Abstract
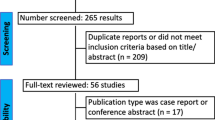
Dysphagia is one of the most frequent sequelae of stroke. It can result in various complications such as malnutrition, dehydration, aspiration pneumonia, and poor rehabilitation outcomes. Repetitive transcranial magnetic stimulation (rTMS) has been reported to improve dysphagia after a stroke; however, effective treatment protocols have not been established yet. We evaluated the effect of the following rTMS parameters on post-stroke dysphagia: stimulation frequency [high frequency (≥ 3 Hz) or low frequency (1 Hz)] and stimulation site (ipsilesional or contralesional mylohyoid cortex). Outcomes were measured immediately, at 3 weeks, and at 4 weeks after the rTMS session. The PubMed, SCOPUS, Embase, and Cochrane Library databases were systematically searched for relevant studies published between January 01, 1980, and December 13, 2021. Randomized controlled trials on the effects of rTMS on post-stroke dysphagia were included. Six studies were finally included in the analysis. The selected studies included 158 patients (rTMS group: 81 patients; sham group: 77 patients). Regarding the effect of high-frequency rTMS on the ipsilesional cortex, the standardized swallowing assessment (SSA) scores showed significant improvement after rTMS sessions immediately and at 4 weeks [immediate: P = 0.02, standard mean difference (SMD) = − 0.61, 95% confidence interval (CI) = − 1.14 to − 0.08; 4 weeks: P = 0.006, SMD = − 0.74, 95% CI = − 1.27 to − 0.21]; however, there was no significant reduction in the Penetration–Aspiration Scale (PAS) scores between the rTMS and sham groups (immediate: P = 0.43, SMD = 0.25, 95% CI = − 0.36, 0.86; 3 weeks: P = 0.39, SMD = 0.37, 95% CI = − 0.47 to 1.22). After low-frequency rTMS on the ipsilesional cortex, a significantly greater improvement in the SSA scores was found in the rTMS group than in the sham group, both immediately and at 4 weeks after rTMS sessions (immediate: P = 0.03, SMD = − 0.59, 95% CI = − 1.12 to − 0.06; 4 weeks: P = 0.001, SMD = − 0.92, 95% CI = − 1.48 to − 0.37). In addition, immediately after the rTMS sessions, the PAS scores were significantly reduced in the rTMS group than in the sham group (P = 0.047, SMD = − 0.60, 95% CI = − 1.19 to − 0.01). However, at 4 weeks after rTMS sessions, there was no significant reduction in the PAS scores in the rTMS group compared to the sham group (P = 0.48, SMD = − 0.19, 95% CI = − 0.71 to 0.33). Both high-frequency rTMS of the ipsilesional cortex and low-frequency rTMS of the contralesional cortex improved some measurements of the swallowing function in stroke patients immediately and at 4 weeks after treatment.




Similar content being viewed by others
References
Chang MC, Kwak SG, Chun MH. Dysphagia in patients with isolated pontine infarction. Neural Regen Res. 2018;13(12):2156–9.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63.
Yang S, Choo YJ, Chang MC. The preventive effect of dysphagia screening on pneumonia in acute stroke patients: a systematic review and meta-analysis. Healthcare (Basel). 2021;9(12):1764.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10(10):CD000323.
Byeon H. Combined effects of NMES and Mendelsohn maneuver on the swallowing function and swallowing-quality of life of patients with stroke-induced sub-acute swallowing disorders. Biomedicines. 2020;8(1):12.
Chang MC, Park S, Cho JY, Lee BJ, Hwang JM, Kim K, Park D. Comparison of three different types of exercises for selective contractions of supra- and infrahyoid muscles. Sci Rep. 2021;11(1):7131.
Speyer R, Sutt AL, Bergström L, Hamdy S, Pommée T, Balaguer M, Kaale A, Cordier R. Neurostimulation in people with oropharyngeal dysphagia: a systematic review and meta-analysis of randomised controlled trials—Part II: brain neurostimulation. J Clin Med. 2022;11(4):993.
Kim WS, Paik NJ. Safety review for clinical application of repetitive transcranial magnetic stimulation. Brain Neurorehabil. 2021;14(1): e6.
Bai Z, Zhang J, Fong KNK. Effects of transcranial magnetic stimulation in modulating cortical excitability in patients with stroke: a systematic review and meta-analysis. J Neuroeng Rehabil. 2022;19(1):24.
Cheng IKY, Chan KMK, Wong CS, Li LSW, Chiu KMY, Cheung RTF, Yiu EML. Neuronavigated high-frequency repetitive transcranial magnetic stimulation for chronic post-stroke dysphagia: a randomized controlled study. J Rehabil Med. 2017;49(6):475–81.
