Abstract
Purpose
This study aimed to investigate the stability of posterior corneal surface 2 years after transepithelial photorefractive keratectomy (TPRK) in patients with a residual stromal thickness less than 350 μm.
Methods
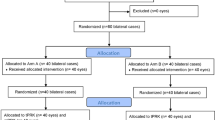
In total, 408 eyes of 212 patients (160 women, 52 men) who underwent TPRK were enrolled in this retrospective study. All surgeries were performed in the Amaris 750S excimer laser platform with smart pulse technology. The posterior corneal elevation, anterior chamber depth, Q value, and curvature were measured using Pentacam preoperatively and postoperatively. All patients were followed up for 2 years. The relationship between percent tissue altered (PTA), age, and changes in posterior corneal surface was analyzed.
Results
The mean preoperative spherical equivalent was − 6.80 ± 1.18 D (range: − 9.00 to − 2.63 D). The mean residual stromal thickness was 336.46 ± 7.25 μm (range: 310–348 μm). The mean PTA was 30.93 ± 2.03% (range: 24.29–35.28%). At 2 years after surgery, the elevation of six points in the central area decreased by 1.91 ± 2.97 μm, 2.98 ± 3.23 μm, 1.17 ± 3.85 μm, 1.70 ± 2.88 μm, 1.36 ± 3.19 μm, and 1.65 ± 3.18 μm, compared with the preoperative value (P < 0.05). The elevation of three points in the peripheral area increased by 1.87 ± 6.34 μm, 0.68 ± 6.00 μm, and 0.95 ± 5.50 μm (P < 0.05). There was no significant linear relationship between PTA, age, and changes in posterior corneal surface, anterior chamber depth, and K2 (all P > 0.05).
Conclusion
Within 2 years after TPRK, the posterior corneal surface remained stable in patients with a residual stromal thickness between 310 and 350 μm. There was no sign of iatrogenic ectasia during the follow-up period.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Faktorovich EG, Melwani K (2014) Efficacy and safety of pain relief medications after photorefractive keratectomy: review of prospective randomized trials. J Cataract Refract Surg 40:1716–1730. https://doi.org/10.1016/j.jcrs.2014.08.001
Vestergaard AH (2014) Past and present of corneal refractive surgery: a retrospective study of long-term results after photorefractive keratectomy, and a prospective study of refractive lenticule extraction. Acta Ophthalmol 92:492–493. https://doi.org/10.1111/aos.12450
Chang YM, Liang CM, Weng TH et al (2021) Mitomycin C for the prevention of corneal haze in photorefractive keratectomy: a meta-analysis and trial sequential analysis. Acta Ophthalmol 99:652–662. https://doi.org/10.1111/aos.14704
Kaiserman I, Sadi N, Mimouni M et al (2017) Corneal breakthrough haze after photorefractive keratectomy with mitomycin C: incidence and risk factors. Cornea 36:961–966. https://doi.org/10.1097/ICO.0000000000001231
Golan O, Randleman JB (2018) Pain management after photorefractive keratectomy. Curr Opin Ophthalmol 29:306–312. https://doi.org/10.1097/ICU.0000000000000486
Sanchez P, Moutsouris K, Pandolfi A (2014) Biomechanical and optical behavior of human corneas before and after photorefractive keratectomy. J Cataract Refract Surg 40:905–917. https://doi.org/10.1016/j.jcrs.2014.03.020
Shang J, Shen Y, Jhanji V et al (2021) Comparison of corneal biomechanics in post-SMILE, post-LASEK, and keratoconic eyes. Front Med (Lausanne) 8(695697):2021. https://doi.org/10.3389/fmed.2021.695697. (eCollection)
Francis M, Khamar P, Shetty R et al (2018) In vivo prediction of air-puff induced corneal deformation using LASIK, SMILE, and PRK finite element simulations. Invest Ophthalmol Vis Sci 59:5320–5328. https://doi.org/10.1167/iovs.18-2470
Guo H, Hosseini-Moghaddam SM, Hodge W (2019) Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol 19:167. https://doi.org/10.1186/s12886-019-1165-3
Moshirfar M, Tukan AN, Bundogji N et al (2021) Ectasia after corneal refractive surgery: a systematic review. Ophthalmol Ther 10:753–776. https://doi.org/10.1007/s40123-021-00383-w
