Abstract
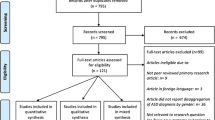
This study aims to provide an up-to-date meta-analysis of data from studies investigating the risk of bearing a child with autism spectrum disorder (ASD) after being conceived by assisted reproductive technology (ART). The study was conducted according to the PRISMA Statement. PubMed and Scopus databases were searched up to August 2, 2020. Observational studies using a type of conception of assisted reproductive technology and examined as outcome offspring with ASD were included. A random effect model was applied due to the heterogeneity of the studies. Statistical analysis was performed with Stata 13 software. The Newcastle–Ottawa scale was used to assess the methodological quality of the included studies. The search strategy identified 587 potentially relevant studies. A total of 15 studies provided adequate data for statistical comparisons and, therefore, were included in the meta-analysis. Analysis of the subset of studies that examined all offspring and controlled for confounder factors revealed that the use of ART is associated with a higher risk of ASD (RR = 1.11, 95% CI = 1.03–1.19, p < 0.009), while in the case of studies that focused on singletons, a statistically significant association between ART and ASD was not observed (RR = 0.96, 95% CI = 0.82–1.13, p = 0.654).
Conclusion: The present meta-analysis confirmed the existing positive correlation between ART and ASD in offspring, suggesting that ART is correlated with a higher risk for bearing a child with ASD. In contrast, this relationship is not confirmed in singletons. High quality prospective studies with a larger number of participants are still required.
What is Known: • Studies that investigated the association between ART and ASD in offspring have shown conflicting results. • A previous meta-analysis showed that offspring conceived by ART are 1.35 times more likely to develop ASD than offspring spontaneously conceived. | |
What is New: • This investigation separately considered studies with and without adjustment for confounders. • The findings from the two analyses were similar. |







Similar content being viewed by others
Abbreviations
- ART:
-
Assisted reproductive technology
- ASD:
-
Autism spectrum disorder
- ICSI:
-
Intracytoplasmic sperm injection
- LBW:
-
Low birth weight
- MAR:
-
Medically assisted reproduction
- NOS:
-
Newcastle-Ottawa Scale
References
Masi A, DeMayo MM, Glozier N, Guastella AJ. An overview of autism spectrum disorder, heterogeneity and treatment options. Neurosci Bull [Internet]. 2017 Apr 17;33(2):183–93. Available from: https://doi.org/10.1007/s12264-017-0100-y
Autism spectrum disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. Fifth. Washington DC: American Psychiatric Association; 2013. p. 50–9.
Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. The epidemiology of autism spectrum.
Data & statistics on autism spectrum disorder | CDC [Internet]. [cited 2020 Aug 23]. Available from: https://www.cdc.gov/ncbddd/autism/data.html
Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, et al. Genetic heritabilty. Arch Gen Psychiatry. 2011;68(11):1095–102.
Landrigan PJ. What causes autism? Exploring the environmental contribution. Curr Opin Pediatr. 2010 Apr;22(2):219–25.
Germain ARD levine susan hanson maureen. 乳鼠心肌提取 HHS Public Access. Physiol Behav. 2017;176(3):139–48.
Froehlich-Santino W, Londono Tobon A, Cleveland S, Torres A, Phillips J, Cohen B, et al. Prenatal and perinatal risk factors in a twin study of autism spectrum disorders. J Psychiatr Res [Internet]. 2014;54(1):100–8. https://doi.org/10.1016/j.jpsychires.2014.03.019
Rao SC. Prevalence of autism spectrum disorder in preterm infants : a meta-analysis. 2017;142(3).
Jenabi E, Karami M, Khazaei S, Bashirian S. The association between preeclampsia and autism spectrum disorders among children : a meta-analysis. 2019;126–30.
Gardener H, Spiegelman D, Buka SL. Perinatal and neonatal risk factors for autism : a comprehensive meta-analysis. 2011;344–55.
