Abstract
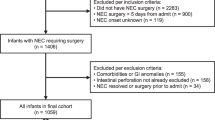
Necrotizing enterocolitis (NEC) in premature infants is associated with high morbidity and mortality, and the optimal intervention remains uncertain. To compare the mortality of primary peritoneal drainage versus primary peritoneal laparotomy as initial surgical intervention for NEC. All data were extracted from PubMed, Embase, and the Cochrane Library. Studies published up to December 2021. Patients with NEC. Studies centered on primary peritoneal drainage and primary peritoneal laparotomy as the initial surgical treatment. Mortality outcomes were available for both interventions. Randomized controlled trials, retrospective cohort studies, and case series in peer-reviewed journals. Language limited to English. Odds ratio (OR) with 95% confidence intervals (CIs) was used to evaluate mortality outcome. Subgroup analyses and linear regression were performed to ascertain the association between mortality pre-specified factors. Data of 1062 patients received peritoneal drainage and 2185 patients received peritoneal laparotomy from five case series, five retrospective cohort studies, and three randomized controlled trials. Peritoneal drainage caused similar mortality (OR 1.49, 95% CI 0.99–2.26) compared with peritoneal laparotomy as initial surgical management for NEC infants. The subgroup analysis of study design, sample size, birth weight, and sex showed similar findings, but inconsistent results were found for country (USA: 1.47, 95% CI 0.90–2.41; Canada: 2.53, 95% CI 0.30–21.48; Australia: 10.29, 95% CI 1.03–102.75; Turkey: 0.09, 95% CI 0.01–0.63) and gestational age (age mean difference < 3: 1.23, 95% CI 0.72–2.11; age mean difference ≥ 3: 2.29, 95% CI 1.04–5.05). No statistically significance was found for the linear regression between mortality and sample size (P = 0.842), gestational age (P = 0.287), birth weight (P = 0.257), sex (P = 0.6). Small sample size, high heterogeneity, NEC, and spontaneous intestinal perforation (SIP) had to be analyzed together, lack of selection criteria for the future selection of an intervention, and no clear, standardized procedures.
Conclusion: There was no significant difference in mortality between peritoneal drainage and laparotomy as initial surgical intervention. The results suggest that either intervention could be used in selected patients.
What is Known: • Necrotizing enterocolitis (NEC) in premature infants is associated with high morbidity and mortality, and the optimal intervention remains uncertain. | |
What is New: • No significant difference of mortality between peritoneal drainage and laparotomy as initial surgical intervention. |




Similar content being viewed by others
Data availability
Since it is a meta-analysis, all data were extracted from public database, then all data were available.
Abbreviations
- CIs:
-
Confidence intervals
- NEC:
-
Necrotizing enterocolitis
- OR:
-
Odds ratio
- SIP:
-
Spontaneous intestinal perforation
References
Lawrence G, Bates J, Gaul A (1982) Pathogenesis of neonatal necrotising enterocolitis. Lancet 1:137–139
Henry MC, Moss RL (2009) Necrotizing enterocolitis. Annu Rev Med 60:111–124
Rich BS, Dolgin SE (2017) Necrotizing enterocolitis. Pediatr Rev 38:552–559
Jones IH, Hall NJ (2020) Contemporary outcomes for infants with necrotizing enterocolitis-a systematic review. J Pediatr 220:86–92 e83
Braun D, Braun E, Chiu V, Burgos AE, Gupta M, Volodarskiy M, Getahun D (2020) Trends in neonatal intensive care unit utilization in a large integrated health care system. JAMA Netw Open 3:e205239
Cuttini M, Forcella E, Rodrigues C, Draper ES, Martins AF, Laine A, Willars J, Hasselager A, Maier RF, Croci I, Bonet M, Zeitlin J (2020) What drives change in neonatal intensive care units? A qualitative study with physicians and nurses in six European countries. Pediatr Res 88:257–264
Nino DF, Sodhi CP, Hackam DJ (2016) Necrotizing enterocolitis: new insights into pathogenesis and mechanisms. Nat Rev Gastroenterol Hepatol 13:590–600
Neu J, Walker WA (2011) Necrotizing enterocolitis. N Engl J Med 364:255–264