Fernandes P, González-Méijome JM, Madrid-Costa D et al (2011) Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg 27:765–776. https://doi.org/10.3928/1081597X-20110617-01
Packer M (2018) The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol 12:2427–2438. https://doi.org/10.2147/OPTH.S188785
Randleman JB, Woodward M, Lynn MJ et al (2008) Risk assessment for ectasia after corneal refractive surgery. Ophthalmology 115:37–50. https://doi.org/10.1016/j.ophtha.2007.03.073
Santhiago MR, Smadja D, Gomes BF et al (2014) Association between the percent tissue altered and post-laser in situ keratomileusis ectasia in eyes with normal preoperative topography. Am J Ophthalmol 158:87–95. https://doi.org/10.1016/j.ajo.2014.04.002
Santhiago MR (2016) Percent tissue altered and corneal ectasia. Curr Opin Ophthalmol 27:311–315. https://doi.org/10.1097/ICU.0000000000000276
Giri P, Azar DT (2017) Risk profiles of ectasia after keratorefractive surgery. Curr Opin Ophthalmol 28:337–342. https://doi.org/10.1097/ICU.0000000000000383
Jin SX, Dackowski E, Chuck RS (2020) Risk factors for postlaser refractive surgery corneal ectasia. Curr Opin Ophthalmol 31:288–292. https://doi.org/10.1097/ICU.0000000000000662
Soundarya B, Sachdev GS, Ramamurthy S et al (2020) Ectasia after keratorefractive surgery: analysis of risk factors and treatment outcomes in the Indian population. Indian J Ophthalmol 68:1028–1031. https://doi.org/10.4103/ijo.IJO_1580_19
Randleman JB, Trattler WB, Stulting RD (2008) Validation of the Ectasia Risk Score System for preoperative laser in situ keratomileusis screening. Am J Ophthalmol 145:813–818. https://doi.org/10.1016/j.ajo.2007.12.033
Kim H, Choi JS, Joo CK (2006) Corneal ectasia after PRK: clinicopathologic case report. Cornea 25:845–848. https://doi.org/10.1097/01.ico.0000224634.72309.43
Randleman JB, Caster AI, Banning CS et al (2006) Corneal ectasia after photorefractive keratectomy. J Cataract Refract Surg 32:1395–1398. https://doi.org/10.1016/j.jcrs.2006.02.078
Leccisotti A (2007) Corneal ectasia after photorefractive keratectomy. Graefes Arch Clin Exp Ophthalmol 245:869–875. https://doi.org/10.1007/s00417-006-0507-z
Nishimura R, Negishi K, Saiki M et al (2007) No forward shifting of posterior corneal surface in eyes undergoing LASIK. Ophthalmology 114:1104–1110. https://doi.org/10.1016/j.ophtha.2006.09.014
Ciolino JB, Belin MW et al (2006) Changes in the posterior cornea after laser in situ keratomileusis and photorefractive keratectomy. J Cataract Refract Surg 32:1426–1431. https://doi.org/10.1016/j.jcrs.2006.03.037
Ciolino JB, Khachikian SS, Cortese MJ et al (2007) Long-term stability of the posterior cornea after laser in situ keratomileusis. J Cataract Refract Surg 33:1366–1370. https://doi.org/10.1016/j.jcrs.2007.04.016
Grewal DS, Brar GS, Grewal SP (2011) Posterior corneal elevation after LASIK with three flap techniques as measured by Pentacam. J Refract Surg 27:261–268. https://doi.org/10.3928/1081597X-20100618-01
Zhao Y, Qian Y, Chen X et al (2021) Comparison of posterior corneal elevation after SMILE and FS-LASIK in correcting myopia over 90 diopters. Ann Transl Med 9:373. https://doi.org/10.21037/atm-20-5165
Zhang L, Wang Y (2010) The shape of posterior corneal surface in normal, post-LASIK, and post-epi-LASIK eyes. Invest Ophthalmol Vis Sci 51:3468–3475. https://doi.org/10.1167/iovs.09-4811
Li M, Yang D, Zhao Y et al (2020) Impact of ablation ratio on 5-year postoperative posterior corneal stability after refractive surgery: SMILE and FS-LASIK. Eye Vis (Lond) 7:53. https://doi.org/10.1186/s40662-020-00218-y
Zhao Y, Fu D, Chen Z et al (2022) Three-year follow-up of posterior corneal elevation in thin corneas after small incision lenticule extraction. Front Med (Lausanne) 9:758223. https://doi.org/10.3389/fmed.2022.758223
Zhao Y, Jian W, Chen Y et al (2017) Three-year stability of posterior corneal elevation after small incision lenticule extraction (SMILE) for moderate and high myopia. J Refract Surg 33:84–88. https://doi.org/10.3928/1081597X-20161117-01