Wu S, Wu F, Ding Y, Hou J, Bi J, Zhang Z. Advanced parental age and autism risk in children: a systematic review and meta-analysis. Acta Psychiatr Scand [Internet]. 2017 Jan;135(1):29–41. Available from: https://doi.org/10.1111/acps.12666
Davidovitch M, Chodick G, Shalev V, Eisenberg VH, Dan U, Reichenberg A, et al. Infertility treatments during pregnancy and the risk of autism spectrum disorder in the offspring. Prog Neuro-Psychopharmacology Biol Psychiatry [Internet]. 2018 Aug;86(May):175–9. Available from: https://doi.org/10.1016/j.pnpbp.2018.05.022
Grether JK, Qian Y, Croughan MS, Wu YW, Schembri M, Camarano L, et al. Is infertility associated with childhood autism? J Autism Dev Disord [Internet]. 2013 Mar 10;43(3):663–72. Available from: https://doi.org/10.1007/s10803-012-1598-5
Schieve LA, Drews-Botsch C, Harris S, Newschaffer C, Daniels J, DiGuiseppi C, et al. Maternal and paternal infertility disorders and treatments and autism spectrum disorder: findings from the study to explore early development. J Autism Dev Disord. 2017;47(12):3994–4005.
Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem [Internet]. 2018 Dec;62(March):2–10. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0009912018302200
Care OP. C ommittee opinion. Am Coll Obstet Gynecol WOMEN’S Heal CARE PHYSICIAN. 2016;128(666):6.
Assisted Reproductive Technology (ART) | Reproductive health | CDC [Internet]. [cited 2020 Aug 23]. Available from: https://www.cdc.gov/art/index.html
Adamson D, Baker V. Multiple births from assisted reproductive technologies: a challenge that must be met. Fertil Steril [Internet]. 2004 Mar;81(3):517–22. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0015028203030668
McDonald SD, Han Z, Mulla S, Murphy KE, Beyene J, Ohlsson A. Preterm birth and low birth weight among in vitro fertilization singletons: a systematic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol [Internet]. 2009 Oct;146(2):138–48. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0301211509003753
Sandin S, Hultman C, Reichenberg A. Autism in children born after in vitro fertilization—reply. JAMA [Internet]. 2013 Nov 20;310(19):2101. Available from: https://doi.org/10.1001/jama.2013.278610
Hvidtjørn D, Grove J, Schendel D, Schieve LA, Sværke C, Ernst E, et al. Risk of autism spectrum disorders in children born after assisted conception: a population-based follow-up study. J Epidemiol Community Health. 2011;65(6):497–502.
Klemetti R, Sevóna T, Gissler M, Hemminki E. Health of children born as a result of in vitro fertilization. Pediatrics. 2006;118(5):1819–27.
Maimburg RD, Vaeth M. Do children born after assisted conception have less risk of developing infantile autism? Hum Reprod [Internet]. 2007 Jul 1;22(7):1841–3. Available from: https://doi.org/10.1093/humrep/dem082
Conti E, Mazzotti S, Calderoni S, Saviozzi I, Guzzetta A. Are children born after assisted reproductive technology at increased risk of autism spectrum disorders? A systematic review. Hum Reprod. 2013;28(12):3316–27.
Liu L, Gao J, He X, Cai Y, Wang L, Fan X. Association between assisted reproductive technology and the risk of autism spectrum disorders in the offspring: a meta-analysis. Sci Rep [Internet]. 2017 May 7;7(1):46207. https://doi.org/10.1038/srep46207
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med [Internet]. 2009 Jul 21;6(7):e1000097. Available from: https://doi.org/10.1371/journal.pmed.1000097
Ottawa Hospital Research Institute [Internet]. [cited 2020 Oct 6]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Walter S. Choice of effect measure for epidemiological data. J Clin Epidemiol [Internet]. 2000 Sep;53(9):931–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0895435600002109
Sterne JAC, Bradburn MJ, Egger M. Meta-analysis in StataTM. Syst Rev Heal Care Meta-Analysis Context Second Ed. 2008;347–69.
Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc [Internet]. 2015 Sep;13(3):196–207. Available from: http://journals.lww.com/01787381-201509000-00012
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med [Internet]. 2002 Jun 15;21(11):1539–58. Available from: https://doi.org/10.1002/sim.1186
Anzures-Cabrera J, Higgins JPT. Graphical displays for meta-analysis: an overview with suggestions for practice. Res Synth Methods [Internet]. 2010 Jan;1(1):66–80. Available from: https://doi.org/10.1002/jrsm.6
Series CB. Cochrane handbook for systematic reviews of interventions [Internet]. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane handbook for systematic reviews of interventions. Wiley; 2019. Available from: https://doi.org/10.1002/9781119536604
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ [Internet]. 1997 Sep 13;315(7109):629–34. Available from: https://doi.org/10.1136/bmj.315.7109.629
Publication ASP. Stata Meta-Analysis Reference Manual.
