Abstract
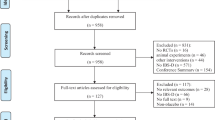
Functional abdominal pain is a very frequent functional gastrointestinal disorder but still without adequate treatment options. Therefore, the main aim of this systematic review and meta-analysis was to evaluate strain-specific probiotic effects on functional abdominal pain in children. This was a systematic review and meta-analysis of randomized controlled trials published in a period up to 1st of April 2020 that analyzed probiotic interventions for pediatric functional abdominal pain. We included 9 randomized controlled trials (a total of 702 children, 506 with functional abdominal pain; 4 to 18 years); 8 studies were available for meta-analysis (a total of 641 children). Lactobacillus rhamnosus GG and Lactobacillus reuteri DSM 17938 were the only two probiotic strains investigated. Significant reduction in pain intensity (6 trials, n = 380, mean difference − 1.24, 95% CI − 2.35 to − 0.13) and increase in number of days without pain (2 trials, n = 101, mean difference 26.42, 95% CI 22.67 to 30.17) were found in children taking L. reuteri DSM 17938. For all other outcomes, there were no significant differences between probiotic and placebo.
Conclusion: Based on the available evidence, no firm conclusions can be given; however, L. reuteri was proven to decrease the pain intensity in children with functional abdominal pain. Further trials regarding long-term outcomes, possibly involving longer interventions, are needed.
What is Known: • Previously published systematic reviews have suggested that probiotics may have an effect on the pain in children with functional gastrointestinal disorders, but limited data exist on strain-specific effects. What is New: • This systematic review provides evidence on the probiotic use on the strain-specific level. • This systematic review showed that the use of Lactobacillus reuteri DSM 17938 modestly reduces the pain intensity in children with functional abdominal pain. |





Similar content being viewed by others
Abbreviations
- LGG:
-
Lactobacillus rhamnosus GG
- FAP:
-
Functional abdominal pain
- RCT:
-
Randomized controlled trials
- FGID:
-
Functional gastrointestinal disorders
- IBS:
-
Irritable bowel syndrome
- SD:
-
Standard deviations
- CI:
-
Confidence interval
- MD:
-
Mean difference
References
Korterink JJ, Diederen K, Benninga MA, Tabbers MM (2015) Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One 10(5):e0126982. https://doi.org/10.1371/journal.pone.0126982
Spee LA, Lisman-Van Leeuwen Y, Benninga MA, Bierma-Zeinstra SM, Berger MY (2013) Prevalence, characteristics, and management of childhood functional abdominal pain in general practice. Scand J Prim Health Care 31(4):197–202. https://doi.org/10.3109/02813432.2013.844405
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M (2016) Functional disorders: children and adolescents. Gastroenterology 130(5):1527–1537. https://doi.org/10.1053/j.gastro.2016.02.015
Youssef NN, Murphy TG, Langseder AL, Rosh JR (2006) Quality of life for children with functional abdominal pain: a comparison study of patients’ and parents’ perceptions. Pediatrics 117(1):54–59. https://doi.org/10.1542/peds.2005-0114
Assa A, Ish-Tov A, Rinawi F, Shamir R (2015) School attendance in children with functional abdominal pain and inflammatory bowel diseases. J Pediatr Gastroenterol Nutr 61(5):553–557. https://doi.org/10.1097/MPG.0000000000000850
Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Whear RS, Thompson Coon J, Logan S (2018) Recurrent abdominal pain in children: summary evidence from 3 systematic reviews of treatment effectiveness. J Pediatr Gastroenterol Nutr 67(1):23–33. https://doi.org/10.1097/MPG.0000000000001922
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S, Calder PC, Sanders ME (2014) Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11(8):506–514. https://doi.org/10.1038/nrgastro.2014.66