Dai ML, Wang QM, Lin ZS et al (2018) Posterior corneal surface differences between non-laser in situ keratomileusis (LASIK) and 10-year post-LASIK myopic eyes. Acta Ophthalmol 96:127–133. https://doi.org/10.1111/aos.13532
Yu M, Chen M, Dai J (2019) Comparison of the posterior corneal elevation and biomechanics after SMILE and LASEK for myopia: a short- and long-term observation. Graefes Arch Clin Exp Ophthalmol 257:601–606. https://doi.org/10.1007/s00417-018-04227-5
Nishimura R, Negishi K, Dogru M et al (2009) Effect of age on changes in anterior chamber depth and volume after laser in situ keratomileusis. J Cataract Refract Surg 35:1868–1872. https://doi.org/10.1016/j.jcrs.2009.06.022
Wang J, Lopes BT, Li H et al (2021) Unintended changes in ocular biometric parameters during a 6-month follow-up period after FS-LASIK and SMILE. Eye Vis (Lond) 8:9. https://doi.org/10.1186/s40662-021-00232-8
Chen Z, Zhao Y, Zhou X et al (2021) Seven-year observation of posterior corneal elevation after small-incision lenticule extraction in patients with moderate and high myopia. J Cataract Refract Surg 47:1398–1402. https://doi.org/10.1097/j.jcrs.0000000000000639
Cagini C, Messina M, Lupidi M et al (2015) Posterior corneal surface stability after femtosecond laser-assisted keratomileusis. J Ophthalmol 2015:184850. https://doi.org/10.1155/2015/184850
Sun HJ, Park JW, Kim SW (2009) Stability of the posterior corneal surface after laser surface ablation for myopia. Cornea 28:1019–1022. https://doi.org/10.1097/ICO.0b013e3181a06f1e
Wang B, Zhang Z, Naidu RK et al (2016) Comparison of the change in posterior corneal elevation and corneal biomechanical parameters after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia correction. Cont Lens Anterior Eye 39:191–196. https://doi.org/10.1016/j.clae.2016.01.007
Zhao Y, Li M, Zhao J et al (2016) Posterior corneal elevation after small incision lenticule extraction for moderate and high myopia. PLoS One 11:e0148370. https://doi.org/10.1371/journal.pone.0148370
Randleman JB, Dawson DG, Grossniklaus HE et al (2008) Depth-dependent cohesive tensile strength in human donor corneas: implications for refractive surgery. J Refract Surg 24:85–89. https://doi.org/10.3928/1081597X-20080101-15
Sorkin N, Kaiserman I, Domniz Y et al (2017) Risk assessment for corneal ectasia following photorefractive keratectomy. J Ophthalmol 2017:2434830. https://doi.org/10.1155/2017/2434830
Funding
This work was supported by the Medical and Health Development Grant of Shandong Province, China (No. 2017WS180).
Author information
Authors and Affiliations
Contributions
Study conception and design were performed by L. H., S. T., and L. K. L. Data collection was done by L. H., Z. J. F., W. H. F., L. S., and L. K. L. Analysis and interpretation of data was done by L. H., Z. J. F., and L. K. L. Writing the manuscript were performed by L. H., S. T., and L. K. L. Critical revision of the manuscript were performed by L. H., Z. J. F., W. H. F., L. S., and L. K. L. Statistical expertise were performed by L. H., Z. J. F., and S. T. Administrative, technical, or material support were performed by L. K. L. Supervision were performed by L. H. and L. K. L. All authors have reviewed the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committees of Institutional Review Boards of Qingdao Eye Hospital. All patients were adequately informed about the study as well as the risks and benefits of the surgery and provided signed informed consent to participate.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, H., Zhang, J., Shao, T. et al. Two-year stability of posterior corneal surface after transepithelial photorefractive keratectomy with a residual stromal thickness less than 350 μm. Graefes Arch Clin Exp Ophthalmol 261, 857–865 (2023). https://doi.org/10.1007/s00417-022-05814-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05814-3