Diop H, Cabral H, Gopal D, Cui X, Stern JE, Kotelchuck M. Early autism spectrum disorders in children born to fertile, subfertile, and ART-treated women. Matern Child Health J [Internet]. 2019;23(11):1489–99. Available from: https://doi.org/10.1007/s10995-019-02770-z
Fountain C, Zhang Y, Kissin DM, Schieve LA, Jamieson DJ, Rice C, et al. Association between assisted reproductive technology conception and autism in California, 1997-2007. Am J Public Health. 2015;105(5):963–71.
Kamowski-Shakibai MT, Magaldi N, Kollia B. Parent-reported use of assisted reproduction technology, infertility, and incidence of autism spectrum disorders. Res Autism Spectr Disord [Internet]. 2015;9:77–95. Available from: https://doi.org/10.1016/j.rasd.2014.10.009
Lehti V, Brown AS, Gissler M, Rihko M, Suominen A, Sourander A. Autism spectrum disorders in IVF children: a national case-control study in Finland. Hum Reprod. 2013;28(3):812–8.
Lyall K, Pauls DL, Spiegelman D, Santangelo SL, Ascherio A. Fertility therapies, infertility and autism spectrum disorders in the Nurses’ Health Study II. Paediatr Perinat Epidemiol. 2012;26(4):361–72.
ÖZBARAN B, KÖSE S, AKYOL ARDIÇ Ü, ERERMİŞ S, KESIKÇI ERGİN H, BİLDİK T, et al. Yardımcı Üreme Teknikleriyle Doğmuş Çocukların ve Annelerinin Psikiyatrik Değerlendirmesi: Klinik Bir Çalışma. Nöro Psikiyatr Arşivi [Internet]. 2013 Mar 5;50(1):59–64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15891417
Shimada T, Kitamoto A, Todokoro A, Ishii-Takahashi A, Kuwabara H, Kim S-Y, et al. Parental age and assisted reproductive technology in autism spectrum disorders, attention deficit hyperactivity disorder, and Tourette syndrome in a Japanese population. Res Autism Spectr Disord [Internet]. 2012 Jan;6(1):500–7. Available from: https://doi.org/10.1016/j.rasd.2011.07.010
Svahn MF, Hargreave M, Nielsen TSS, Plessen KJ, Jensen SM, Kjaer SK, et al. Mental disorders in childhood and young adulthood among children born to women with fertility problems. Hum Reprod. 2015;30(9):2129–37.
Zachor DA, Ben Itzchak E. Assisted reproductive technology and risk for autism spectrum disorder. Res Dev Disabil [Internet]. 2011;32(6):2950–6. Available from: https://doi.org/10.1016/j.ridd.2011.05.007
Jenabi E, Seyedi M, Hamzehei R, Bashirian S, Rezaei M, Razjouyan K, et al. Association between assisted reproductive technology and autism spectrum disorders in Iran: a case-control study. Clin Exp Pediatr [Internet]. 2020 Sep 15;63(9):368–72. Available from: https://doi.org/10.3345/cep.2020.00073
Pisarska MD, Chan JL, Lawrenson K, Gonzalez TL, Wang ET. Genetics and epigenetics of infertility and treatments on outcomes. J Clin Endocrinol Metab [Internet]. 2019 Jun 1;104(6):1871–86. Available from: https://academic.oup.com/jcem/article/104/6/1871/5245823
Janeczko D, Hołowczuk M, Orzeł A, Klatka B, Semczuk A. Paternal age is affected by genetic abnormalities, perinatal complications and mental health of the offspring (Review). Biomed Reports [Internet]. 2019 Dec 20;12(3):83–8. Available from: https://doi.org/10.3892/br.2019.1266
Das L, Parbin S, Pradhan N, Kausar C, Patra SK. Epigenetics of reproductive infertility. Front Biosci - Sch. 2017;9(4):509–35.
