Abstract
Objective
To analyze the correlation between bone morphogenetic protein (BMP) antagonist Gremlin 1 (GREM1), Thrombospondin-2 (THBS2) and immune cell infiltration in non-small cell lung cancer (NSCLC) and the related clinical significance.
Methods
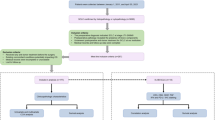
A total of 150 NSCLC patients admitted to our hospital during May 2019–January 2022 were picked. The expression of GREM1 and THBS2 and the infiltration of immune cells in tumor tissues were detected through immunohistochemistry (IHC). These objects were graded as GREM1-positive group (n = 97), GREM1-negative group (n = 53), THBS2-positive group (n = 102) and THBS2-negative group (n = 48) according to the expression of GREM1 and THBS2. The correlation between the expression of GREM1 and THBS2 with immune cell infiltration and clinicopathological indicators was analyzed. Kaplan–Meier survival analysis was adopted to analyze the relationship between the expression of GREM1 and THBS2 and the prognosis in NSCLC tissues. The overall progression-free survival (PFS) of the two groups were compared by log-rank test.
Results
The results of IHC showed that the positive expression rate of GREM1 was 64.67% (97/150) in cancer tissues and 36.00% (54/150) in adjacent tissues. The positive expression rate of THBS2 was 68.00% (102/150) in cancer tissues and 25.33% (38/150) in adjacent tissues. The positive expression rate of GREM1 and THBS2 in cancer tissues was both much higher than that in adjacent tissues (P < 0.01). GREM1-positive group had much higher proportion of tumor diameter ≥ 2 cm, stage III–IV and lymph-node metastasis than GREM1-negative group (P < 0.05). THBS2-positive group had markedly higher proportion of tumor diameter ≥ 2 cm, stage III–IV, lymph-node metastasis and high differentiation than THBS2-negative group (P < 0.01). GREM1-positive group had much higher level of CD3 + T, and sharply lower level of CD8 + T and CD11c + DCs than GREM1-negative group (P < 0.01). THBS2-positive group had much higher level of CD3 + T, and sharply lower level of CD8 + T and CD11c + DCs than THBS2-negative group (P < 0.01). According to Kaplan–Meier survival analysis, the overall median progression-free survival (PFS) was 7.45 months. Log-rank test showed that NSCLC patients with positive GREM1 and THBS2 had much shorter PFS than negative patients (P < 0.01). Log-rank test showed that the expression of GREM1 and THBS2 was related to the PFS of patients (P < 0.01).
Conclusion
GREM1 and THBS2 were highly expressed in NSCLC tissues and acted as pro-oncogenes in the development and progression of NSCLC, which aggravated the disease by mediating immune cell infiltration.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Alexander M, Kim SY, Cheng H (2020) Update 2020: management of non-small cell lung cancer. Lung 198(6):897–907
Broderick SR (2020) Adjuvant and neoadjuvant immunotherapy in non-small cell lung cancer. Thorac Surg Clin 30(2):215–220
Duma N, Santana-Davila R, Molina JR (2019) Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc 94(8):1623–1640
Hsu ML, Naidoo J (2020) Principles of immunotherapy in non-small cell lung cancer. Thorac Surg Clin 30(2):187–198
Jiang YM, Yu DL, Hou GX, Jiang JL, Zhou Q, Xu XF (2019) Serum thrombospondin-2 is a candidate diagnosis biomarker for early non-small-cell lung cancer. Biosci Rep. https://doi.org/10.1042/BSR20190476
Jonna S, Subramaniam DS (2019) Molecular diagnostics and targeted therapies in non-small cell lung cancer (NSCLC): an update. Discov Med 27(148):167–170
Kan J, Fu B, Zhou R, Zhou D, Huang Y, Zhao H, Zhang Y, Rong Y, Dong J, Xia L, Liu S, Huang Q, Wang N, Ning N, Zhang B, Zhang E (2022) He-Chan Pian inhibits the metastasis of non-small cell lung cancer via the miR-205-5p-mediated regulation of the GREM1/Rap1 signaling pathway. Phytomedicine 94:153821