Denning TL, Bhatia AM, Kane AF, Patel RM, Denning PW (2017) Pathogenesis of NEC: role of the innate and adaptive immune response. Semin Perinatol 41:15–28
Neu J, Pammi M (2017) Pathogenesis of NEC: Impact of an altered intestinal microbiome. Semin Perinatol 41:29–35
Tanner SM, Berryhill TF, Ellenburg JL, Jilling T, Cleveland DS, Lorenz RG, Martin CA (2015) Pathogenesis of necrotizing enterocolitis: modeling the innate immune response. Am J Pathol 185:4–16
Rose AT, Patel RM (2018) A critical analysis of risk factors for necrotizing enterocolitis. Semin Fetal Neonatal Med 23:374–379
Samuels N, van de Graaf RA, de Jonge RCJ, Reiss IKM, Vermeulen MJ (2017) Risk factors for necrotizing enterocolitis in neonates: a systematic review of prognostic studies. BMC Pediatr 17:105
Cotten CM (2019) Modifiable risk factors in necrotizing enterocolitis. Clin Perinatol 46:129–143
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, Poole WK, Blakely ML, Wright L, Higgins R, Network NNR (2005) Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 115:696–703
Zhou Q, Nino DF, Yamaguchi Y, Wang S, Fulton WB, Jia H, Lu P, Prindle T, Jr., Pamies D, Morris M, Chen LL, Sodhi CP, Hackam DJ (2021) Necrotizing enterocolitis induces T lymphocyte-mediated injury in the developing mammalian brain. Sci Transl Med 13
Moschopoulos C, Kratimenos P, Koutroulis I, Shah BV, Mowes A, Bhandari V (2018) The neurodevelopmental perspective of surgical necrotizing enterocolitis: the role of the gut-brain axis. Mediators Inflamm 2018:7456857
Hong CR, Han SM, Jaksic T (2018) Surgical considerations for neonates with necrotizing enterocolitis. Semin Fetal Neonatal Med 23:420–425
Ahle S, Badru F, Damle R, Osei H, Munoz-Abraham AS, Bajinting A, Barbian ME, Bhatia AM, Gingalewski C, Greenspon J, Hamilton N, Stitelman D, Strand M, Warner BW, Villalona GA (2020) Multicenter retrospective comparison of spontaneous intestinal perforation outcomes between primary peritoneal drain and primary laparotomy. J Pediatr Surg 55:1270–1275
Rao SC, Basani L, Simmer K, Samnakay N, Deshpande G (2011) Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Database Syst Rev CD006182
Rakshasbhuvankar A, Rao S, Minutillo C, Gollow I, Kolar S (2012) Peritoneal drainage versus laparotomy for perforated necrotising enterocolitis or spontaneous intestinal perforation: a retrospective cohort study. J Paediatr Child Health 48:228–234
Yanowitz TD, Sullivan KM, Piazza AJ, Brozanski B, Zaniletti I, Sharma J, DiGeronimo R, Nayak SP, Wadhawan R, Reber KM, Murthy K, Group CSNF (2019) Does the initial surgery for necrotizing enterocolitis matter? Comparative outcomes for laparotomy vs. peritoneal drain as initial surgery for necrotizing enterocolitis in infants <1000g birth weight. J Pediatr Surg 54:712–717
van Heesewijk AE, Rush ML, Schmidt B, Kirpalani H, DeMauro SB (2020) Agreement between study designs: a systematic review comparing observational studies and randomized trials of surgical treatments for necrotizing enterocolitis. J Matern Fetal Neonatal Med 33:1965–1973
Moss RL, Dimmitt RA, Barnhart DC, Sylvester KG, Brown RL, Powell DM, Islam S, Langer JC, Sato TT, Brandt ML, Lee H, Blakely ML, Lazar EL, Hirschl RB, Kenney BD, Hackam DJ, Zelterman D, Silverman BL (2006) Laparotomy versus peritoneal drainage for necrotizing enterocolitis and perforation. N Engl J Med 354:2225–2234
Rees CM, Eaton S, Kiely EM, Wade AM, McHugh K, Pierro A (2008) Peritoneal drainage or laparotomy for neonatal bowel perforation? A randomized controlled trial. Ann Surg 248:44–51
Grave GD, Nelson SA, Walker WA, Moss RL, Dvorak B, Hamilton FA, Higgins R, Raju TN (2007) New therapies and preventive approaches for necrotizing enterocolitis: report of a research planning workshop. Pediatr Res 62:510–514
Rees CM, Eaton S, Khoo AK, Kiely EM, Members of NETTG, Pierro A (2010) Peritoneal drainage does not stabilize extremely low birth weight infants with perforated bowel: data from the NET Trial. J Pediatr Surg 45:324–328; discussion 328–329
Sola JE, Tepas JJ 3rd, Koniaris LG (2010) Peritoneal drainage versus laparotomy for necrotizing enterocolitis and intestinal perforation: a meta-analysis. J Surg Res 161:95–100
Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK, Poole WK, Jobe AH, Wright LL, Higgins RD, Network NNR (2006) Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics 117:e680-687
Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT (2020) Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 7:7
Ahmed T, Ein S, Moore A (1998) The role of peritoneal drains in treatment of perforated necrotizing enterocolitis: recommendations from recent experience. J Pediatr Surg 33:1468–1470
Azarow KS, Ein SH, Shandling B, Wesson D, Superina R, Filler RM (1997) Laparotomy or drain for perforated necrotizing enterocolitis: who gets what and why? Pediatr Surg Int 12:137–139
Dimmitt RA, Meier AH, Skarsgard ED, Halamek LP, Smith BM, Moss RL (2000) Salvage laparotomy for failure of peritoneal drainage in necrotizing enterocolitis in infants with extremely low birth weight. J Pediatr Surg 35:856–859
Morgan LJ, Shochat SJ, Hartman GE (1994) Peritoneal drainage as primary management of perforated NEC in the very low birth weight infant. J Pediatr Surg 29:310–314; discussion 314–315
Zenciroglu A, Cakmak O, Demirel N, Bas AY, Yilmaz D, Karaman I, Erdogan D (2005) Outcome of primary peritoneal drainage for perforated necrotizing enterocolitis: comparison between laparotomy and drainage. Eur J Pediatr Surg 15:243–247
Kelleher J, Mallick H, Soltau TD, Harmon CM, Dimmitt RA (2013) Mortality and intestinal failure in surgical necrotizing enterocolitis. J Pediatr Surg 48:568–572
Stey A, Barnert ES, Tseng CH, Keeler E, Needleman J, Leng M, Kelley-Quon LI, Shew SB (2015) Outcomes and costs of surgical treatments of necrotizing enterocolitis. Pediatrics 135:e1190-1197
Tashiro J, Wagenaar AE, Perez EA, Sola JE (2017) Peritoneal drainage is associated with higher survival rates for necrotizing enterocolitis in premature, extremely low birth weight infants. J Surg Res 218:132–138
Blakely ML, Tyson JE, Lally KP, Hintz SR, Eggleston B, Stevenson DK, Besner GE et al (2021) Initial laparotomy versus peritoneal drainage in extremely low birthweight infants with surgical necrotizing enterocolitis or isolated intestinal perforation: a multicenter randomized clinical trial. Ann Surg 274:e370–e380
Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, Sanchez PJ, Shankaran S, Van Meurs KP, Ball MB, Hale EC, Newman NS, Das A, Higgins RD, Stoll BJ, Eunice Kennedy Shriver National Institute of Child H, Human Development Neonatal Research N (2015) Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med 372:331–340
Ahle M, Drott P, Andersson RE (2013) Epidemiology and trends of necrotizing enterocolitis in Sweden: 1987–2009. Pediatrics 132:e443-451
Frost BL, Modi BP, Jaksic T, Caplan MS (2017) New medical and surgical insights into neonatal necrotizing enterocolitis: a review. JAMA Pediatr 171:83–88
Stoll BJ (1994) Epidemiology of necrotizing enterocolitis. Clin Perinatol 21:205–218
Mintz AC, Applebaum H (1993) Focal gastrointestinal perforations not associated with necrotizing enterocolitis in very low birth weight neonates. J Pediatr Surg 28:857–860
Han SM, Hong CR, Knell J, Edwards EM, Morrow KA, Soll RF, Modi BP, Horbar JD, Jaksic T (2020) Trends in incidence and outcomes of necrotizing enterocolitis over the last 12years: a multicenter cohort analysis. J Pediatr Surg 55:998–1001
Loepke AW, Soriano SG (2008) An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg 106:1681–1707
Author information
Authors and Affiliations
Contributions
Wei Li and Jie Tang carried out the studies, participated in collecting data, and drafted the manuscript. Wei Li and Zhongxian Zhu performed the statistical analysis and participated in its design. Jie Tang and Zhongxian Zhu helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, W., Tang, J., Zhu, Z. et al. Initial surgical treatment of necrotizing enterocolitis: a meta-analysis of peritoneal drainage versus laparotomy. Eur J Pediatr 181, 2593–2601 (2022). https://doi.org/10.1007/s00431-022-04454-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04454-3