Fett-Conte AC, Bossolani-Martins AL, Rosan DBA. Etiology of autism the complexity of risk factors in autism spectrum disorder. In: Autism spectrum disorder - recent advances [Internet]. InTech; 2015. Available from: http://www.intechopen.com/books/autism-spectrum-disorder-recent-advances/etiology-of-autism-the-complexity-of-risk-factors-in-autism-spectrum-disorder
Loke YJ, Hannan AJ, Craig JM. The role of epigenetic change in autism spectrum disorders. Front Neurol. 2015;6(MAY):1–18.
Deangelis AM, Martini AE, Owen CM. Assisted reproductive technology and epigenetics. Semin Reprod Med. 2018;36(3–4):221–32.
Hiura H, Okae H, Chiba H, Miyauchi N, Sato F, Sato A, et al. Imprinting methylation errors in ART. Reprod Med Biol [Internet]. 2014 Oct;13(4):193–202. Available from: https://doi.org/10.1007/s12522-014-0183-3
Chen W, Peng Y, Ma X, Kong S, Tang S, Zhao Y, et al. Epigenetic effects of assisted reproductive technology in human offspring 1 2. Available from: https://doi.org/10.1101/816157
Horsthemke B, Ludwig M. Assisted reproduction: the epigenetic perspective. Hum Reprod Update [Internet]. 2005 Oct 1;11(5):473–82. Available from: http://academic.oup.com/humupd/article/11/5/473/606511/Assisted-reproduction-the-epigenetic-perspective
Whitelaw N, Bhattacharya S, Hoad G, Horgan GW, Hamilton M, Haggarty P. Epigenetic status in the offspring of spontaneous and assisted conception. Hum Reprod [Internet]. 2014 Jul 1;29(7):1452–8. Available from: https://doi.org/10.1093/humrep/deu094
Author information
Authors and Affiliations
Contributions
MTA: conceived the study, participated in its design, collection, and interpretation of the data; she also performed the data collection and extraction, as well as the statistical analyses, and helped draft the manuscript. GNK: contributed to the data collection and extraction, in the analysis of the results, and in drafting the manuscript. PT: contributed to the data collection and extraction, as well as in the analysis of the results. CD: participated in the manuscript’s design and coordination. EZ: participated in the manuscript’s design and coordination. IS: participated in the manuscript’s design and coordination. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All analyses were based on previous published studies; thus, no ethical approval was required.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Paolo Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The search string that we used to Pubmed was: (((((in vitro fertilization[MeSH Terms]) OR (fertilization[MeSH Terms])) OR (infertility[MeSH Terms])) OR (assisted reproduction technologies[MeSH Terms])) OR (intracytoplasmic sperm injection[MeSH Terms]) AND ((humans[Filter]) AND (English [Filter]))) AND (((((autism[MeSH Terms]) OR (autistic[MeSH Terms])) OR (asperger syndrome[MeSH Terms])) OR (rett syndrome[MeSH Terms])) OR (developmental disorder[MeSH Terms]) AND ((humans[Filter]) AND (English [Filter]))). The search string that was applied to Scopus database was: ( ( TITLE-ABS-KEY ( in AND vitro AND fertilization) OR TITLE-ABS-KEY ( fertilization) OR TITLE-ABS-KEY ( infertility) OR TITLE-ABS-KEY ( assisted AND reproduction AND technologies) OR TITLE-ABS-KEY ( intracytoplasmic AND sperm AND injection))) AND ( ( TITLE-ABS-KEY ( autism) OR TITLE-ABS-KEY ( autistic) OR TITLE-ABS-KEY ( asperger AND syndrome) OR TITLE-ABS-KEY ( rett AND syndrome) OR TITLE-ABS-KEY ( developmental AND disorder))) AND ( LIMIT-TO ( DOCTYPE, "ar")) AND ( LIMIT-TO ( LANGUAGE, "English")) AND ( EXCLUDE ( EXACTKEYWORD, "Nonhuman")).
Rights and permissions
About this article
Cite this article
Andreadou, M.T., Katsaras, G.N., Talimtzi, P. et al. Association of assisted reproductive technology with autism spectrum disorder in the offspring: an updated systematic review and meta-analysis. Eur J Pediatr 180, 2741–2755 (2021). https://doi.org/10.1007/s00431-021-04187-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04187-9