Pourmirzaiee MA, Famouri F, Moazeni W, Hassanzadeh A, Hajihashemi M (2020) The efficacy of the prenatal administration of Lactobacillus reuteri LR92 DSM 26866 on the prevention of infantile colic: a randomized control trial. Eur J Pediatr Published ahead of print 179:1619–1626. https://doi.org/10.1007/s00431-020-03641-4
Fang HR, Zhang GQ, Cheng JY, Li ZY (2019) Efficacy of Lactobacillus-supplemented triple therapy for Helicobacter pylori infection in children: a meta-analysis of randomized controlled trials. Eur J Pediatr 178(1):7–16. https://doi.org/10.1007/s00431-018-3282-z
Gareau MG, Sherman PM, Walker WA (2010) Probiotics and the gut microbiota in intestinal health and disease. Nat Rev Gastroenterol Hepatol 7(9):503–514. https://doi.org/10.1038/nrgastro.2010.117
Newlove-Delgado TV, Martin AE, Abbott RA, Bethel A, Thompson-Coon J, Whear R, Logan S (2017) Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev 3:CD010972. https://doi.org/10.1002/14651858.CD010972.pub2
Horvath A, Dziechciarz P, Szajewska H (2011) Meta-analysis: Lactobacillus rhamnosus GG for abdominal pain-related functional gastrointestinal disorders in childhood. Aliment Pharmacol Ther 33(12):1302–1310. https://doi.org/10.1111/j.1365-2036.2011.04665.x
Korterink JJ, Ockeloen L, Benninga MA, Tabbers MM, Hilbink M, Deckers-Kocken JM (2014) Probiotics for childhood functional gastrointestinal disorders: a systematic review and meta-analysis. Acta Paediatr 103(4):365–372. https://doi.org/10.1111/apa.12513
Rutten JM, Korterink JJ, Venmans LM, Benninga MA, Tabbers MM (2015) Nonpharmacologic treatment of functional abdominal pain disorders: a systematic review. Pediatrics 135(3):522–535. https://doi.org/10.1542/peds.2014-2123
Wegh CAM, Benninga MA, Tabbers MM (2018) Effectiveness of probiotics in children with functional abdominal pain disorders and functional constipation: a systematic review. J Clin Gastroenterol 52 Suppl 1, Proceedings from the 9th Probiotics, Prebiotics and New Foods, Nutraceuticals and Botanicals for Nutrition & Human and Microbiota Health Meeting, held in Rome, Italy from September 10 to 12, 2017:S10-S26. doi:https://doi.org/10.1097/MCG.0000000000001054
Ding FCL, Karkhaneh M, Zorzela L, Jou H, Vohra S (2019) Probiotics for paediatric functional abdominal pain disorders: a rapid review. Paediatr Child Health 24(6):383–394. https://doi.org/10.1093/pch/pxz036
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ WV. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane, 2019. Handbook. 2019. p. Available from www.training.cochrane.org/handbook
Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, Walker LS (2006) Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130(5):1527–1537. https://doi.org/10.1053/j.gastro.2005.08.063
Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, Staiano A (1999) Childhood functional gastrointestinal disorders. Gut 45(Suppl 2):II60–II68. https://doi.org/10.1136/gut.45.2008.ii60
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Schünemann HBJ, Guyatt G, Oxman A Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Updated October 2013. The GRADE working group, 2013
Higgins JP, White IR, Wood AM (2008) Imputation methods for missing outcome data in meta-analysis of clinical trials. Clin Trials 5(3):225–239. https://doi.org/10.1177/1740774508091600
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Francavilla R, Miniello V, Magista AM, De Canio A, Bucci N, Gagliardi F, Lionetti E, Castellaneta S, Polimeno L, Peccarisi L, Indrio F, Cavallo L (2010) A randomized controlled trial of Lactobacillus GG in children with functional abdominal pain. Pediatrics 126(6):e1445–e1452. https://doi.org/10.1542/peds.2010-0467
Gawronska A, Dziechciarz P, Horvath A, Szajewska H (2007) A randomized double-blind placebo-controlled trial of lactobacillus GG for abdominal pain disorders in children. Aliment Pharmacol Ther 25(2):177–184. https://doi.org/10.1111/j.1365-2036.2006.03175.x
