-year follow-up study. Endoscopy 39:1053–1058
Fujita M, Manabe N, Honda K, Tarumi K, Murao T, Katada S, Kimura Y, Matsumoto H, Kamada T, Shiotani A, Hata J, Haruma K (2010) Long-term outcome after double-balloon endoscopy in patients with obscure gastrointestinal bleeding. Digestion 82:173–178
Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P, Barbaro F, Cellier C, Charton JP, Delvaux M, Despott EJ, Domagk D, Klein A, McAlindon M, Rosa B, Rowse G, Sanders DS, Saurin JC, Sidhu R, Dumonceau JM, Hassan C, Gralnek IM (2015) Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 47:352–376
Hashimoto R, Matsuda T, Nakahori M (2019) False-negative double-balloon enteroscopy in overt small bowel bleeding: long-term follow-up after negative results. Surg Endosc 33:2635–2641
Yano T, Yamamoto H, Sunada K, Miyata T, Iwamoto M, Hayashi Y, Arashiro M, Sugano K (2008) Endoscopic classification of vascular lesions of the small intestine (with videos). Gastrointest Endosc 67:169–172
Shinozaki S, Yano T, Sakamoto H, Sunada K, Hayashi Y, Sato H, Lefor AK, Yamamoto H (2015) Long-term outcomes in patients with overt obscure gastrointestinal bleeding after negative double-balloon endoscopy. Dig Dis Sci 60:3691–3696
Sun B, Rajan E, Cheng S, Shen R, Zhang C, Zhang S, Wu Y, Zhong J (2006) Diagnostic yield and therapeutic impact of double-balloon enteroscopy in a large cohort of patients with obscure gastrointestinal bleeding. Am J Gastroenterol 101:2011–2015
Samaha E, Rahmi G, Landi B, Lorenceau-Savale C, Malamut G, Canard JM, Bloch F, Jian R, Chatellier G, Cellier C (2012) Long-term outcome of patients treated with double balloon enteroscopy for small bowel vascular lesions. Am J Gastroenterol 107:240–246
Rahmi G, Samaha E, Vahedi K, Delvaux M, Gay G, Lamouliatte H, Filoche B, Saurin JC, Ponchon T, Rhun ML, Coumaros D, Bichard P, Maniere T, Lenain E, Chatellier G, Cellier C (2014) Long-term follow-up of patients undergoing capsule and double-balloon enteroscopy for identification and treatment of small-bowel vascular lesions: a prospective, multicenter study. Endoscopy 46:591–597
May A, Friesing-Sosnik T, Manner H, Pohl J, Ell C (2011) Long-term outcome after argon plasma coagulation of small-bowel lesions using double-balloon enteroscopy in patients with mid-gastrointestinal bleeding. Endoscopy 43:759–765
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Satimai Aniwan, Vichai Viriyautsahakul, Thanawat Luangsukrerk, Phonthep Angsuwatcharakon, Panida Piyachaturawat, Pradermchai Kongkam, Sombat Treeprasertsuk, Pinit Kullavanijaya, Rungsun Rerknimitr and Ms. Natanong Kongtab have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aniwan, S., Viriyautsahakul, V., Luangsukrerk, T. et al. Low rate of recurrent bleeding after double-balloon endoscopy-guided therapy in patients with overt obscure gastrointestinal bleeding. Surg Endosc 35, 2119–2125 (2021). https://doi.org/10.1007/s00464-020-07615-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07615-3