Du J, Yang F, Liu L, Hu J, Cai B, Liu W, Xu G, Liu X. Repetitive transcranial magnetic stimulation for rehabilitation of poststroke dysphagia: a randomized, double-blind clinical trial. Clin Neurophysiol. 2016;127(3):1907–13.
Khedr EM, Abo-Elfetoh N. Therapeutic role of rTMS on recovery of dysphagia in patients with lateral medullary syndrome and brainstem infarction. J Neurol Neurosurg Psychiatry. 2010;81(5):495–9.
Khedr EM, Abo-Elfetoh N, Rothwell JC. Treatment of post-stroke dysphagia with repetitive transcranial magnetic stimulation. Acta Neurol Scand. 2009;119(3):155–61.
Kim L, Chun MH, Kim BR, Lee SJ. Effect of repetitive transcranial magnetic stimulation on patients with brain injury and dysphagia. Ann Rehabil Med. 2011;35(6):765–71.
Lim KB, Lee HJ, Yoo J, Kwon YG. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Ann Rehabil Med. 2014;38(5):592–602.
Park E, Kim MS, Chang WH, Oh SM, Kim YK, Lee A, Kim YH. Effects of bilateral repetitive transcranial magnetic stimulation on post-stroke dysphagia. Brain Stimul. 2017;10(1):75–82.
Park JW, Oh JC, Lee JW, Yeo JS, Ryu KH. The effect of 5 Hz high-frequency rTMS over contralesional pharyngeal motor cortex in post-stroke oropharyngeal dysphagia: a randomized controlled study. Neurogastroenterol Motil. 2013;25(4):324-e250.
Ünlüer NÖ, Temuçin ÇM, Demir N, Serel Arslan S, Karaduman AA. Effects of low-frequency repetitive transcranial magnetic stimulation on swallowing function and quality of life of post-stroke patients. Dysphagia. 2019;34(3):360–71.
Zhang C, Zheng X, Lu R, Yun W, Yun H, Zhou X. Repetitive transcranial magnetic stimulation in combination with neuromuscular electrical stimulation for treatment of post-stroke dysphagia. J Int Med Res. 2019;47(2):662–72.
Zhong L, Rao J, Wang J, Li F, Peng Y, Liu H, Zhang Y, Wang P. Repetitive transcranial magnetic stimulation at different sites for dysphagia after stroke: a randomized, observer-blind clinical trial. Front Neurol. 2021;12: 625683.
Cheng I, Sasegbon A, Hamdy S. Effects of neurostimulation on poststroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2021;24(8):1388–401.
Chiang CF, Lin MT, Hsiao MY, Yeh YC, Liang YC, Wang TG. Comparative efficacy of noninvasive neurostimulation therapies for acute and subacute poststroke dysphagia: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2019;100(4):739-50.e4.
Li L, Huang H, Jia Y, Yu Y, Liu Z, Shi X, Wang F. Systematic review and network meta-analysis of noninvasive brain stimulation on dysphagia after stroke. Neural Plast. 2021;2021:3831472.
Li H, Li L, Zhang R, Huang X, Lin J, Liu C, Lou W. Effectiveness of repetitive transcranial magnetic stimulation on poststroke dysphagia: a meta-analysis of randomized-controlled trials. Int J Rehabil Res. 2022;45(2):109–17 (Epub ahead of print).
Liao X, Xing G, Guo Z, Jin Y, Tang Q, He B, McClure MA, Liu H, Chen H, Mu Q. Repetitive transcranial magnetic stimulation as an alternative therapy for dysphagia after stroke: a systematic review and meta-analysis. Clin Rehabil. 2017;31(3):289–98.
Pisegna JM, Kaneoka A, Pearson WG Jr, Kumar S, Langmore SE. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol. 2016;127(1):956–68.
Wang T, Dong L, Cong X, Luo H, Li W, Meng P, Wang Q. Comparative efficacy of non-invasive neurostimulation therapies for poststroke dysphagia: a systematic review and meta-analysis. Neurophysiol Clin. 2021;51(6):493–506.
Zhu Y, Gu L. Noninvasive brain stimulation for poststroke dysphagia: a meta-analysis for randomized controlled trials. Eur Neurol. 2021;85(1):1–8.
Daskalakis ZJ, Christensen BK, Fitzgerald PB, Roshan L, Chen R. The mechanisms of interhemispheric inhibition in the human motor cortex. J Physiol. 2002;543(Pt 1):317–26.
Di Lazzaro V, Oliviero A, Profice P, Insola A, Mazzone P, Tonali P, Rothwell JC. Direct demonstration of interhemispheric inhibition of the human motor cortex produced by transcranial magnetic stimulation. Exp Brain Res. 1999;124(4):520–4.