Romano C, Ferrau V, Cavataio F, Iacono G, Spina M, Lionetti E, Comisi F, Famiani A, Comito D (2014) Lactobacillus reuteri in children with functional abdominal pain (FAP). J Paediatr Child Health 50(10):E68–E71. https://doi.org/10.1111/j.1440-1754.2010.01797.x
Weizman Z, Abu-Abed J, Binsztok M (2016) Lactobacillus reuteri DSM 17938 for the management of functional abdominal pain in childhood: a randomized, double-blind, Placebo-Controlled Trial. J Pediatr 174:160–164 e161. https://doi.org/10.1016/j.jpeds.2016.04.003
Jadresin O, Hojsak I, Misak Z, Kekez AJ, Trbojevic T, Ivkovic L, Kolacek S (2017) Lactobacillus reuteri DSM 17938 in the treatment of functional abdominal pain in children: RCT study. J Pediatr Gastroenterol Nutr 64(6):925–929. https://doi.org/10.1097/MPG.0000000000001478
Eftekhari K, Vahedi Z, Kamali Aghdam M, Noemi Diaz D (2015) A randomized double-blind placebo-controlled trial of lactobacillus reuteri for chronic functional abdominal pain in children. Iran J Pediatr 25(6):e2616. https://doi.org/10.5812/ijp.2616
Maragkoudaki M, Chouliaras G, Orel R, Horvath A, Szajewska H, Papadopoulou A (2017) Lactobacillus reuteri DSM 17938 and a placebo both significantly reduced symptoms in children with functional abdominal pain. Acta Paediatr 106(11):1857–1862. https://doi.org/10.1111/apa.13992
Jadrešin O, Sila S, Trivić I, Mišak Z, Kolaček S, Hojsak I (2020) Lactobacillus reuteri DSM 17938 is effective in the treatment of functional abdominal pain in children: results of the double-blind randomized study. Clin Nutr S0261-5614(20):30190–30194
Sabbi T (2011) The use of lactobacillus GG in children with functional abdominal pain: a double-blind randomized control trial. Clin Nutr Suppl 6:198
Zeevenhooven J, Rexwinkel R, Van Berge Henegouwen VWA, Krishnan U, Vandenplas Y, Strisciuglio C, Staiano A, Devanarayana NM, Rajindrajith S, Benninga MA, Tabbers MM, Consensus Group on Outcome Measures Made in Pediatric Enteral Nutrition Clinical Trials Working G (2020) A core outcome set for clinical trials in pediatric functional abdominal pain disorders. J Pediatr 221:115–122 e115. https://doi.org/10.1016/j.jpeds.2020.02.032
Rowland M, Bourke B, Drumm B (2005) Do the Rome criteria help the doctor or the patient? J Pediatr Gastroenterol Nutr 41(Suppl 1):S32–S33. https://doi.org/10.1097/01.scs.0000180296.19978.75
Shin A, Preidis GA, Shulman R, Kashyap PC (2019) The gut microbiome in adult and pediatric functional gastrointestinal disorders. Clin Gastroenterol Hepatol 17(2):256–274. https://doi.org/10.1016/j.cgh.2018.08.054
Author information
Authors and Affiliations
Contributions
OJ and IH conceptualized and planned this systematic review and meta-analysis. IT and TN independently searched the literature. IT and TN individually collected the study details and outcome data using a predetermined form. Disagreement was resolved by discussion with IH and OJ. Risk of bias for each study was assessed individually. Analysis was done by IH and revised by IT, TN, and OJ. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Iva Hojsak received payment/honorarium for lectures or consultation from BioGaia, Nutricia, Nestle, Chr Hansen, Biocodex, Oktal Pharma; Ivana Trivić, Tena Niseteo and Oleg Jadrešin declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable for this manuscript.
Additional information
Communicated by Gregorio Paolo Milani
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 27 kb)
ESM 2
(DOCX 17 kb)

Supplemental Figure 1.
Effect of Lactobacillus reuteri DSM 17938 on a) the number of days missed from the school and b) on the number of days without pain. (PNG 341 kb)
Rights and permissions
About this article
Cite this article
Trivić, I., Niseteo, T., Jadrešin, O. et al. Use of probiotics in the treatment of functional abdominal pain in children—systematic review and meta-analysis. Eur J Pediatr 180, 339–351 (2021). https://doi.org/10.1007/s00431-020-03809-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03809-y