Koppens MAJ, Davis H, Valbuena GN, Mulholland EJ, Nasreddin N, Colombe M, Antanaviciute A, Biswas S, Friedrich M, Lee L, Oxford IBD Cohort Investigators, Wang LM, Koelzer VH, East JE, Simmons A, Winton DJ, Leedham SJ (2021) Bone morphogenetic protein pathway antagonism by grem1 regulates epithelial cell fate in intestinal regeneration. Gastroenterology 161(1):239–254
Kozumi K, Kodama T, Murai H, Sakane S, Govaere O, Cockell S, Motooka D, Kakita N, Yamada Y, Kondo Y, Tahata Y, Yamada R, Hikita H, Sakamori R, Kamada Y, Daly AK, Anstee QM, Tatsumi T, Morii E, Takehara T (2021) Transcriptomics identify thrombospondin-2 as a biomarker for NASH and advanced liver fibrosis. Hepatology 74(5):2452–2466. https://doi.org/10.1002/hep.31995. (Epub 2021 Aug 21 PMID: 34105780; PMCID: PMC8596693)
Lan L, Evan T, Li H, Hussain A, Ruiz EJ, Zaw Thin M, Ferreira RMM, Ps H, Riising EM, Zen Y, Almagro J, Ng KW, Soro-Barrio P, Nelson J, Koifman G, Carvalho J, Nye EL, He Y, Zhang C, Sadanandam A, Behrens A (2022) GREM1 is required to maintain cellular heterogeneity in pancreatic cancer. Nature 607(7917):163–168
Liu SY, Wu YL (2020) Tislelizumab: an investigational anti-PD-1 antibody for the treatment of advanced non-small cell lung cancer (NSCLC). Expert Opin Investig Drugs 29(12):1355–1364
Reck M, Remon J, Hellmann MD (2022) First-line immunotherapy for non-small-cell lung cancer. J Clin Oncol 40(6):586–597
Sun Q, Qi X, Zhang W, Li X (2021) Knockdown of circRNA_0007534 suppresses the tumorigenesis of cervical cancer via miR-206/GREM1 axis. Cancer Cell Int 21(1):54
Udgata S, Takenaka N, Bamlet WR, Oberg AL, Yee SS, Carpenter EL, Herman D, Kim J, Petersen GM, Zaret KS (2021) THBS2/CA19-9 detecting pancreatic ductal adenocarcinoma at diagnosis underperforms in prediagnostic detection: implications for biomarker advancement. Cancer Prev Res (phila) 14(2):223–232
Wu K, Lin K, Li X, Yuan X, Xu P, Ni P, Xu D (2020) Redefining tumor-associated macrophage subpopulations and functions in the tumor microenvironment. Front Immunol 4(11):1731
Xie D, Hu J, Wu T, Cao K, Luo X (2021) Four immune-related genes (FN1, UGCG, CHPF2 and THBS2) as potential diagnostic and prognostic biomarkers for carbon nanotube-induced mesothelioma. Int J Gen Med 29(14):4987–5003
Yang H, Sun B, Fan L, Ma W, Xu K, Hall SRR, Wang Z, Schmid RA, Peng RW, Marti TM, Gao W, Xu J, Yang W, Yao F (2022a) Multi-scale integrative analyses identify THBS2+ cancer-associated fibroblasts as a key orchestrator promoting aggressiveness in early-stage lung adenocarcinoma. Theranostics 12(7):3104–3130
Yang S, Zhang Y, Hua Y, Cui M, Wang M, Gao J, Liu Q, Liao Q (2022b) GREM1 is a novel serum diagnostic marker and potential therapeutic target for pancreatic ductal adenocarcinoma. Front Oncol 26(12):968610
Yang Z, Wu H, Zhang K, Rao S, Qi S, Liu M, Chen Y, Wang Y (2022c) Circ_0007580 knockdown strengthens the radiosensitivity of non-small cell lung cancer via the miR-598-dependent regulation of THBS2. Thorac Cancer 13(5):678–689
Funding
No external funding received to conduct this study.
Author information
Authors and Affiliations
Contributions
YFB and ESY conceived the idea and conceptualised the study. YFB and ESY collected the data. ESY and NW analysed the data. YFB and NW drafted the manuscript, then NW reviewed the manuscript. All authors read and approved the final draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
This study was conducted with approval from the Ethics Committee of our hospital. This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bao, Y., Yan, E. & Wang, N. Evaluation of GREM1 and THBS2 as prognostic markers in in non-small cell lung cancer. J Cancer Res Clin Oncol 149, 7849–7856 (2023). https://doi.org/10.1007/s00432-023-04746-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04746-7