Ferbert A, Priori A, Rothwell JC, Day BL, Colebatch JG, Marsden CD. Interhemispheric inhibition of the human motor cortex. J Physiol. 1992;453:525–46.
Gerloff C, Cohen LG, Floeter MK, Chen R, Corwell B, Hallett M. Inhibitory influence of the ipsilateral motor cortex on responses to stimulation of the human cortex and pyramidal tract. J Physiol. 1998;510(Pt 1):249–59.
Boroojerdi B, Diefenbach K, Ferbert A. Transcallosal inhibition in cortical and subcortical cerebral vascular lesions. J Neurol Sci. 1996;144(1–2):160–70.
Murase N, Duque J, Mazzocchio R, Cohen LG. Influence of interhemispheric interactions on motor function in chronic stroke. Ann Neurol. 2004;55(3):400–9.
Du J, Yang F, Hu J, Hu J, Xu Q, Cong N, Zhang Q, Liu L, Mantini D, Zhang Z, Lu G, Liu X. Effects of high- and low-frequency repetitive transcranial magnetic stimulation on motor recovery in early stroke patients: evidence from a randomized controlled trial with clinical, neurophysiological and functional imaging assessments. Neuroimage Clin. 2019;21: 101620.
Long H, Wang H, Zhao C, Duan Q, Feng F, Hui N, Mao L, Liu H, Mou X, Yuan H. Effects of combining high- and low-frequency repetitive transcranial magnetic stimulation on upper limb hemiparesis in the early phase of stroke. Restor Neurol Neurosci. 2018;36(1):21–30.
Sasaki N, Kakuda W, Abo M. Bilateral high- and low-frequency rTMS in acute stroke patients with hemiparesis: a comparative study with unilateral high-frequency rTMS. Brain Inj. 2014;28(13–14):1682–6.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Erlbaum; 1988.
Casula EP, Pellicciari MC, Bonnì S, Spanò B, Ponzo V, Salsano I, Giulietti G, Martino Cinnera A, Maiella M, Borghi I, Rocchi L, Bozzali M, Sallustio F, Caltagirone C, Koch G. Evidence for interhemispheric imbalance in stroke patients as revealed by combining transcranial magnetic stimulation and electroencephalography. Hum Brain Mapp. 2021;42(5):1343–58.
Cirillo G, Di Pino G, Capone F, Ranieri F, Florio L, Todisco V, Tedeschi G, Funke K, Di Lazzaro V. Neurobiological after-effects of non-invasive brain stimulation. Brain Stimul. 2017;10(1):1–18.
Smith MC, Stinear CM. Transcranial magnetic stimulation (TMS) in stroke: ready for clinical practice? J Clin Neurosci. 2016;31:10–4.
Cortes M, Black-Schaffer RM, Edwards DJ. Transcranial magnetic stimulation as an investigative tool for motor dysfunction and recovery in stroke: an overview for neurorehabilitation clinicians. Neuromodulation. 2012;15(4):316–25.
Demirtas-Tatlidede A, Alonso-Alonso M, Shetty RP, Ronen I, Pascual-Leone A, Fregni F. Long-term effects of contralesional rTMS in severe stroke: safety, cortical excitability, and relationship with transcallosal motor fibers. NeuroRehabilitation. 2015;36(1):51–9.
Saur D, Lange R, Baumgaertner A, Schraknepper V, Willmes K, Rijntjes M, Weiller C. Dynamics of language reorganization after stroke. Brain. 2006;129(Pt 6):1371–84.
Teismann IK, Suntrup S, Warnecke T, Steinsträter O, Fischer M, Flöel A, Ringelstein EB, Pantev C, Dziewas R. Cortical swallowing processing in early subacute stroke. BMC Neurol. 2011;11:34.
Hamdy S, Aziz Q, Rothwell JC, Singh KD, Barlow J, Hughes DG, Tallis RC, Thompson DG. The cortical topography of human swallowing musculature in health and disease. Nat Med. 1996;2(11):1217–24.
Hamdy S, Aziz Q, Rothwell JC, Power M, Singh KD, Nicholson DA, et al. Recovery of swallowing after dysphagic stroke relates to functional reorganization in the intact motor cortex. Gastroenterology. 1998;115(5):1104–12.
Funding
This study received no external funding. The present study was supported by a National Research Foundation of Korea grand funded by the Korean government (grant no. NRF- 2019M3E5D1A02068106).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hsiao, MY., Choo, Y.J., Liu, IC. et al. Effect of Repetitive Transcranial Magnetic Stimulation on Post-stroke Dysphagia: A Meta-analysis of Stimulation Frequency, Stimulation Site, and Timing of Outcome Measurement. Dysphagia 38, 435–445 (2023). https://doi.org/10.1007/s00455-022-10483-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10483-9